ABSTRACT
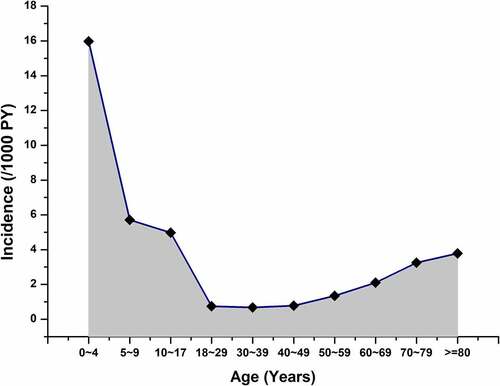
Community-acquired pneumonia (CAP) is a lower respiratory tract infection. It is one of the commonest infectious diseases and the third leading cause of death worldwide. However, the epidemiological profiles of CAP in southeastern China are unknown. Data of inpatients and outpatients diagnosed with CAP from January 1, 2015 to December 31, 2020 were obtained from the National Healthcare Big Data in Fuzhou (Fuzhou Database). This database covers medical data from 37 hospitals and 159 community health service stations. The incidence rate, treatment pattern, and direct medical costs of CAP were assessed using clinical data. A total of 8,156,237 patients were enrolled, with a mean age of 33.72 ± 20.88 years. The overall incidence rate of CAP was 3.13 (95% confidence interval [CI]: 3.11–3.15) per 1000 person-years (PY), with 15.97 (95% CI: 15.85–16.08) per 1000 PY in children below 5 years old and 2.62 (95% CI: 2.57–2.66) per 1000 PY in the elderly ≥60 years. The cost per outpatient was $242.83 ± 341.62, and the cost per inpatient was $4,530.4 ± 9,151.68. The three most used therapeutic drugs in patients with CAP are cefotaxime, moxifloxacin, and azithromycin. In addition, despite the ability of both imported and domestic pneumococcal conjugate vaccines to reduce the incidence rate of CAP, the current vaccination coverage rates were relatively low. We suggest that more attention should be paid to the disease burden of CAP, especially due to its great economic burden in China.
Introduction
Community-acquired pneumonia (CAP) is a lower respiratory tract infection (LRTI). It is the third leading cause of death in the world and one of the commonest infectious diseases. The disease burden of CAP remains high worldwide, particularly in developing countries.Citation1,Citation2
The incidence rate of CAP varies with age: it is higher in children below 5 years old than in other age groups.Citation3 The incidence rate of CAP in children below 5 years old is 34–40 per 1000 person-years (PY) in Europe and North America and 65.8 per 1000 PY in China.Citation4,Citation5 According to United States (US) data, the incidence rate of CAP in hospitalized adults in the US is 24.8 (95% confidence interval [CI]: 23.5–26.1) per 10000 PY and 164.3 (95% CI: 141.9–189.3) per 10000 PY in older adults ≥80 years.Citation6 In China, the incidence is 2.4–14.98 per 1000 PY in people aged ≥18 years.Citation5
In addition to incidence rates, hospitalization and mortality rates should also be considered. Studies have shown that approximately 25% of patients with CAP need hospitalization,Citation7 and 10% of these hospitalized patients need further treatment in the intensive care unit (ICU).Citation8 The mortality rate of CAP in the elderly is higher than in other age populations.Citation3 A study in Japan showed that the mortality rates of hospitalized patients with CAP aged 15–44, 45–64, 65–74, and ≥75 years was 1.4%, 3.3%, 6.9%, and 9.3%, respectively.Citation9 The high incidence, hospitalization, and mortality rates impose a huge burden, including physical, psychological, and especially economic burdens on patients and their families or caregivers. In 2010, the 13-valent pneumococcal conjugate vaccine (PCV13) was introduced in the US for children below 2 years old. Its effectiveness in reducing the incidence of pneumonia and other invasive pneumococcal diseases in children has been shown in several countries. Although the imported (Pfizer, 2017) or domestic (Walvax, 2020) PCV13 vaccine was introduced in China in 2017, the current vaccination coverage rate is relatively low due to vaccine hesitancy in children’s guardians in China.
The epidemiological profiles of CAP have been studied in European and American countries. Meanwhile, such studies are rare in China. Very few studies have reported the national and all-age group incidence rate of CAP in most provinces and cities in mainland China. However, in Fuzhou the medical data can be obtained from the Fuzhou database, which has a high coverage of the residents’ medical data. Fuzhou, the capital of Fujian province, is a representative city in Southeast China with four distinct seasons and a well-developed economy. To provide more evidence on the disease burden of CAP and inform future prevention and disease management policy decisions in China, this study aimed to assess the incidence, treatment pattern, and direct medical costs of CAP using clinical data.
Materials and methods
Data source
This was a retrospective observational study. Data was obtained from the National Healthcare Big Data in Fuzhou (Fuzhou Database). It is a regional health information system that includes medical data from 37 hospitals and 159 community health service stations (CHSSs) in Fuzhou City. The database has collected over two billion medical records for approximately 10 million Fuzhou residents since September 2001. This data platform links major clinical information systems, such as the hospital information systems, laboratory information management systems, electronic medical records (EMRs), picture archiving and communication systems, surgical information, and medical record information systems. All electronic medical data records were updated every 24 h. Unlike most medical insurance databases,Citation5 the Fuzhou database covers a wider range of people, including both the insured and uninsured – this is more representative of a real-world population. The 10th revision of the International Classification of Diseases (ICD-10) program coding system was used to encode diagnoses. The number of permanent residents in Fuzhou by the end of 2019 was 7.8 million according to the 2019 population change sample survey.Citation10
Study design
Data of inpatients and outpatients diagnosed with CAP in Fuzhou between January 1, 2015 and December 31, 2020 were collected from the database. Since CAP and hospital-acquired pneumonia (HAP) do not have different ICD codes, we used the medical term “肺炎,” which is pneumonia in Chinese, and the ICD-10 code for pneumonia as search terms. The exclusion criteria were as follows: (1) HAP (pneumonia that occurred 48 hours after admission with no diagnosis of pneumonia before admission) or ventilator-associated pneumonia (VAP, pneumonia that occurred 48 to 72 hours after mechanical ventilation), (2) tuberculosis or human immunodeficiency virus, (3) immunosuppression, (4) pulmonary interstitial pneumonia, and (5) multiple episodes of CAP in the same patient.Citation5 New-onset CAP was defined as the first diagnosis of CAP after the study start date with no clinical diagnosis of CAP within 90 days prior to the study start date. Recurrent CAP was defined as CAP occurring after a 90-day CAP-free period since the previous diagnosis. For example, if the interval between two episodes was less than 90 days, only the first episode was included. The baseline information of each enrolled patient was collected, including sex, date of birth, date of CAP diagnosis, urban/rural residency, and type of health insurance. Hospital information and the criteria used to screen all patients are shown in the Supplemental tables. After the search was completed, the records were reviewed by two independent respiratory physicians to ensure accurate and complete identification of CAP cases.
Statistical analysis
All continuous variables with normal distribution are presented as mean ± standard deviation (SD) and examined using a t-test. The non-normal variables were reported as median (interquartile range [IQR]) and examined using the Wilcoxon rank-sum test. Categorical variables are shown as frequency and percentage of each category and evaluated using the χ2 test or Fisher’s exact test, where appropriate. All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, North Carolina, USA). A significance level of 0.05 was assigned for each hypothesis testing.
Regarding the incidence of CAP, the numerator (M) was the number of patients diagnosed with CAP at least once during the study period. The denominator (N) was either the follow-up time from the study start date to the date of first diagnosis of CAP (CAP subjects), date of death, or end of the study date, whichever came first for non-CAP subjects. The incidence rate of CAP was calculated per 1000 PY with its exact Poisson 95% CIs using the formula: (M/N) × 1000. The overall incidence rates and incidence rates stratified by sex, age group, season (spring, March–May; summer, June–August; autumn, September–November; and winter, December–February), ethnicity (Han vs. other ethnicity groups), region (urban vs. rural), and hospital grade (second-class hospital and CHSS vs. tertiary hospital). For precision purposes, a sensitivity analysis was performed to estimate the overall CAP incidence over a 5-year period of 2015–2019 and in all the strata to exclude the effects of coronavirus disease (COVID-19), given the reinforcement of the restriction of personnel movement and medical visits in Fuzhou in early 2020.
Regarding the economic burden of CAP, healthcare costs were calculated by considering diagnostic cost groups, total costs, and discharge numbers. The costs were estimated per person for outpatient and inpatient groups, respectively, and classified into cost for therapy, examination, surgical procedures, medications, nursing care, and other utilities. For the treatment pattern analysis, the costs of medications were stratified by antibiotics, antivirus, medicine, and traditional Chinese medicine (TCM).
This study was approved by the ethical review committee of Zhejiang Chinese Medical University, and the requirement for informed consent was waived. The study was performed in accordance with the principles of the Declaration of Helsinki.
Results
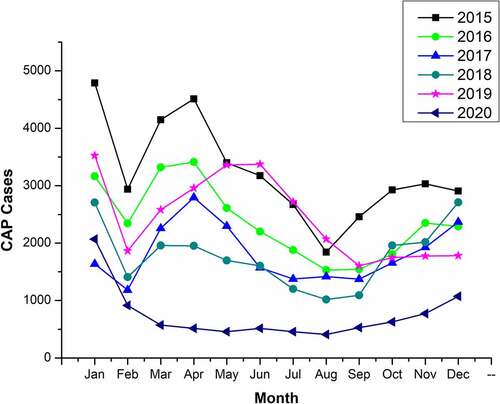
The participant selection process is shown in . A total of 14,367,648 inpatient and outpatient records within the study period were obtained. Cases with duplicate records (5,118,466) and missing information or outliers (1,092,945) including negative and null values for age, null values for sex, consecutive hospitalization for more than 6 years, and primary diagnosis of “?,” and null diagnosis were excluded. A total of 8,156,237 patients were enrolled, with a mean age of 33.72 ± 20.88 years. These participants came from 182 medical institutions, including 10 tertiary hospitals, 27 second-class hospitals, and 159 CHSSs. Of the 306,874 patients diagnosed with pneumonia, 164,726 (53.68%) were male. There were 95,077 (30.98%), 46,508 (15.16%), and 10,123 (3.3%) patients aged <5, 5–18, and ≥80 years old. Most of the patients with pneumonia were of Han ethnicity (252,884, 82.41%). Pneumonia was diagnosed mostly in spring (91,431, 29.79%), followed by winter (84,742, 27.61%), summer (66,632, 21.71%), and autumn (64,069, 20.88%) ().
In total, 148,711 patients had one or more CAP diagnoses, among whom 82,748 (55.64%) were male. Children below 5 years old were the most affected (72,926, 49.04%). There were 34,691 (23.33%) patients aged 5–18 years and 2,626 (1.77%) aged ≥80 years. Similar to patients with pneumonia, most patients with CAP were of Han ethnicity (111,210, 74.78%). The highest number of cases was diagnosed in spring (44,812, 30.13%), followed by winter (41,671, 28.02%), autumn (31,191, 20.97%), and summer (31,037, 20.87%).
Of all patients with CAP, 139,239 (93.63%) were from urban areas. A total of 77,255 (51.95%) patients were diagnosed in tertiary hospitals, and 71,456 (48.05%) were diagnosed in second-class hospitals and CHSSs. Of 158,163 patients with pneumonia but without a CAP diagnosis, 81,978 (51.83%) were male. The proportion of patients aged <18 years was lower in the non-CAP pneumonia group than in the CAP group, with 22,151 (14.01%) children below 5 years old and 11,817 (7.47%) participants aged 5–18 years (). In addition, there were 64,109 inpatients, 84,602 outpatients, and 8,724 ICU patients. The CAP and ICU admission rates were 43.12% and 13.61%, respectively.
Table 1. Basic characteristics of patients registered in the Fuzhou database in 2015–2020
Incidence rate of CAP
The overall incidence rate of CAP in was 3.13 (95% CI: 3.11–3.15) per 1000 PY. The incidence rate was higher in men than in women (3.52 [95% CI: 3.5–3.55] vs. 2.74 [95% CI: 2.72–2.77] per 1000 PY). The incidence rate was highest in children below 5 years old (15.97 [95% CI: 15.85–16.08] per 1000 PY), followed by 5.71 (95% CI: 5.62–5.8) per 1000 PY and 0.78 (95% CI: 0.76–0.8) per 1000 PY in the patients aged 5–10 and 40–50 years, respectively. The incidence rate increased with age, reaching 3.78 (95% CI: 3.63–3.92) per 1000 PY in the elderly aged ≥80 years. The overall incidence rate for older adults aged ≥60 years was 2.62 (95% CI: 2.57–2.66) per 1000 PY. The absolute number of patients with Han ethnicity in the total CAP population was approximately thrice that of other ethnic groups, but the incidence rate was lower than that of others (2.68 [95% CI: 2.67–2.7] vs. 6.26 [95% CI: 6.14–6.26] per 1000 PY). The highest incidence rate was observed in winter and spring (3.81 [95% CI: 3.77–3.85] and 3.68 [95% CI: 3.65–3.72] per 1000 PY), followed by autumn (2.68 [95% CI: 2.65–2.71] per 1000 PY), and summer (2.43 [95% CI: 2.4–2.46] per 1000 PY). The incidence rate in urban areas was similar to that in rural areas (3.13 [95% CI: 3.11–3.15] vs. 3.14 [95% CI: 3.08–3.21] per 1000 PY]. The incidence of CAP was higher in tertiary hospitals than in second-class hospitals and CHSSs (4.06 [95% CI: 4.03–4.09] vs. 2.51 [95% CI: 2.49–2.53] per 1000 PY) ().
Table 2. Incidence rate of CAP in the Fuzhou database in 2015–2020
A sensitivity analysis was performed to estimate the incidence of CAP over a 5-year period, 2015–2019. The incidence rate of CAP in Fuzhou during this period was 3.46 (95% CI: 3.44–3.48) per 1000 PY, which was higher than that in 2015–2020 ().
Table 3. Incidence rate of CAP in the Fuzhou database in 2015–2019
Cost
The costs associated with CAP in Fuzhou were estimated. The mean cost per outpatients in 2015–2020 was $242.83 ± 341.62. The outpatient costs were mainly spent on medicine and therapeutics (according to the cost index in the system). The mean cost of medicine was not significantly different from that of TCM ($117.38 ± 214.18 vs $ 119.69 ± 176.07), and the mean cost of therapeutics was lower ($77.56 ± 94.98). The mean cost per inpatient was much higher than that per outpatient ($4,530.4 ± 9,151.68). The cost of medicine was highest ($1,518.16 ± 3,348.79), followed by that of laboratory workup ($928.83 ± 1,437.92), examination ($ 758.04 ± 1,428.17), and therapeutic drugs ($ 722.25 ± 1,922.31). The mean length of hospital stay was 8.73 ± 27.22 days ().
Table 4. Direct economic cost ($) per person
Medicine
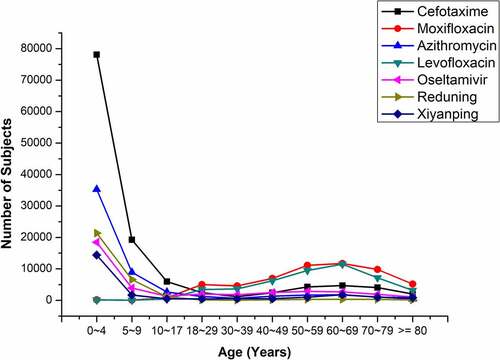
The three commonest administered medicines were all antibiotics: cefotaxime (n = 124,372), moxifloxacin (n = 53,399), and azithromycin (54,906) (). The most used antiviral medicines were oseltamivir (n = 38,433) and ribavirin (n = 6,222). TCM was used less than antibiotics (68,921) ().
Table 5. The medication and corresponding cost for CAP
The use of different medicines in the various age groups is shown in a line graph (). Cefotaxime, azithromycin, oseltamivir, and two TCMs (reduning and xiyanping) were mainly used in children below 5 years old, and the use of these medicines decreased with age. Moxifloxacin and levofloxacin were used more in adults aged ≥50 years than in children below 5 years old. The medication use among the children and adults in Fuzhou was in accordance with the CAP guidelines for diagnosis and treatment of children and adults.
Discussion
To the best of our knowledge, this is the first study using data from a real-world database to study the epidemiological profiles of CAP in Fuzhou, China. We found that the incidence rate of CAP in Fuzhou was 3.13 per 1000 PY for all age groups in our study. The incidence rate was higher in males than females; this is similar to findings from other studies.Citation5,Citation11–13 A recent national study by Zhan et al. showed a mean incidence rate of 7.13 per 1000 PY for 28 other provinces,Citation5 which was much higher than that in our study. However, the lowest incidence in their study was in South China (2.82 per 1000 PY), which was similar to our results. The incidence rate in Fuzhou, which is a southeastern city, is presumably lower than the national incidence rate. Compared with the data of European and American countries,Citation6,Citation14 the incidence rate of CAP in our study was relatively low. This may be as a result of the COVID-19 outbreak, which may have impacted the incidence rate of CAP; the overall incidence was higher in 2015–2019 than in 2015–2020. Furthermore, the lockdown of many areas of China, including Fuzhou, in early 2020 resulted in a decrease in personnel movement and medical visits. According to the estimated CAP data for different months and years in 2015–2019, excluding the special data from 2020, it was found the two peaks were in March–May and December–January (spring and winter).
The incidence was grouped by age in a U-shaped curve, consistent with the trends in previous studies.Citation5,Citation13 Some studies have shown that the incidence rate of CAP is significantly higher in children below 5 years old than in other age groups,Citation5,Citation15 which is similar to our findings. While the burden of CAP is greater among the elderly in Europe and the US, the burden of CAP is still higher in young children in China, which could be correlated, among other factors, with a delay in the introduction of the pediatric pneumococcal conjugate vaccine (PCV) in China.
Regarding the seasonal distribution of CAP, the incidence of CAP was much higher in winter and spring than in summer and autumn in Fuzhou. Given that the seasonal climate varies greatly with regions in China, this finding may not be generalizable in the whole nation; however, all regions in southeast China have similar geographic features. The seasonal patterns caused by different pathogens are different.Citation16,Citation17 Bacterial infection is the main cause of CAP in adults, but some studies have shown that Mycoplasma is the commonest pathogen of CAP in young adults.Citation12,Citation18–20 Of all CAP cases, 10.23% are from mixed infections (infections caused by multiple pathogens). The commonest mixed infections are caused by a combination of bacteria and viruses, such as Streptococcus pneumoniae (SP) mixed with respiratory syncytial virus (RSV), bacteria mixed with mycoplasma, and virus mixed with Mycoplasma infection.Citation17 Although some experts have suggested that CAP is not seasonal,Citation19 most studies concluded that CAP caused by bacteria, respiratory viruses, and multiple pathogens are most common in winter and spring, while Mycoplasma pneumoniae is more frequent in summer and autumn.Citation16,Citation21,Citation22 With regard to the decrease of incidence in Feb, it may be due to the fact that citizens avoid going to the hospital, and the decrease in population mobility during the Chinese New Year holiday in February.
We observed different treatment patterns in the different age groups. Cefotaxime was the most used medicine and was used twice as often as the second most used medicine, azithromycin. We also estimated the cost of common medicines, and the most expensive was cefotaxime. In this study, cefotaxime was mainly used in children below 5 years old. In addition, its use was decreased in children and teenagers aged 5–18. It was rarely used in adults ≥18 years old. Similarly, azithromycin, oseltamivir, reduning, and xiyanping were commonly used in young people, but were less commonly used in older adults. In contrast, moxifloxacin and levofloxacin were used less often in people below 18 years old and more often in adults. Antibiotics were the main medicines used in CAP, while antiviral medicines were rarely used. This may be explained by the greater use of second-class hospitals and CHSSs, where antibiotics might be preferred. The highest cost for both inpatients and outpatients was the cost of medicine; this cost was higher for inpatients. This might mean that antibiotic use imposes a huge economic burden on patients with CAP. Moreover, microbiological testing is needed to ensure fast, accurate, and affordable testing for individualized and early treatment for patients with CAP.Citation23 Moreover, no prospective study has examined the benefits of antibiotics in patients with probable viral pneumonia.Citation24 The impact of these factors on the treatment patterns in our context is not possible due to limited resources.
China has a population of more than 1.4 billion persons,Citation25 and southeast China covers Zhejiang, Jiangxi, Guangdong, and Fujian provinces, which have similar characteristics similar with Fuzhou. Based on the incidence rate in Fuzhou in this study, approximately 25,000 people in Fuzhou and more than 5 million people in China had CAP infection within the study period. In the face of a great disease burden, preventive measures are very important. While daily non-pharmaceutical measures, such as wearing masks and frequent hand washing, are effective in preventing CAP, the development and use of vaccines against CAP pathogens are very necessary for a larger population. The vaccine against SP (Spn) is the commonest and is known to reduce the risk of pneumonia in certain populations. Currently, the most commonly used Spn vaccine in China is PCV13.Citation3,Citation26 In addition, the influenza vaccine can prevent pneumonia from influenza viruses and has a certain preventive effect on bacterial pneumonia secondary to influenza.Citation27 However, these vaccines are yet to be included in the China National Expanded Programme on Immunization (EPI) or regional (southeastern China or Fuzhou) medical reimbursement programs, resulting in significantly lower vaccination coverage rates. An analysis by Hong Zhang showed that the coverage of PCV13 among children aged 2 months to 6 years in Zhongshan, Guangdong province in 2016 and 2019 was 4.82% and 2.52%, respectively.Citation28 In the 2011–2012 influenza season, 6.4% of urban residents were vaccinated against seasonal influenza,Citation29 and the overall vaccination rate for people aged ≥60 years was only 4%.Citation30 The influenza vaccine uptake in China fell substantially below the World Health Assembly (WHA) target of 75% in the elderly by 2010.Citation31 Therefore, an effective vaccination strategy and reimbursement mechanism, particularly for high-risk groups such as children and older adults, should be developed in Fuzhou or China.
This study has several limitations. First, the hospitals covered by the Fuzhou database were limited. The Fuzhou database covered 10 tertiary hospitals and 172 second-class hospitals and CHSSs, which means that second-class hospitals and CHSSs were the most used. Meanwhile, the information from provincial-level hospitals of Fujian was unavailable. Moreover, this study was concentrated in Fuzhou city only, and thus generalizing the results to other areas will require similar conditions or environmental factors. Second, case identification was limited to the database. Using the ICD-10 coding rules and Chinese names of cases to determine the target population, there may have been an over-diagnosis or under-diagnosis of patients. In addition, the data in the Fuzhou database are structured data of EMRs, which may not be suitable for research purposes. Therefore, errors in the data are almost inevitable. However, due to our limited resources, we could not quantify the impact in our study. Finally, although cases of other types of pneumonia, such as HAP, were excluded and the cases were reviewed by two independent reviewers, the accuracy of the case inclusion needs further verification. For example, the EMRs need to be reviewed for more details. This could not be performed due to our limited access to EMRs.
In conclusion, this study showed the overall incidence rate, cost, and medication associated with CAP in Fuzhou, as well as seasonal patterns and incidence rates in children and older adults. Based on the results of our study, more attention should be paid to the burden of CAP, especially to the economic burden. To reduce the burden of CAP, it is necessary to reinstate cost-effective preventive measures, such as vaccine development and utilization strategies, especially for vulnerable populations, including children and older adults.
Acknowledgments
We thank Yang Feng, Yufeng Song, Chenguang Zhu, and Siyang Qu from Xiamen Chazen Biomedical Technology Company for their help with data analysis, text editing, and language editing.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- WHO. The top 10 causes of death. 2020.
- Qazi S, Aboubaker S, MacLean R, Fontaine O, Mantel C, Goodman T, Young M, Henderson P, Cherian T. Ending preventable child deaths from pneumonia and diarrhoea by 2025. Development of the integrated global action plan for the prevention and control of pneumonia and diarrhoea. Arch Dis Child. 2015;100(Suppl 1):S23–8. doi:10.1136/archdischild-2013-305429.
- Zhai J, Cao B. Guidelines for the diagnosis and treatment of community-acquired pneumonia in adults in China (2016). Chin J Tuberc Respir Dis. 2016;39:253–79.
- Ostapchuk M, Roberts DM, Haddy R. Community-acquired pneumonia in infants and children. Am Fam Physician. 2004;70:899–908.
- Sun Y, Li H, Pei Z, Wang S, Feng J, Xu L, Gao P, Cao B, Zhan S. Incidence of community-acquired pneumonia in urban China: a national population-based study. Vaccine. 2020;38(52):8362–70. doi:10.1016/j.vaccine.2020.11.004.
- Jain S, Self WH, Wunderink RG, Fakhran S, Balk R, Bramley AM, Reed C, Grijalva CG, Anderson EJ, Courtney DM, et al. Community-acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med. 2015;373:415–27. doi:10.1056/NEJMoa1500245.
- Chinese Medical Doctor Association, Guidelines for emergency community acquired pneumonia in China (2015). Chin J Emergency Med. 2015; 24:1324–44.
- Ewig S, Ruiz M, Mensa J, Marcos MA, Martinez JA, Arancibia F, Niederman M, Torres A. Severe community-acquired pneumonia: assessment of severity criteria. Am J Respir Crit Care Med. 1998;158(4):1102–08. doi:10.1164/ajrccm.158.4.9803114.
- Falguera M, Pifarre R, Martin A, Sheikh A, Moreno A. Etiology and outcome of community-acquired pneumonia in patients with diabetes mellitus. Chest. 2005;128:3233–39. doi:10.1378/chest.128.5.3233.
- Fuzhou Statistics Bureau, Fuzhou had a permanent resident population of 7.8 million by the end of 2019 http://tjj.fuzhou.gov.cn/zz/zwgk/tjzl/tjxx/202002/t20200221_3203497.htm. 2020. (Fuzhou: Fuzhou Statistics Bureau)
- Li Y, An Z, Yin D, Liu Y, Huang Z, Ma Y, Li H, Li Q, Wang H. Disease burden of community acquired pneumonia among children under 5 y old in China: a population based survey. Hum Vaccin Immunother. 2017;13(7):1681–87. doi:10.1080/21645515.2017.1304335.
- Bao Z, Yuan X, Wang L, Sun Y, Dong X. The incidence and etiology of community-acquired pneumonia in fever outpatients. Exp Biol Med (Maywood). 2012;237(11):1256–61. doi:10.1258/ebm.2012.012014.
- Rozenbaum MH, Mangen MJ, Huijts SM, van der Werf TS, Postma MJ. Incidence, direct costs and duration of hospitalization of patients hospitalized with community acquired pneumonia: a nationwide retrospective claims database analysis. Vaccine. 2015;33:3193–99. doi:10.1016/j.vaccine.2015.05.001.
- Jain S, Williams DJ, Arnold SR, Ampofo K, Bramley AM, Reed C, Stockmann C, Anderson EJ, Grijalva CG, Self WH, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372:835–45. doi:10.1056/NEJMoa1405870.
- Juvén T, Mertsola J, Waris M, Leinonen M, Meurman O, Roivainen M, Eskola J, Saikku P, Ruuskanen O. Etiology of community-acquired pneumonia in 254 hospitalized children. Pediatr Infect Dis J. 2000;19(4):293–98. doi:10.1097/00006454-200004000-00006.
- Peng Y, Shu C, Fu Z, Li QB, Liu Z, Yan L. Pathogen detection of 1 613 cases of hospitalized children with community acquired pneumonia. Zhongguo Dang Dai Er Ke Za Zhi. 2015;17:1193–99.
- Ying X, Wang D, Song B, Lan D. Etiological investigation of community acquired pneumonia in adults in different seasons. Chin J PHM. 2014;30:843–4, 9.
- Liu Y, Chen M, Zhao T, Wang H, Wang R, Cai B, Cao B, Sun T, Hu Y, Xiu Q, et al. Causative agent distribution and antibiotic therapy assessment among adult patients with community acquired pneumonia in Chinese urban population. BMC Infect Dis. 2009;9(1):31. doi:10.1186/1471-2334-9-31.
- Liu Y, Chen M, Zhao T, Wang H, Wang R, Liu Q, Cai BQ, Cao B, Sun TY, and Hu YJ, et al. A multicentre study on the pathogenic agents in 665 adult patients with community-acquired pneumonia in cities of China. Chin J Tuberc Respir Dis 29 1 . 2006:3–8. 6638292
- Tao L, Hu B, He L, Wei L, Xie H, Wang B, Li H-Y, Chen X-H, Zhou C-M, Deng -W-W. Etiology and antimicrobial resistance of community-acquired pneumonia in adult patients in China. Chin Med J. 2012;125:2967–72.
- Shu L, Xu J, Wang S, Zhong H, Dong X, Jiang K, Zhang HY, Xiong Q, Wang C, Sun T, et al. Distribution of pathogenic microorganisms and its relationship with clinical features in children with community-acquired pneumonia. Chin J Contemp Pediatr. 2015;17:1056–61.
- Zhong L, Qiu Y. Pathogen changes and risk factor analysis of community - acquired pneumonia in the elderly of a hospital in Zhejiang province in recent 5 years. Chin Gen Pract. 2014;17:1506–10.
- Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, Cooley LA, Dean NC, Fine MJ, Flanders SA, et al. Diagnosis and treatment of adults with community-acquired pneumonia. an official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45–e67. doi:10.1164/rccm.201908-1581ST.
- Galván JM, Rajas O, Aspa J. Review of non-bacterial infections in respiratory medicine: viral pneumonia. Arch Bronconeumol. 2015;51:590–97. doi:10.1016/j.arbr.2015.09.015.
- National Bureau of Statistics (NBS), The seventh national population census. 2021.
- Chinese Preventive Medicine Association, Expert consensus on immunoprophylaxis of pneumococcal disease (2020 version). Chin J Vaccines Immunization. 2021; 27:1–47.
- Ferdinands JM, Gargiullo P, Haber M, Moore M, Belongia EA, Shay KD. Inactivated influenza vaccines for prevention of community-acquired pneumonia. Epidemiology. 2012;24:530–37. doi:10.1097/EDE.0b013e3182953065.
- Zhang H. Analysis of category 2 vaccines in children 2 month to 6 years old in eastern Zhongshan city. Shenzhen J Integr Traditional Chin West Med. 2021;31:42–44.
- Zhou L, Su Q, Xu Z, Feng A, Jin H, Wang S, Feng Z. Seasonal influenza vaccination coverage rate of target groups in selected cities and provinces in China by season (2009/10 to 2011/12). PLoS One. 2013;8:e73724. doi:10.1371/journal.pone.0073724.
- Feng Z, Yang T, Wang Q, Yan L, Leng Z, Chen S, Zhang XX, Yang WZ, et al. Prevent infectious diseases through vaccination, and protect health of the elderly. Natl Med J China. 2020;100:3821–26.
- WHO. 2003. Fifty-sixth World Health Assembly: prevention and control of influenza pandemics and annual epidemics. Geneva: Fifty-sixth World Health Assembly.