ABSTRACT
Background
Men who have sex with men (MSM), a population bearing the greatest HIV burden in many countries, may also be vulnerable to COVID-19. COVID-19 vaccines are essential to containing the pandemic. However, vaccine hesitancy may compromise vaccine coverage. We aimed to understand the uptake of COVID-19 vaccine and factors associated with COVID-19 vaccine hesitancy among HIV-infected MSM in mainland China.
Methods
A cross-sectional online survey among HIV-infected MSM was conducted between 13 and 21 February 2021 in mainland China. Variables including demographics, mental health status, HIV characteristics, and knowledge of and attitudes toward COVID-19 pandemic and COVID-19 vaccine were collected. Chi-square tests and multivariable logistic regression were used to analyze factors associated with COVID-19 vaccine hesitancy.
Results
A total of 1295 participants were included. The median age was 29.3 years (interquartile range [IQR] 25.2–34.0 years). The uptake of COVID-19 vaccine was 8.7%. Two main reasons for receiving vaccines were “regarded vaccination as self-health protection” (67.3%) and “trust in domestic medical technology” (67.3%). Among participants who did not initiate vaccination, concern about side effects (46.4%) and disclosure of HIV infection (38.6%) were top two reasons, and 47.2% had higher vaccine hesitancy. Men who had with high antiretroviral therapy (ART) adherence (adjusted odds ratio [aOR] 0.53, 95% confidence interval [CI] 0.35–0.80), often (0.26, 0.17–0.40) or sometimes (0.46, 0.31–0.67) paid attention to information about the COVID-19 vaccine, preferred domestic vaccines (0.37, 0.24–0.59), thought the pandemic had moderate (0.58, 0.38–0.90) and moderately severe or severe impact (0.54, 0.38–0.78) on immunity, who were waiting for vaccination programs organized at workplace (0.60, 0.44–0.81) and who were unaware of where to get COVID-19 vaccine (0.61, 0.45–0.82) had lower degree of COVID-19 vaccine hesitancy. Men who were concerned about the efficacy (1.72, 1.16–2.54) and side effects (2.44, 1.78–3.35) had higher degree of COVID-19 vaccine hesitancy.
Conclusion
COVID-19 vaccine uptake among HIV-infected MSM is still suboptimal. Understanding influencing factors of vaccine hesitancy among this group and making tailored measures to alleviate hesitancy would help improve the coverage of COVID-19 vaccination in this population.
Introduction
The raging COVID-19 pandemic caused by SARS‑CoV‑2 has been a major global public health threat. COVID-19 vaccines are expected to contain the pandemic to the largest extent. As of 24 July 2021, 18 vaccines were authorized by at least one national regulatory authority for public use.Citation1 Many countries have implemented phased distribution plans that prioritize those at the highest risk of complications, such as the elderly, and those at high risk of exposure and transmission, such as healthcare workers.Citation2 As of 24 July 2021, just under 4 billion doses of COVID‑19 vaccines have been administered worldwide.Citation3 In China, authorities officially launched a vaccination program for winter-spring period on 15 December 2020, which targeted at several key populations including workers engaging in the cold chain industry, customs, healthcare, and public transport and fresh produce markets.Citation4 This program was the first part of a “step by step plan” of COVID-19 vaccination,Citation5 and free vaccination has been introduced nationwide as the second part since 9 January 2021.Citation6 As of 9 June 2021, China has approved six domestic vaccine candidates. There are four inactivated vaccines (Sinopharm (Beijing), Sinopharm (Wuhan), Sinovac and Minhai Biotechnology Co), one adenovirus vector vaccine (CanSino) and one recombinant protein subunit vaccine (Anhui Zhifei Longcom).Citation7 Nearly 1.5 billion doses of COVID-19 vaccines have been administered across China as of 15 July.Citation8 Surveillance data from China CDC show that the incidence of general and abnormal reactions of China’s COVID-19 vaccines is lower than the average reported level of other kinds of vaccines in 2019.Citation9
With the development and gradual access of COVID-19 vaccines, herd immunity would be expected to form by mass vaccination, which has been regarded as a successful method for curbing the spread of many infectious diseases.Citation10 However, vaccine hesitancy, defined as delay in acceptance or refusal of vaccination despite availability of vaccination services,Citation11 can hinder the achievement of herd immunity.Citation12 It has adverse effect not only directly on the implementation of immunization programs but also on the scope of which people can be protected by vaccines.Citation13 Vaccine hesitancy has become a growing threat globally and may cause further outbreaks of infection.Citation14
In fact, before COVID-19 vaccines were approved numerous studies measured the willingness of potential COVID-19 vaccination. Acceptance rate varied extensively among countries, ranging from 23.6% in Kuwait to 97.0% in Ecuador.Citation15 Estimated 68.4% of the global population are willing to be vaccinatedCitation16 and acceptance rate was found 91.3% in China, which was higher than most countries worldwide.Citation15 Nevertheless, the willingness may not completely represent actual uptake.Citation17,Citation18 Vaccine hesitancy is one of the important determinants influencing the process between willingness and actual behavior, which might be related to individual attitudes, vaccine attributes and political factors.Citation19 Vaccine hesitancy is a continuumCitation18 rather than labeling individuals simply as “in favor of the vaccine” or “against the vaccine.”Citation20 Hence, this might be more convincing in assessing vaccine hesitancy.
The World Health Organization (WHO) states that people under health conditions affecting immunity are susceptible to SARS‑CoV‑2.Citation21 Compared with HIV-uninfected individuals, HIV-infected individuals were more likely to be infected with SARS‑CoV‑2Citation22 and have 30% higher severe or fatal COVID-19 outcomeCitation23 and mortality.Citation24 Furthermore, a recent study from South Africa showed that HIV-infected individuals diagnosed with SARS‑CoV‑2 who were with comorbidities, not on antiretroviral therapy (ART), with a history of immune suppression (CD4 count <200 cells per μL), with a history of a viral load of 1000 copies per mL or more were with worse COVID-19 in-hospital outcome.Citation25 Men who have sex with men (MSM), a population bearing the greatest HIV burden in many countriesCitation26 may also be vulnerable to SARS‑CoV‑2. Inadequate HIV prevention services or treatment interruptionCitation27 may worsen immunity for HIV-infected MSM and consequently increasing potential risk of SARS‑CoV‑2. Hence, COVID-19 vaccination may need to prioritize MSM, especially HIV-infected MSM as a vulnerable group.
Considering vaccination programs have been accessible in many countries, it is crucial to understand the actual implementation of COVID-19 vaccination in this population and possible reasons for reluctance or refusal of the vaccine so as to make tailored preventive strategies for this group. Our study aimed to understand the uptake and hesitancy relevant to COVID-19 vaccination among HIV-infected MSM in mainland China.
Methods
Study design and participants
We conducted a cross-sectional online survey between 13 and 21 February 2021. Individuals were recruited by convenience sampling through Li Hui Shi Kong, an online WeChat official account with over 76,000 HIV-infected subscribers from various regions in the country. A web-based, self-administered anonymous questionnaire was developed using the online survey platform Wenjuanxing (https://www.wjx.cn). Study information together with inclusion criteria and the quick response (QR) code of questionnaire was posted via Li Hui Shi Kong. Interested participants scanned the QR code to access the questionnaire. At the end of survey, participants were directed to a lottery page to win a random reimbursement ranging from RMB 10–130 (USD 1 ≈ RMB 6.4).
Eligibility criteria were as follows: 1) born male; 2) had male–male sex in the past; 3) self-reported HIV-positive; 4) consented to participate in the survey (chose “I agree” option before starting the survey). Participants would be excluded if 1) time to complete the questionnaire was less than 5 minutes; 2) the same option was selected for all items; 3) gave wrong answer to the quality control question (Is Beijing, Shenzhen, Guangzhou or Shanghai China’s capital?); 4) answered with logically contradictory options.
Measurement
Demographics, mental health status and HIV characteristics
Demographics were collected including age, gender, sexual orientation, residency, marital status, education, occupation, income, types of health insurance, health-related status (i.e., experience of disability/chronic diseases, frailty). The nine-item Patient Health Questionnaire (PHQ-9) and the seven-item Generalized Anxiety Disorder Scale (GAD-7) were used to assess depression and anxiety status. Viral load of HIV in recent year, HIV transmission route, time since HIV diagnosis, ART adherence measured by the eight-item Morisky Medication Adherence Scale (MMAS-8) were also asked in this survey.
Knowledge of and attitudes toward COVID-19 pandemic and COVID-19 vaccine
Perception of the severity of SARS-CoV-2, frequency of following information about the COVID-19 vaccine, source of COVID-19 vaccine information, preference toward domestic or imported vaccine were collected. Participants were also asked to answer “can ART prevent COVID-19 or not?” and COVID-19 impact on clinical attendance or ART collection/immunity/discrimination and inequity/other psychologic disruptions. The Vaccine Hesitancy Scale (VHS) was applied to measure COVID-19 vaccine hesitancy. The survey also asked reasons to initiate and not to initiate the COVID-19 vaccination.
Statistical analysis
For participants who did not initiate the COVID-19 vaccination, degree of vaccine hesitancy was dichotomized into “lower” and “higher” by the median value of scores of VHS. Chi-square tests were applied to assess differences between participants with lower and higher COVID-19 vaccine hesitancy in related factors of demographics, mental health status and HIV characteristics, and knowledge of and attitudes toward COVID-19 pandemic and COVID-19 vaccine.
Subsequently, multivariable logistic regression was employed to identify factors associated with degree of vaccine hesitancy. Enter method for logistic regression was conducted. Adjusted odds ratio (aOR) and the 95% confidence interval (95% CI) were estimated. Variance inflation factor (VIF) was calculated to ensure independence of each variable in the model. The final model had a mean VIF of 1.33. The outcome of Hosmer and Lemeshow Test (χ2 = 9.4, df = 8, P = 0.31) showed the model had a good fitting degree. All analyses were performed using SPSS 25.0 (IBM Corporation, New York, NY, United States). Statistical significance was set at P< 0.05. Bar graphs were depicted to describe reasons to initiate the COVID-19 vaccination or not and the distribution of each item of VHS by GraphPad Prism 8.0 (GraphPad Software, San Diego, California). Details on scoring methods, validity and reliability of scales can be viewed in Supplemental Files. Validity was calculated through confirmatory factor analysis (CFA) by AMOS 24.0 (IBM Corporation, New York, NY, United States).
Ethics approval
This study was approved by the Ethics Committee of the School of Public Health (Shenzhen), Sun Yat-sen University (Approval number: SYSU-PHS-2020042).
Results
Demographics, mental health status and HIV characteristics
A total of 1411 HIV-infected MSM completed the online survey. After quality control with inclusion and exclusion criteria, 1295 questionnaires were considered valid, with a valid response rate of 91.8%. Geographic distribution was shown in Supplementary File Table S1. Among participants who did not initiate the COVID-19 vaccination (N = 1182), over two-thirds (67.7%) were aged 26–44 years old. Most (89.7%) were cisgender men (10.3% were transgender women). Five hundred and forty-two (45.9%) participants had experience of disability, 406 (34.3%) participants had experience of chronic diseases, 18 (1.5%) participants were frail. Over four-fifths participants (81.3%) of participants had medium or high ART adherence. See .
Table 1. Demographics, mental health status and HIV characteristics among HIV-infected MSM in China, stratified by degree of vaccine hesitancy
Knowledge of and attitudes toward COVID-19 pandemic and COVID-19 vaccine
Nearly one-third (32.2%) participants often paid attention to information about the COVID-19 vaccine. Among those who paid attention (including often, sometimes or seldom) to the vaccine, information was almost attained via the internet (96.1%), followed by TV programs (39.6%), communication with relatives and friends (14.7%), expert lectures (11.2%). A majority (88.3%) participants showed preference to domestic vaccines. Over half of the participants thought COVID-19 pandemic had moderately severe or severe impact on clinical attendance or ART collection (56.9%)/immunity (58.0%)/discrimination and inequity (58.4%)/other psychologic disruptions (52.7%). See .
Table 2. Knowledge of and attitudes toward COVID-19 pandemic and COVID-19 vaccine among HIV-infected MSM in China, stratified by degree of vaccine hesitancy
Reasons to initiate COVID-19 vaccination or not
One hundred and thirteen (8.7%) had at least one dose of any COVID-19 vaccine. A total of 1182 participants did not initiate the COVID-19 vaccination, shows the reasons to initiate the COVID-19 vaccination. Over two-thirds (67.3%) participants regarded vaccination as self-health protection, the same percentage with participants regarded vaccination as trust in domestic medical technology. Just under half (49.6%) of participants had been vaccinated because they thought SARS‑CoV‑2 may exacerbate preexisting diseases. Seven (6.2%) participants had participated in vaccination programs organized at workplace. Moreover, 18 (15.9%) participants had no special reasons.
Figure 1. Reasons to initiate (A) and not to initiate (B) COVID-19 vaccination among HIV-infected MSM in China.
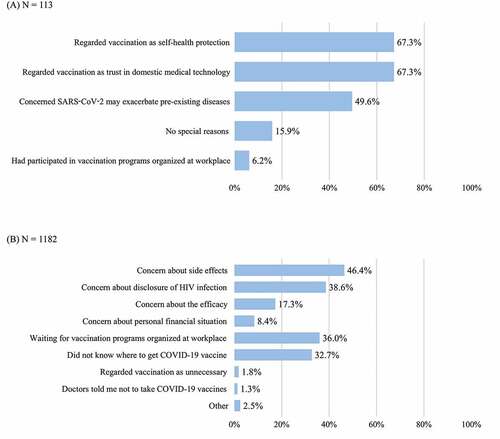
Reasons not to initiate the vaccination are depicted in . The top two reasons were concern about side effects (46.4%) and disclosure of HIV infection (38.6%), then the efficacy (17.3%) and personal financial situation (8.4%). Exception from all reasonable concerns above, waiting for vaccination programs organized at workplace and unawareness of where to get COVID-19 vaccine were also hinders, chosen by 384 (36.0%) and 378 (32.7%) participants. Besides, very few regarded vaccination as unnecessary (1.8%) or were told by doctors not to take COVID-19 vaccines (1.3%).
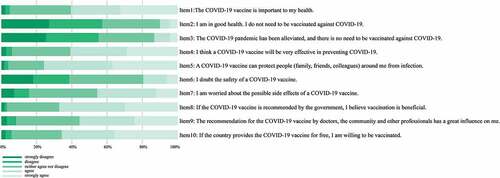
Vaccine hesitancy
The median value of VHS scoring was 2.4. Proportion of degree of vaccine hesitancy (lower or higher) was 52.8% vs 47.2%. The distribution of each item of VHS is depicted in . At least one-tenth of participants agreed or strongly agreed with the statement that it is unnecessary to be vaccinated because self was in good health (item 2, 10.0%) and alleviated pandemic (item 3, 13.1%). Of note, over three-fifths of participants believed in the efficacy of COVID-19 vaccines (item 4, 60.8%) and the vaccine can protect people around them from infection (item 5, 75.7%). More than two-thirds had belief in government’s vaccination recommendation (item 8, 67.2%). Over half believed suggestions made by health care professionals had an influence on their decision-making (item 9, 55.7%).
Figure 2. View on each item of the Vaccine Hesitancy Scale among HIV-infected MSM in China (N = 1182).
Correlates of COVID-19 vaccine hesitancy
In multivariable logistic regression analysis (Y: degree of vaccine hesitancy, 0 = lower hesitancy and 1 = higher hesitancy), lower COVID-19 hesitancy was associated with high ART adherence (aOR 0.53, 95% CI 0.35–0.80), often (0.26, 0.17–0.40) or sometimes (0.46, 0.31–0.67) paying attention to information about the COVID-19 vaccine, preference toward domestic vaccines (0.37, 0.24–0.59), perceived moderate (0.58, 0.38–0.90) and moderately severe or severe impact (0.54, 0.38–0.78) of SARS-CoV-2 on immunity, waiting for vaccination programs organized at workplace (0.60, 0.44–0.81) and unawareness of where to get COVID-19 vaccine (0.61, 0.45–0.82). Degree of vaccine hesitancy were positively correlated with concern about the efficacy (1.72, 1.16–2.54) and side effects (2.44, 1.78–3.35) of the COVID-19 vaccine. See .
Table 3. Correlates of COVID-19 vaccine hesitancy among HIV-infected MSM in China
Discussion
Overall, the COVID-19 vaccine uptake among HIV-infected MSM in mainland China was 8.7%. A total of 1182 participants did not vaccinate in this survey. Proportion of participants with lower and higher vaccine hesitancy were 52.8% vs 47.2%. Our findings demonstrated that primary correlates of COVID-19 vaccine hesitancy were vaccine-attribute factors (i.e., preference for domestic vaccines, concern about the efficacy and side effects of vaccine) and factors relevant to HIV infection (i.e., ART adherence and COVID-19 impact on immunity). Thus, this study suggests that there is an urgent need to make tailored strategies to alleviate vaccine hesitancy.
Health awareness is an essential motivation. Individuals who thought the pandemic had at least moderate impact on immunity were less hesitant about the vaccine. Moreover, some ART-related topics are associated with vaccine hesitancy. In this survey, high ART adherence was negatively associated with degree of vaccine hesitancy. View on “can ART prevent COVID-19” may also influence vaccine hesitancy, although this variable did not show statistical significance while entering into logistic regression model. Advice about the role of ART in preventing or treating COVID-19 has not reached a consensus.Citation28 If unvaccinated HIV-infected individuals regard antivirals as a useful prophylactic or regard COVID-19 vaccines as interference in previous antiretroviral medications, it may influence decision on COVID-19 vaccination. Also, health awareness can be influenced by a personal threat, which can be explained by the term “complacency” caused by low self-perceived risk of vaccine-preventable diseases.Citation11 Due to timely action and united effort to contain the epidemic, China has entered the stage of “regular epidemic prevention and control” where work, study and life of civils has been orderly resumed. They regarded this condition as a symbol of safety consequently became vaccine non-adaptors. Hence, immunization work from public health institutions should shed light on altruism and the benefit of herd immunity.Citation29 Then COVID-19 vaccination can be facilitated as a social responsibility.Citation30
The phenomenon of vaccine hesitancy is common. The WHO declared vaccine hesitancy was one of the top 10 global health threats in 2019.Citation31 Regarding the COVID-19 vaccine, concerns about the efficacy and side effects hindered the expansion of vaccination in this survey. This is understandable because vaccine-specific issues were most frequent cited determinants in vaccine hesitancy.Citation13 Besides COVID-19 vaccines, vaccine hesitancy also appeared with other types of vaccines applied among HIV-infected individuals. Common reasons not to initiate the vaccination including concerns about side effectsCitation32 and lack of expected efficacy.Citation33 In addition, for HIV-infected individuals, they may worry that the vaccine would further worsen their immune system.Citation32 Even if taking ART, some parameters such as increased CD8 T cells and lymphocytic exhaustion cannot be fully normalized and long-term antibody production and decreased responses to neoantigens or recall antigens may develop a potential threat to COVID-19 vaccine response.Citation34 Considering insufficient data on HIV-infected individuals included in approved phase 2 and 3 COVID-19 vaccine trials,Citation34 it is vital to carry out rigorous vaccine testing and offer efficacious evidence in a transport way to maintain public trust and relieve vaccine hesitancy.
We started this online survey on 13 February 2021, which was 1 month later than the initiation of national free vaccination policy.Citation6 Of note, before implementing such a policy, priority of vaccination had been given to high-risk populations,Citation4 but there was no guidance on COVID-19 vaccination for people with immunodeficiency or immune disorders.Citation35 In our study, nearly one-tenth participants (8.7%) were vaccinated under such circumstances. According to an interview with Dr. Nanshan Zhong 30 March 2021, only about 4.0% of people in China received at least one dose against COVID-19.Citation36 Primary reasons for vaccination were self-health protection (67.3%) and trust in domestic medical technology (67.3%). China disseminated COVID-19 related knowledge in a timely manner, and as a result public awareness reached a high level.Citation37 In addition, followers of Li Hui Shi Kong (an HIV-themed WeChat official account) are likely to have higher health literacy. The frequency of following information about the COVID-19 vaccine was a predictor of degree of vaccine hesitancy and the Internet was the most common media where they attained information about vaccine progress (96.1%). Information from social media is an important source of healthcare information,Citation38,Citation39 and those who at least sometimes paid attention to information about the COVID-19 vaccine may care more about preventive measures for health protection. There were also two phenomena worth considering. Participants who were waiting for organized vaccination at workplace or did not know where to get COVID-19 vaccine were less likely to have hesitancy. A possible explanation for the former group is that under the management of street committee staff, members in one company or organization are viewed as a unit to be vaccinated. Nevertheless, vaccination service was not widely available at the time of survey. Thus, waiting was more convenient. For the latter group, insufficient dissemination in their communities may be the main reason. Hence, optimal publicity of vaccine through social media may contribute to the COVID-19 vaccination program.
As of 29 March 2021, National Health Commission of the People’s Republic of China officially announced technical guideline for the inoculation of COVID-19 vaccines (1st version), offering vaccination advice for people with impaired immunity. Inactivated vaccines and the recombinant subunit vaccine are recommended; for the adenovirus vector vaccine, it is recommended that individuals are fully informed and fully consider the benefits and the risks before vaccination.Citation40 Expert recommendation on COVID-19 vaccination for HIV-infected adults, drafted by professionals from AIDS and Hepatitis C Professional Group, Chinese Society of Infectious Diseases has been published recently,Citation41 may also provide reliable suggestions for HIV-infected individuals. The vaccination should be delayed if there are clinical contraindications such as allergy to vaccine components and an HIV-infected individual does not start ART with diagnosed opportunistic infection/uncontrolled malignant rumor. The WHO and NIH both advise HIV-infected individuals should receive COVID-19 vaccines regardless of their CD4 or viral load status because the potential benefits outweigh potential risks.Citation42,Citation43 Policies or guidelines relevant to vaccination can provide reliable suggestions about COVID-19 vaccination and relieve possible concerns among HIV-infected individuals to some extent. Albeit the Chinese government set high vaccination coverage target, the Joint Prevention and Control Mechanism of the State Council of the People’s Republic of China emphasized that COVID-19 vaccination is not compulsory and should be implemented based on consent and voluntariness.Citation44 The majority of vaccine receivers were likely to take the vaccine based on their own decision.
Vaccines are considered as the only method to provide long-term immunity and prevent viral diseases.Citation45 Only by achieving an uptake rate of 70–80% of the entire population, can herd immunity be better realized and benefit everyone in the society. China’s goal was to achieve 60% uptake rate by the end of June 2021.Citation36 As of 18 Sep 2021, share of people fully vaccinated against COVID-19 in China was 78%.Citation46 Despite of such progress, we cannot lose attention about vaccination with the spread of new variantsCitation47 and the looming of resurgence.Citation48–51 Understanding factors associated with COVID-19 vaccine hesitancy among HIV-infected individuals from personal aspect (health awareness), vaccine aspect and national aspect (information dissemination and guidance making), making tailored measures would benefit the coverage of COVID-19 vaccination in this population.
There are several limitations in this study. First, a cross-sectional study design confines a causal conclusion so that we can only describe associations between degree of vaccine hesitancy and related factors. Second, this web-based survey was only conducted in mainland China, which may limit the generalizability of results. Third, information bias is unavoidable due to the self-reported information. However, data examination was set to exclude ineligible participants and ensure data quality.
Author contributions
This study was conceived and designed by Huachun Zou and Yong Cai in consultation with the other authors. Weiran Zheng and Hui Li were responsible for field study. Yinghui Sun and Heping Zhao were responsible for data compilation and data analysis. All authors have contributed to interpretation of data and study findings. Weiran Zheng, Yinghui Sun, Hui Li and Heping Zhao drafted the manuscript with all authors critically reviewing the paper.
Supplemental Material
Download ()Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2021.1996152
Additional information
Funding
References
- London School of Hygiene & Tropical Medicine. COVID-19 vaccine tracker. 2021 [accessed 2021 Jul 24]. https://vac-lshtm.shinyapps.io/ncov_vaccine_landscape/ .
- The Guardian. Covid-19 vaccine: who are countries prioritising for first doses? 2020 [accessed 2021 Mar 30]. https://www.theguardian.com/world/2020/nov/18/covid-19-vaccine-who-are-countries-prioritising-for-first-doses .
- Our World in Data. Coronavirus (COVID-19) vaccinations. 2021 [accessed 2021 Jul 24]. https://ourworldindata.org/covid-vaccinations .
- Xinhuanet. China vaccinating key groups against COVID-19. 2020 [accessed 2021 Apr 5]. http://www.xinhuanet.com/english/2021-01/04/c_139641409.htm .
- Reuters. China says will vaccinate ‘key groups’ over winter, spring. 2020 [accessed 2021 Apr 5]. https://au.news.yahoo.com/china-vaccinate-key-groups-over-045323011.html?guccounter=1&guce_referrer=aHR0cHM6Ly93d3cuZ29vZ2xlLmNvbS8&guce_referrer_sig=AQAAAMTFRQRAa_DjA0cjhqyjuMYpKoAdYDJq3_i-rYAQ57XV1SoYE7uzAH6qvS153cGZPRVFYyD9834wWVAmGb97JQsuAoq6HTo2J1ja7yL8E6L92v0NPY32mFach8d4_FOQp_OtDgOwIL9RuBFeEnsu5gbviTHgt7sNvfc05a6MiSWJ .
- The State Council of the People’s Republic of China. COVID-19 vaccination free to Chinese residents: official. 2021 [accessed 2021 Mar 26]. http://english.www.gov.cn/statecouncil/ministries/202101/09/content_WS5ff94558c6d0f72576943854.html .
- Basta NE, Moodie EMM; on behalf of the McGill University COVID19 Vaccine Tracker Team. COVID-19 vaccine development and approvals tracker. [accessed 2021 Sep 22]. https://covid19.trackvaccines.org/country/china/ .
- National Health Commission of the People’s Republic of China. Over 1.49 bln doses of COVID-19 vaccines administered in China. 2021 [accessed 2021 Jul 24]. https://en.nhc.gov.cn/2021-07/15/c_84159.htm .
- Chinese Center for Disease Control and Prevention. Interpretation of adverse effect monitoring information for national COVID-19 vaccination. 2021 [accessed 2021 Jun 3]. http://www.chinacdc.cn/jkzt/ymyjz/ymyjjz_6758/202105/t20210528_230908.html .
- Frederiksen LSF, Zhang Y, Foged C, Thakur A. The long road toward COVID-19 herd immunity: vaccine platform technologies and mass immunization strategies. Front Immunol. 2020;11:1817. doi:10.3389/fimmu.2020.01817.
- MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–64. doi:10.1016/j.vaccine.2015.04.036.
- Craxì L, Casuccio A, Amodio E, Restivo V. Who should get COVID-19 vaccine first? A survey to evaluate hospital workers’ opinion. Vaccines (Basel). 2021;9(3):189. doi:10.3390/vaccines9030189.
- Obregon R, Mosquera M, Tomsa S, Chitnis K. Vaccine hesitancy and demand for immunization in Eastern Europe and Central Asia: implications for the region and beyond. J Health Commun. 2020;25(10):808–15. doi:10.1080/10810730.2021.1879366.
- Iyengar KP, Vaishya R, Jain VK, Ish P. BAME community hesitancy in the UK for COVID-19 vaccine: suggested solutions. Postgrad Med J. 2021 [accessed 2021 Mar 29]: postgradmedj-2021-139957. doi:10.1136/postgradmedj-2021-139957.
- Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines (Basel). 2021;9(2):160. doi:10.3390/vaccines9020160.
- Wang W, Wu Q, Yang J, Dong K, Chen X, Bai X, Chen X, Chen Z, Viboud C, Ajelli M, et al. Global, regional, and national estimates of target population sizes for covid-19 vaccination: descriptive study. BMJ. 2020;371:m4704. doi:10.1136/bmj.m4704.
- Chen M, Li Y, Chen J, Wen Z, Feng F, Zou H, Fu C, Chen L, Shu Y, Sun C, et al. An online survey of the attitude and willingness of Chinese adults to receive COVID-19 vaccination. Hum Vaccines Immunother. 2021;17(7):2279–88. doi:10.1080/21645515.2020.1853449.
- Su Z, Wen J, Abbas J, McDonnell D, Cheshmehzangi A, Li X, Ahmad J, Šegalo S, Maestro D, Cai Y, et al. A race for a better understanding of COVID-19 vaccine non-adopters. Brain Behav Immun Health. 2020;9:100159. doi:10.1016/j.bbih.2020.100159.
- Finney Rutten LJ, Zhu X, Leppin AL, Ridgeway JL, Swift MD, Griffin JM, St Sauver JL, Virk A, Jacobson RM. Evidence-based strategies for clinical organizations to address COVID-19 vaccine hesitancy. Mayo Clin Proc. 2021;96(3):699–707. doi:10.1016/j.mayocp.2020.12.024.
- Laine C, Cotton D, Moyer DV. COVID-19 vaccine: promoting vaccine acceptance. Ann Intern Med. 2021;174(2):252–53. doi:10.7326/m20-8008.
- World Health Organization. COVID-19: vulnerable and high risk groups. 2021 [accessed 2021 Mar 26]. https://www.who.int/westernpacific/emergencies/covid-19/information/high-risk-groups .
- Ssentongo P, Heilbrunn ES, Ssentongo AE, Advani S, Chinchilli VM, Nunez JJ, Du P. Epidemiology and outcomes of COVID-19 in HIV-infected individuals: a systematic review and meta-analysis. Sci Rep. 2021;11(1):6283. doi:10.1038/s41598-021-85359-3.
- World Health Organization. WHO warns that HIV infection increases risk of severe and critical COVID-19. [accessed 2021 Sep 23]. https://www.who.int/news/item/15-07-2021-who-warns-that-hiv-infection-increases-risk-of-severe-and-critical-covid-19 .
- Bhaskaran K, Rentsch CT, MacKenna B, Schultze A, Mehrkar A, Bates CJ, Eggo RM, Morton CE, Bacon SCJ, Inglesby P. HIV infection and COVID-19 death: a population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet HIV. 2021;8(1):e24–e32. doi:10.1016/s2352-3018(20)30305-2.
- Jassat W, Cohen C, Tempia S, Masha M, Goldstein S, Kufa T, Murangandi P, Savulescu D, Walaza S, Bam JL, et al. Risk factors for COVID-19-related in-hospital mortality in a high HIV and tuberculosis prevalence setting in South Africa: a cohort study. Lancet HIV. 2021;8(9):e554–e567. doi:10.1016/s2352-3018(21)00151-x.
- Deeks SG, Overbaugh J, Phillips A, Buchbinder S. HIV infection. Nat Rev Dis Primers. 2015;1:15035. doi:10.1038/nrdp.2015.35.
- Sanchez TH, Zlotorzynska M, Rai M, Baral SD. Characterizing the impact of COVID-19 on men who have sex with men across the United States in April, 2020. AIDS Behav. 2020;24(7):2024–32. doi:10.1007/s10461-020-02894-2.
- Kanwugu ON, Adadi P. HIV/SARS-CoV-2 coinfection: a global perspective. J Med Virol. 2021;93(2):726–32. doi:10.1002/jmv.26321.
- Chou WS, Budenz A. Considering emotion in COVID-19 vaccine communication: addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020;35(14):1718–22. doi:10.1080/10410236.2020.1838096.
- Barello S, Palamenghi L, Graffigna G. Looking inside the “black box” of vaccine hesitancy: unlocking the effect of psychological attitudes and beliefs on COVID-19 vaccine acceptance and implications for public health communication. Psychol Med. 2021 [accessed 2021 Mar 8]:1–5. doi:10.1017/s003329172100101x.
- Trogen B, Oshinsky D, Caplan A. Adverse consequences of rushing a SARS-CoV-2 vaccine: implications for public trust. JAMA. 2020;323(24):2460–61. doi:10.1001/jama.2020.8917.
- Harrison N, Poeppl W, Herkner H, Tillhof KD, Grabmeier-Pfistershammer K, Rieger A, Forstner C, Burgmann H, Lagler H. Predictors for and coverage of influenza vaccination among HIV-positive patients: a cross-sectional survey. HIV Med. 2017;18(7):500–06. doi:10.1111/hiv.12483.
- Mohseni-Zadeh M, Rey D, Batard ML, Beck Wirth G, Partisani M-L, Lang J-M, Hansmann Y, Christmann D, Martinot M. Inadequate vaccination coverage in a French cohort of HIV positive patients. Med Mal Infect. 2010;40(12):683–90. doi:10.1016/j.medmal.2010.06.005.
- Ambrosioni J, Blanco JL, Reyes-Urueña JM, Davies M-A, Sued O, Marcos MA, Martínez E, Bertagnolio S, Alcamí J, Miro JM. Overview of SARS-CoV-2 infection in adults living with HIV. Lancet HIV. 2021;8(5):e294–e305. doi:10.1016/s2352-3018(21)00070-9 .
- ChinaDaily. Govt spells out groups not eligible for vaccination. 2021 [accessed 2021 Apr 15]. https://www.chinadaily.com.cn/a/202101/04/WS5ff26f41a31024ad0baa0342.html .
- Phoenix New Media. Exclusive|Zhong Nanshan calls for vaccination: don’t wait until foreign countries are immunized, China is dangerous. [accessed 2021 Apr 25]. https://v.ifeng.com/c/852HTO12J6W .
- National Health Commission of the People’s Republic of China. Health awareness among Chinese people rises in 2020. 2021 [accessed 2021 Apr 5]. http://en.nhc.gov.cn/2021-04/02/c_83377.htm .
- Benis A, Khodos A, Ran S, Levner E, Ashkenazi S. Social media engagement and influenza vaccination: a survey during the COVID-19 pandemic. J Med Internet Res. 2021;23(3):e25977. doi:10.2196/25977.
- Zeballos Rivas DR, Lopez Jaldin ML, Nina Canaviri B, Portugal Escalante LF, Alanes Fernández AMC, Aguilar Ticona JP. Social media exposure, risk perception, preventive behaviors and attitudes during the COVID-19 epidemic in La Paz, Bolivia: a cross sectional study. PLoS One. 2021;16(1):e0245859. doi:10.1371/journal.pone.0245859.
- National Health Commission of the People’s Republic of China. Technical guideline for the inoculation of COVID-19 vaccines. 2021 [accessed 2021 Apr 5]. http://en.nhc.gov.cn/2021-04/01/c_83365.htm .
- AIDS and Hepatitis C Professional Group, Chinese Society of Infectious Diseases. Expert recommendation for novel severe acute respiratory syndrome coronavirus 2 (SARS_CoV_2) vaccination in patients with HIV infection. Chin J Intern Med. 2021. doi:10.3760/cma.j.cn112138.20210403-00259.
- World Health Organization. WHO’s science in 5 on COVID-19: HIV & COVID-19. [accessed 2021 Sep 22]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/media-resources/science-in-5/episode-48—hiv-covid-19?gclid=Cj0KCQjwqKuKBhCxARIsACf4XuEmSRVHWk7zUgp-fibKSZp2PF5_XP8gHQT5z13ceWJESnUENtCzq8IaAnduEALw_wcB .
- HIV.gov. Interim guidance for COVID-19 and persons with HIV. [accessed 2021 Sep 22]. https://clinicalinfo.hiv.gov/en/guidelines/covid-19-and-persons-hiv-interim-guidance/interim-guidance-covid-19-and-persons-hiv?view=full .
- Press conference of the Joint Prevention and Control Mechanism of the State Council. Introduction of the situation regarding further prevention and control of the COVID-19 and vaccination on September 7, 2021. [accessed 2021 Sep 22]. http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11400&gecstype=1 .
- Trovato M, Sartorius R, D’Apice L, Manco R, De Berardinis P. Viral emerging diseases: challenges in developing vaccination strategies. Front Immunol. 2020;11:2130. doi:10.3389/fimmu.2020.02130.
- Xinhuanet. The number of people covered by COVID-19 vaccination have reached 1.1 billion in China, over 1 billion people complete the entire vaccination process. [accessed 2021 Sep 22]. http://m.news.cn/2021-09/19/c_1127881191.htm .
- Gómez CE, Perdiguero B, Esteban M. SARS emerging -CoV-2 variants and impact in global vaccination programs against SARS-CoV-2/COVID-19. Vaccines (Basel). 2021;9(3):243. doi:10.3390/vaccines9030243.
- Shimizu K, Wharton G, Sakamoto H, Mossialos E. Resurgence of covid-19 in Japan. BMJ. 2020;370:m3221. doi:10.1136/bmj.m3221.
- Agut H. COVID-19, September 2020: fall storm warning. Virologie (Montrouge). 2020;24(6):361–67. doi:10.1684/vir.2020.0865.
- Devi S. COVID-19 resurgence in Iran. Lancet. 2020;395(10241):1896. doi:10.1016/s0140-6736(20)31407-0.
- Zhang K, Vilches TN, Tariq M, Galvani AP, Moghadas SM. The impact of mask-wearing and shelter-in-place on COVID-19 outbreaks in the United States. Int J Infect Dis. 2020;101:334–41. doi:10.1016/j.ijid.2020.10.002.

