ABSTRACT
The mortality rate from COVID-19 appears to be higher in solid organ transplant (SOT) recipients when compared with other populations. Vaccination is a key strategy to prevent the COVID-19 pandemic. However, it is unclear how readily SOT recipients will get vaccinated against COVID-19. We conducted an internet-based survey to investigate the vaccination willingness among Chinese SOT recipients and further explore possible influencing factors. Eight hundred and thirteen respondents participated in the survey. Overall, 46 (5.7%) recipients were vaccinated against COVID-19, while 767 (94.3%) were not. Among those not vaccinated, 175 (22.8%) intended to be vaccinated, while 592 (77.2%) were categorized as vaccine-hesitant. The most common reason for vaccination hesitancy is fear of preexisting comorbidities, followed by fear of side effects and doctors’ negative advice. Factors associated with vaccination willingness were as follows: with liver transplantation, the main source of information on COVID-19 vaccines was from medical doctors, scientists, and scientific journals, with at least college-level education, positive intention toward influenza vaccination during the current season, perceived importance of vaccination for SOT recipients, and having been vaccinated against influenza during the last season. Our survey indicated the necessity for SOT recipients to receive more comprehensive and accessible health education about vaccination and emphasized the critical role of transplantation physicians in promoting vaccine acceptance among SOT recipients. We hope that our survey results will help governments to better target communication in the ongoing COVID-19 vaccination campaign.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection results in frequent hospitalization and death among the solid organ transplant (SOT) recipients. When compared with other populations, mortality rate from coronavirus disease 2019 (COVID-19) appears to be higher in SOT recipients, attributed to the underlying immunosuppression and concomitant comorbidities.Citation1 It seems that the most promising way to prevent further spread of COVID-19 is vaccination. Therefore, achieving high vaccination coverage is crucial in the control and prevention of COVID-19 pandemic. By the middle of June 2021, more than 280 vaccine candidates against SARS-CoV-2 are in various stages of development,Citation2 and 5 SARS-CoV-2 vaccines (Sinovac, Sinopharm, Sinopharm-Wuhan, Sinopharm-Beijing, CanSino, Zhifei Long-com)Citation3 have been authorized in China for clinical setting use. At the end of March 2021, the National Health Commission of the People’s Republic of China published the first edition of COVID-19 vaccine vaccination technical guideline,Citation3 further popularize and promote the inoculation of vaccine. However, one of the major hurdles to successful COVID-19 vaccination is vaccine hesitancy (i.e. the delay in acceptance or reluctance of vaccination despite availability of vaccination services).Citation4
Several general factors have been reported as association with vaccine hesitancy, including past experience with vaccines, education level, knowledge level, risk perception and trust, subjective norms, perception about the importance of vaccination, and religious and moral convictions.Citation5 Nevertheless, vaccine hesitancy varies with time, environment and for different vaccines.Citation6 In terms of COVID-19 vaccines, additional factors may play an important role in vaccination. Firstly, the speed at which the vaccine candidates were developed and approved within less than one year, while vaccine development commonly takes years to undergo preclinical stages, phase II and phase III trials effectively. Secondly, the durability of the immune response following the vaccination and the effectiveness to limit the asymptomatic spread remains unclear, especially in the immunosuppressed individuals.Citation7 Thirdly, concern and uncertainty that companied with COVID-19 crisis raised the spread of misinformation, which extended to affect COVID-19 vaccination.Citation8
Health-care workers, students, and public populations are the main survey subjects in the existing studies on perceptions and attitudes toward COVID-19 vaccines.Citation8–13 The safety and efficacy of COVID-19 vaccines in SOT recipients are currently unknown as immunocompromised individuals were excluded in most of the clinical trials. It may be different in willingness to get vaccinated between the immunocompromised individuals and normal immunity populations. Recently, a national survey conducted by Michael et al.Citation14 reported low willingness to get vaccinated among SOT recipients. Yet, only 4.1% (n = 54) Asian recipients were included in this study. Up to now, there is as yet no survey about COVID-19 vaccination willingness among immunosuppressed individuals in China. To address this lacuna, we conducted this survey to assess COVID-19 vaccination willingness among SOT recipients in China after the COVID-19 vaccines were put into use, while the vaccination hesitancy reasons and associated factors were analyzed either.
Materials and methods
Study design and sample
An anonymous, self-designed, and structured online questionnaire was conducted in Chinese renal transplant recipients aged 18 years and above, from 12 May to 26 May 2021. The questionnaire was made available through a WeChat platform, released by the Renal Transplantation Center of Zhongshan Hospital Fudan University, and subsequently shared by the other three SOT associated WeChat platforms. A web link collector generated the survey QR code through which participants could access the survey and send their answers. For its distribution, a convenient, nonprobability sampling method was implemented. Ethical approval was granted by the Ethics Committee of Zhongshan Hospital Fudan University (No. B2021-378). Participants in the study were voluntary, and an informed consent form was included in the introductory section of the online survey. Patients who give consent to inform will perform the subsequent questionnaire. All collected data were treated with confidentiality.
Eligibility criteria
The eligibility criteria included age more than or equal to 18, with a history of SOT, and have an ability to read and understand Chinese.
Survey items
The final questionnaire comprised three sections. The first section on demographics included questions on the following: graft, age, sex, post-transplantation time, occupation, residence, educational level, marital status, history of chronic disease, having friends with medical background, previous COVID-19 diagnosis for the respondent.
The second section investigated the knowledge of the participants about COVID-19 vaccines, comprised six items: knew the first edition of COVID-19 vaccine vaccination technical guideline (yes/no), the main source of knowledge about COVID-19 vaccines (allowing the selection of a single main source out of four possible options: television and news release; social media platforms; medical doctors, scientists or scientist journals; or relatives and friends inform), recognize the importance of COVID-19 vaccination for preventing the spread of COVID-19 in the future (yes/no), recognize the importance of COVID-19 vaccination for SOT patients (yes/no).
The third section evaluated the willingness to get a COVID-19 vaccine, included following questions (): 1. Have you been vaccinated with influenza vaccine in the last influenza season (2020–2021)? (yes/no). 2. Are you willing to accept influenza vaccine in the current season (2021–2022)? (yes/no). 3. Have your family members been vaccinated against COVID-19? (yes/no). 4. Have you already been vaccinated against COVID-19? (yes/no).
Figure 1. The flow chart for the third section of the questionnaire. COVID-19 = coronavirus disease 2019; SARS-CoV-2 = Severe acute respiratory syndrome coronavirus 2; Flu = influenza.
If the answer was “yes,” data collectors asked a multiple-choice question “Do you have any adverse reactions after accept the COVID-19 vaccine? (no/sleepiness/ fatigue/pain at the injection site/fever/ allergy/others).”
If the answer was “no,” the respondents will be asked about their willingness to be vaccinated (yes/uncertain/no). If the answer was “yes,” data collectors asked about whether they will receive vaccination as soon as possible or not? (yes/wait a while). If the answer was “no” or “uncertain,” they will be asked about the reasons for hesitancy and the possible way to promote vaccine coverage were investigated.
Statistical analysis
Statistical analysis was performed using IBM SPSS 26.0 for windows. Number (n) and percentage (%) were presented for categorical variables, while quantitative variables were presented as mean (standard deviation). Chi-square tests were used for univariate analysis of qualitative variables. Variables with p < .25 in the univariate analysis were included in multiple logistic regression analysis model, in order to explore potential factors associated with vaccination hesitancy. Odds ratio (OR) and 95% confidence intervals (95% CI) were calculated. The Hosmer–Lemeshow test and Omnibus test were performed for the model fit estimation. The level of statistical significance was set at p < .050.
Results
Sample characteristics
Overall, 813 respondents from 30 provinces all over China participated in the survey between May 12 and May 26, 2021. The percentage of response was 40.0%. None of the respondents had a history of SARS-CoV-2 infection. Of these, 46 (5.7%) have accepted COVID-19 vaccine and 767 (94.3%) have not. The characteristics of these participants are shown in . Most respondents (n = 691, 85.0%) were renal transplantation recipients, and two-thirds of them were male (n = 551, 67.8%). Most respondents (n = 632, 77.7%) reported to have more than 2 years of transplantation. The urban-rural split close to 1:4 and most of the participants (n = 685, 84.3%) were aged between 30 and 60. In terms of education, 60.5% (n = 492) of the respondents had a college and above education level. Enterprise workers (n = 209, 25.7%) accounted for the highest occupational group, followed by retired/vacation staffs (n = 163, 20.1%), institution staffs (n = 131, 16.1%), and others (n = 96, 11.8%). People over half (n = 477, 58.7%) knew the first edition of COVID-19 vaccine vaccination technical guideline.
Table 1. Characteristics of the respondents for survey
We divided the respondents who have not been vaccinated into two groups, regarding their intention to be vaccinated (). When comparing COVID-19 vaccine hesitancy and not, differences (p < .05) were documented in regard to graft, educational level, history of hyperuricemia, history of other chronic diseases, intention toward influenza vaccination for current season, agree with the importance of COVID-19 vaccines for public health, agree with the importance of COVID-19 vaccines for SOT patients.
Among the participants already vaccinated, most of them (n = 34, 73.9%) self-reported no adverse reaction (ADR) after vaccinations (), 17.4% (n = 8) of them reported pain at the injection site, followed by fatigue (n = 4, 8.7%).
Attitude and practice toward vaccination against influenza and SARS-CoV-2
Only 49 (6.0%) of respondents reported that they have been vaccinated against influenza during the last influenza season (2010–2021) while, when investigating their attitude during the current season (2021–2022), 23.6% (n = 192) of them declared their willingness to get influenza vaccination ().
Instead, in terms of COVID-19 vaccination, 175 (22.8%) SOT recipients reported that they were willing to get vaccinated, while 65.6% (n = 503) declared that they still hesitate, and 89 (11.6%) respondents declared vaccine refusal. Overall, 592 (77.2%) SOT participants were categorized as vaccine-hesitant.
The vaccination willingness was evaluated among the participants have not gotten COVID-19 vaccinated, stratified by the attitude toward being vaccinated against influenza during the current season (2021–2022). The COVID-19 vaccine willingness rate was 17.3% (103/594) in the influenza vaccine refuse group, while it was 41.6% (72/173) in the influenza willingness group ().
Table 2. COVID-19 vaccine willingness rate stratified by attitude toward being vaccinated against influenza during the current season (2021–2022)
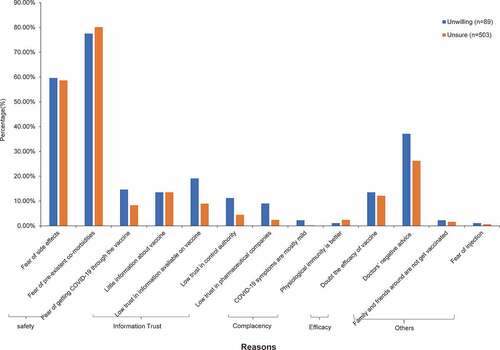
Reasons for vaccination hesitancy
The main reasons for vaccination hesitancy were analyzed from the data of the 592 respondents who were hesitant to receive the COVID-19 vaccine (). The results showed that among these respondents who were unwilling to be vaccinated, the most common reason is fear of preexisting comorbidities (n = 69, 77.5%), followed by fear of side effects (n = 53, 59.6%) and the doctors’ negative advice (n = 33, 37.1%). The main reasons for the respondents’ uncertain to be vaccinated were also the three aforementioned reasons.
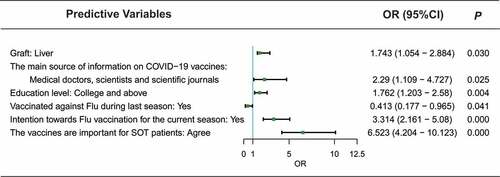
Predictors for willingness to vaccinate against COVID-19
In the multivariate logistic regression model as showed in , factors positively associated with willingness to get vaccinated in SOT patients are followings: with liver transplantation (OR = 1.743, 95% CI = 1.054–2.884), the main source of information on COVID-19 vaccines was medical doctors, scientists, and scientific journals (OR = 2.29, 95% CI = 1.109–4.727), with college and above education (OR = 1.762, 95% CI = 1.203–2.58), positive intention toward influenza vaccination during the current season (OR = 3.314, 95% CI = 2.161–5.08), perceived the importance of vaccine for SOT patients (OR = 6.523, 95% CI = 4.204–10.123). On the contrary, having been vaccinated against influenza during the last season (OR = 0.413, 95% CI = 0.177–0.965) resulted to be a factor associated with vaccination hesitancy.
Figure 3. Multiple logistic regression analysis of factors associated with willingness to vaccinate against COVID-19. COVID-19 = coronavirus disease 2019; OR = odds ratio; CI = confidence interval; Flu = influenza.
For the multiple choices question “In your opinion, which of the following initiatives would help to increase SOT participants vaccinating against SARS-CoV-2?,” the most choice is positive suggestion of transplant physicians (n = 549, 92.7%) ().
Discussion
COVID-19 vaccine is the most potential way to prevent the SARS-CoV-2 pandemic at present. By the time this survey was conducted, the Chinese government had published the first edition of COVID-19 vaccine vaccination technical guideline,Citation3 for propaganda and popularization of COVID-19 vaccine. As described in that guideline, immunocompromised individuals should get vaccinated against SARS-CoV-2. However, many SOT recipients are still concerned with receiving the COVID-19 vaccine in clinical practice. We investigated the willingness to receive COVID-19 vaccine and the associated factors in the current circumstance among Chinese SOT recipients. Our survey indicated that the vaccination rate and vaccination willingness rate were both insufficient in Chinese SOT patients. The most common reason for vaccination hesitancy is fear of preexisting comorbidities. Factors associated with vaccination willingness were as follows: transplantation organ, the main source of information on COVID-19 vaccines, education level, intention toward influenza vaccination during the current season, perception of vaccine for SOT recipients and vaccination state against influenza during last season.
A delightful result in our result was that in these respondents who were vaccinated against SARS-CoV-2, most of them (73.9%, n = 34) reported no ADR and the most reported ADR was pain at the injection site. This was in line with the discovery by Brian et al.Citation15 and Panda et al.Citation16 Among the participants willing to be vaccinated, 16% of them would prefer to postpone vaccination, maybe due to uncertainty about the efficacy and risk of COVID-19 vaccines. Overall, the vaccination hesitancy in our research was higher than the study by Michael et al.Citation14
In the study by Lazaruse et al. relatively high willingness to get vaccinated was reported (>80%) in Asian countries including China and Indonesia.Citation17 However, our result is alarming, since it was obviously lower than the recent surveys among Chinese adults, which indicated that the potential acceptance of COVID-19 vaccines ranged from 60.4% to 82.3% for free vaccine in four studies.Citation13,Citation18–20 This finding indicated difference between SOT recipients and general population in their willingness to vaccinate.
The main reason for vaccine hesitancy was fear of preexisting comorbidities (80.1%), indicated by our survey. Lack of trust in COVID-19 vaccine safety (58.6%) was the second most common reason. This was slightly different with the study conducted by Michael et al. That survey reported that major concerns included potential side effects (85.2%), and fear of incompatibility with organ transplants (75.4%).Citation14 This difference is probably attributed to the popularization of media dissemination on COVID-19 vaccines and people’s high trust in governments. Up to now, hardly any research has taken the immunosuppressive factor into consideration. Special attention should be reserved to SOT recipients when formulating and implementing vaccination policies.
A noticeable finding in our study is that 26.2% of the hesitancy participants reported that they are reluctant or uncertain to get vaccinated as a negative suggestion from clinicians. Aslam et al. reported that experience with the influenza vaccine and the adjuvanted recombinant zoster vaccine can be extrapolated to the COVID-19 vaccine.Citation21 Recently, few studies have reported the efficiency and safety in SOT recipients, indicating the benefits of vaccination in this population.Citation15,Citation22–24 Based on the current guidelines, SOT recipients are at high risk of poor outcomes with SARS-CoV-2, and it is suggested that they be vaccinated with any COVID-19 vaccines as soon as they become approved and available.Citation25 Nevertheless, non-transplant physicians may know little about vaccination for SOT recipients. This result implies that the training of clinicians should be strengthened, not only for transplants but also for non-transplant physicians, regarding the significant vaccine-related benefits based on the scientific mechanisms and clinical trial findings.Citation21
Regarding the possible way to promote vaccine coverage, the choice of “organ transplantation physicians’ positive advice” tops significantly the other options (92.7%). While non-organ transplantation physicians’ positive advice only accounted for 10.3%. This finding reminded us that transplantation physician recommendation plays an important role in vaccine acceptance, often being cited as the top reason for vaccination.
Factors associated with willingness to get vaccinated were evaluated. Consistent with studies conducted by Garcia et al. and Gennaro et al., people with positive intention toward influenza vaccination during the current season were more willing to be vaccinated.Citation26,Citation27 On the contrary, people who were vaccinated against influenza during the last season were less likely to get vaccinated. This was indifferent from previous studies in normal immunity population.Citation13,Citation28,Citation29 Our survey indicated that people who perceived the importance of vaccines were more willing to be vaccinated. They believe that vaccination could protect them from being infected with SARS-CoV-2. This result suggested that improving people’s awareness of vaccine importance will help to increase the willingness to get vaccinated. We also found that transplantation organ type was another significant factor. Liver transplant recipients will be more inclined to get vaccinated. The intensity of immunosuppressants may be one of the factors contributing to this difference.
For the main source of information about vaccines, respondents who depended on medical doctors, scientists, and scientific journals were the most likely to get vaccinated. Therefore, the role of such sources in addressing vaccine issues and providing trust information should be advocated by the media. Earnshaw et al. also highlighted the importance of physicians’ role, they reported that physicians were the most trusted source of information about COVID-19.Citation30
As expected and in line with the existing studies,Citation13,Citation31,Citation32 respondents with higher educational levels had a higher willingness to get vaccinated. Perhaps, they had a better understanding of SARS-CoV-2 and COVID-19 vaccine than those with lower educational background. Another reason might be related to their willingness to learn about the knowledge of vaccines. This result also showed the importance of publicity and education among participants with low educational level.
Our study has several limitations. First, participant selection was not randomized but convenience sampling, which can cause selection bias. Second, the willingness to get vaccinated and the underlying reasons for vaccine hesitancy are not applicable to the general population, as it falls outside the research aim. Third, this survey is based on WeChat and WeChat platform, which may be more challenging for older people, people with visual impairment and those who do not use WeChat were likely underrepresented. Another limitation was that the 6 items in this survey are insufficient to evaluate patients’ knowledge about COVID-19 vaccine. Nevertheless, based on the large sample of our survey, it can still indicate that more than half of the Chinese SOT recipients are hesitant to be vaccinated against SARS-CoV-2 at present. It is important and necessary for the government to popularize the COVID-19 vaccine information to immunosuppressant people in the future. This should be strengthened when preparing for the next wave of viral attack.
Conclusions
To our knowledge, this is the first study investigating the attitude toward COVID-19 vaccination among SOT patients after COVID-19 vaccines approved in China. Vaccination hesitancy can be found in Chinese SOT recipients after the COVID-19 vaccine had been marketed in the present study. This could pose a threat to the preventive measures aimed at controlling COVID-19 spread in immunosuppressed population. Our results revealed the possible factors associated with vaccination willingness, indicated the necessity for SOT recipients to receive more comprehensive and accessible health education about vaccine, emphasized the critical role of transplantation physicians in promoting vaccine acceptance among SOT recipients. We hope that our study could help governments to target communication in the ongoing COVID-19 vaccination campaign.
Author contributions
Conceived and designed the experiments: Tingting Chen, Jina Wang, and Xiaoyu Li. Performed the data analysis: Tingting Chen, Ying Jiang and Lihong Huang. Validated the data: Qiuting Li, Qingqing Cai, Qing Xu and Yuzhu Wang. Administrated the project: Qianzhou Lv and Jina Wang. Supervised the project: Qianzhou Lv and Xiaoyu Li. Wrote the paper: Tingting Chen and Jina Wang.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Azzi Y, Bartash R, Scalea J, Loarte-Campos P, Akalin E. COVID-19 and solid organ transplantation: a review article. Transplantation. 2021;105:37–55. doi:10.1097/tp.0000000000003523.
- World Health Organization (WHO). Draft landscape of COVID-19 candidate vaccines. 2021 June 15 [accessed 2021 June 16]. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines.
- National Health Commission of the People’s Republic of China. The first edition of COVID-19 vaccine vaccination technical guideline. 2021 Mar 29 [accessed 2021 June 16]. http://www.nhc.gov.cn/jkj/s3582/202103/c2febfd04fc5498f916b1be080905771.shtml.
- Coustasse A, Kimble C, Maxik K. COVID-19 and vaccine hesitancy: a challenge the United States must overcome. J Ambul Care Manage. 2021;44:71–75. doi:10.1097/jac.0000000000000360.
- Facciolà A, Visalli G, Orlando A, Bertuccio MP, Spataro P, Squeri R, Picerno I, Di Pietro A. Vaccine hesitancy: an overview on parents’ opinions about vaccination and possible reasons of vaccine refusal. J Public Health Res. 2019;8(1):1436. doi:10.4081/jphr.2019.1436.
- Dzieciolowska S, Hamel D, Gadio S, Dionne M, Gagnon D, Robitaille L, Cook E, Caron I, Talib A, Parkes L, et al. Covid-19 vaccine acceptance, hesitancy and refusal among Canadian healthcare workers: a multicenter survey. Am J Infect Control. 2021;49:1152–57. doi:10.1016/j.ajic.2021.04.079.
- Baldo V, Reno C, Cocchio S, Fantini MP. SARS-CoV-2/COVID-19 vaccines: the promises and the challenges ahead. Vaccines. 2021;9:21. doi:10.3390/vaccines9010021.
- Sallam M, Dababseh D, Eid H, Hasan H, Taim D, Al-Mahzoum K, Al-Haidar A, Yaseen A, Ababneh NA, Assaf A, et al. Low COVID-19 vaccine acceptance is correlated with conspiracy beliefs among university students in Jordan. Int J Environ Res Public Health. 2021;18:2407. doi:10.3390/ijerph18052407.
- Edwards B, Biddle N, Gray M, Sollis K. COVID-19 vaccine hesitancy and resistance: correlates in a nationally representative longitudinal survey of the Australian population. PLoS One. 2021;16:e0248892. doi:10.1371/journal.pone.0248892.
- Chew NWS, Cheong C, Kong G, Phua K, Ngiam JN, Tan BYQ, Wang B, Hao F, Tan W, Han X, et al. An Asia-Pacific study on healthcare workers’ perceptions of, and willingness to receive, the COVID-19 vaccination. Int J Infect Dis. 2021;106:52–60. doi:10.1016/j.ijid.2021.03.069.
- Yurttas B, Poyraz BC, Sut N, Ozdede A, Oztas M, Uğurlu S, Tabak F, Hamuryudan V, Seyahi E. Willingness to get the COVID-19 vaccine among patients with rheumatic diseases, healthcare workers and general population in Turkey: a web-based survey. Rheumatol Int. 2021:1–10. doi:10.1007/s00296-021-04841-3.
- Sun S, Lin D, Operario D. Interest in COVID-19 vaccine trials participation among young adults in China: willingness, reasons for hesitancy, and demographic and psychosocial determinants. medRxiv. 2020. doi:10.1101/2020.07.13.20152678.
- Gan L, Chen Y, Hu P, Wu D, Zhu Y, Tan J, Li Y, Zhang D. Willingness to receive SARS-CoV-2 vaccination and associated factors among Chinese adults: a cross sectional survey. Int J Environ Res Public Health. 2021;18. doi:10.3390/ijerph18041993.
- Ou MT, Boyarsky BJ, Zeiser LB, Po-Yu Chiang T, Ruddy J, Van Pilsum Rasmussen SE, Martin J, St. Clair Russell J, Durand CM, Avery RK, et al. Kidney transplant recipient attitudes toward a SARS-CoV-2 vaccine. Transplant Direct. 2021;7:e713. doi:10.1097/TXD.0000000000001171.
- Boyarsky BJ, Ou MT, Greenberg RS, Teles AT, Werbel WA, Avery RK, Massie AB, Segev DL, Garonzik-Wang JM. Safety of the first dose of SARS-CoV-2 vaccination in solid organ transplant recipients. Transplantation. 2021;105:e56–e7. doi:10.1097/TP.0000000000003654.
- Panda DS, Giri RK, Nagarajappa AK, Basha S. COVID-19 vaccine, acceptance, and concern of safety from public perspective in the state of Odisha, India. Hum Vaccin Immunother. 2021:1–5. doi:10.1080/21645515.2021.1924017.
- Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27:225–28. doi:10.1038/s41591-020-1124-9.
- Liu R, Zhang Y, Nicholas S, Leng A, Maitland E, Wang J. COVID-19 vaccination willingness among Chinese adults under the free vaccination policy. Vaccines. 2021;9:292. doi:10.3390/vaccines9030292.
- Mo PK, Luo S, Wang S, Zhao J, Zhang G, Li L, Li L, Xie L, Lau JTF. Intention to receive the COVID-19 vaccination in China: application of the diffusion of innovations theory and the moderating role of openness to experience. Vaccines. 2021;9:129. doi:10.3390/vaccines9020129.
- Qin W, Wang E, Ni Z. Chinese consumers’ willingness to get a COVID-19 vaccine and willingness to pay for it. PLoS One. 2021;16:e0250112. doi:10.1371/journal.pone.0250112.
- Aslam S, Goldstein DR, Vos R, Gelman AE, Kittleson MM, Wolfe C, Danziger-Isakov L. COVID-19 vaccination in our transplant recipients: the time is now. J Heart Lung Transplant. 2021;40:169–71. doi:10.1016/j.healun.2020.12.009.
- Boyarsky BJ, Werbel WA, Avery RK, Tobian AAR, Massie AB, Segev DL, Garonzik-Wang JM. Immunogenicity of a single dose of SARS-CoV-2 messenger RNA vaccine in solid organ transplant recipients. JAMA. 2021;325(17):1784–86. doi:10.1001/jama.2021.4385.
- Werbel WA, Boyarsky BJ, Ou MT, Massie AB, Tobian AAR, Garonzik-Wang JM, Segev DL. Safety and immunogenicity of a third dose of SARS-CoV-2 vaccine in solid organ transplant recipients: a case series. Ann Intern Med. 2021 June 15;174:1330–32. PMID: 34125572. doi:10.7326/L21-0282.
- Boyarsky BJ, Werbel WA, Avery RK, Tobian AAR, Massie AB, Segev DL, Garonzik-Wang JM. Antibody response to 2-dose SARS-CoV-2 mRNA vaccine series in solid organ transplant recipients. JAMA. 2021;325(21):2204–06. doi:10.1001/jama.2021.7489.
- Transplant Infectious Disease. Guidance on coronavirus disease 2019 (COVID-19) for transplant clinicians updated 1 March 2021. 2021 Mar 1 [accessed 2021 June 11]. https://tts.org/index.php?option=com_content&view=article&id=749&Itemid=140.
- Garcia P, Montez-Rath ME, Moore H, Flotte J, Fults C, Block MS, Han J, Dittrich M, Parsonnet J, Chertow GM, et al. SARS-CoV-2 vaccine acceptability in patients on hemodialysis: a nationwide survey. J Am Soc Nephrol. 2021;32:1575–81. doi:10.1681/asn.2021010104.
- Di Gennaro F, Murri R, Segala FV, Cerruti L, Abdulle A, Saracino A, Bavaro DF, Fantoni M. Attitudes towards anti-SARS-CoV2 vaccination among healthcare workers: results from a national survey in Italy. Viruses. 2021;13:371. doi:10.3390/v13030371.
- Chang YW, Tsai SM, Lin PC, Chou FH. Willingness to receive influenza vaccination during pregnancy and associated factors among pregnant women in Taiwan. Public Health Nurs. 2019;36:284–95. doi:10.1111/phn.12600.
- Alfageeh EI, Alshareef N, Angawi K, Alhazmi F, Chirwa GC. Acceptability of a COVID-19 vaccine among the Saudi population. Vaccines. 2021;9:226. doi:10.3390/vaccines9030226.
- Earnshaw VA, Eaton LA, Kalichman SC, Brousseau NM, Hill EC, Fox AB. COVID-19 conspiracy beliefs, health behaviors, and policy support. Transl Behav Med. 2020;10:850–56. doi:10.1093/tbm/ibaa090.
- Sallam M, Dababseh D, Eid H, Al-Mahzoum K, Al-Haidar A, Taim D, Yaseen A, Ababneh NA, Bakri FG, Mahafzah A, et al. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines. 2021;9:42. doi:10.3390/vaccines9010042.
- Rzymski P, Zeyland J, Poniedziałek B, Małecka I, Wysocki J. The perception and attitudes toward COVID-19 vaccines: a cross-sectional study in Poland. Vaccines. 2021;9(4):382. doi:10.3390/vaccines9040382.