ABSTRACT
Dental caries is considered the third most important scourge in the world. In North America, Inuit populations are the population the most severely affected by dental caries. It is often assumed that this situation can be explained by a combination of factors classical for Indigenous populations: remoteness (geographical distance), low economic status and low health literacy (cultural distance). Using a bibliographic approach, we tested this hypothesis of the “distance effect” by exploring the caries prevalence in other Indigenous populations living in high-income countries. Next, we tested whether the high prevalence of caries is due to population-specific characteristics by tracking caries prevalence over the past few centuries. In result, we showed that while other Indigenous populations are more impacted by caries than the general populations, the Inuit populations present the highest prevalence. Paradoxically, we showed also that past Inuit populations were almost immune to caries before 1950. These two elements suggest that the prevalence of caries observed presently is a recent maladaptation and that beyond the effect of cultural and geographical distance, specific biocultural factors have to be investigated.
Introduction
Dental caries is considered the third most important scourge in the world by the WHO [Citation1]. It is one of the most universal diseases and most humans are affected at least once in their lifetime [Citation2]. Dental caries is characterised by a softening of the hard tissues of the tooth and evolve into a cavity due to the production of acids by bacteria in contact with sugars [Citation3]. These cavities are painful and disabling for eating and speaking. Often neglected and underestimated, painful cavities have an important impact on overall health by altering eating, attention, sleep, mood and social relationships. Most importantly, if left untreated, dental caries can lead to death from sepsis [Citation4,Citation5]. Therefore, dental caries is a critical global health issue, especially in areas where dental care is not readily available, such as in circumpolar areas [Citation6,Citation7].
In North America, Inuit populations are more severely affected by dental caries than the rest of the population in Canada and the United States [Citation6–9]. For example, the prevalence of caries in Inuit children aged 3 to 5 is estimated at 85.3% in the Nunavut region [Citation6]. Because Inuit children are affected by dental caries from an early age, their treatment often requires general anaesthesia which increases the risk of oral care [Citation10,Citation11]. Due to their geographic location, the high level of dental caries poses significant challenges for Canada and the United States [Citation10]. It is therefore particularly important to identify why circumpolar populations present a higher prevalence of dental caries than the rest of the populations.
Since the causes of caries are considered universal, only a few studies have focused on the specific risk factors of Inuit populations. However, the risk factor for caries depends greatly on the way of life. For example, in the populations of European ancestry, dental caries was moderately frequent for a few thousand years until the prevalence increased considerably after the industrial revolution and the abundant consumption of industrial sugars [Citation5,Citation12]. Very recently, the severity of dental caries has decreased in these populations due to considerable efforts in prevention [Citation13–15]. In circumpolar regions, the evolution of caries prevalence is not as well known. But it has been assumed that the high prevalence of caries is due to the fact the prevention effort might have been less efficient due to geographic and cultural distances. Indeed, it is well documented that populations living in areas geographically distant from the health system and/or with low health literacy and/or low economic status are particularly prone to poor health conditions [Citation16–18]. Such populations are also more affected by caries than the rest of the population of the countries where they live due to a cultural gap and a lack of impact of adapted prevention policies [Citation19].
Therefore, one could hypothesise that circumpolar populations who have an original culture, a different language and a lower income than the rest of the population could be subject to this “distance effect”. Other hypotheses can be proposed for instance that specific cultural or biological risk factors may play a role in the differences in caries prevalence between populations. For example, there is population variation in salivary microbiome or tooth mineralisation [Citation20,Citation21]. In Greenland, Inuit populations have larger molars, a higher frequency of shovel-shaped incisors, and a greater absence of the third molar and Carabelli tubercle than European populations [Citation22].
In this article, we intended to explore these two hypotheses based on a bibliographic approach. Firstly, we hypothesised that if the “distance effect” explains the high caries prevalence in Inuit populations then we should find a similar high prevalence in Indigenous populations now living in high-income countries resulting from European colonisation (Australia, Canada, New Zealand and the United States). Secondly, we hypothesised that if the high caries prevalence is due to population-specific characteristics, the high prevalence of caries might be ancient could be observed by tracking the caries prevalence across the last centuries.
Methods
Severity of dental caries in Inuit populations and comparison with indigenous populations and general populations: literature review of the oral health of indigenous populations
We compared severity of dental caries of Inuit populations with indigenous populations and general populations of four countries, Australia, Canada, New Zealand and the United States. We focused on similar western industrialised and democratic countries where indigenous populations and populations of European ancestry still cohabit and where medical research is similarly developed.
We extracted DMFT indices of the general population of these countries from the World Health Organization’s epidemiological database on dental caries [Citation23]. A DMFT index is the number of teeth decayed, missing or filled in 12-year-old children and ranges from 0 to 28 (wisdom teeth are not counted). This index was chosen in this study because it is the most commonly used measure to compare the severity of dental caries in the world [Citation24].
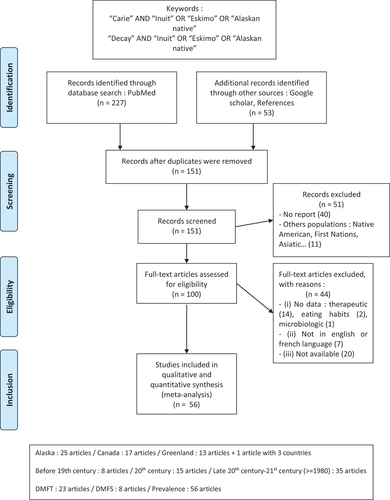
For the indigenous populations, we then performed a literature review () to collect epidemiological data on dental caries in Aboriginal populations in Australia, Inuit and First Nation populations in Canada, Alaskan Native and Native American populations in the United States, and Maori populations in New Zealand. On the PubMed bibliographic data search engine, we used the keywords “oral health”, “dental caries/caries” and “tooth decay” associated with the keywords “Aboriginal” and “indigenous Australia” or “Maori” and “indigenous New Zealand” or “Alaskan Native”, “Inuit”, “Native American” and “First Nation”. We identified 1,955 publications from this research, which was reduced to 828 by removing the duplicated items.
Figure 1. Prisma 2009 flow diagram for selecting studies on dental caries in indigenous populations in Australia, Canada, New Zealand and the United States.
From the 828 references obtained in the bibliographic research, 315 articles were selected based on the abstracts. To be selected, an article had to (i) concern indigenous populations, (ii) concern oral health.
We chose to include only recent articles on the DMFT index of children aged 12 ± 4 years to make the data comparable with WHO dataset. Therefore, we limited our study to articles which (i) include a DMFT index, (ii) concern children between the ages of 8 and 16, and (iii) date between 1980 and 2018. Forty-seven [Citation25] articles were finally included in the study.
Data was extracted from the 47 relevant articles and analysed using R software and ggplot library [Citation26,Citation27]. We applied the Student test to the results to compare the caries rate between the general population and the indigenous population for each country.
Evolution of prevalence of caries in Inuit populations: historical literature review of oral health of Inuit populations
To focus on the oral health of Inuit populations, we studied the evolution of dental caries in these populations, from the 11th century to the 21st century.
We conducted a historical literature review of dental caries in Inuit populations. In this historical literature review, we included on the Arctic populations of Canada, called “Inuit”; of the United States, called “Alaskan Natives”; and of Greenland, called “Kalaallit”.
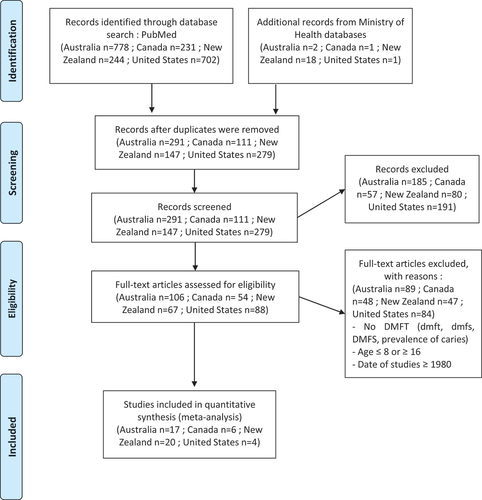
We performed a bibliographic search on PubMed search engine and other sources with the keywords “oral health”, “dental caries/caries” and “tooth decay” associated to the keywords “Alaskan Native”, “Eskimo”, “Inuit” and “Greenland”. We also performed another search with the keywords “archeological”, “prehistoric”, “mummies” associated with the keywords “Alaskan Native”, “Eskimo”, “Inuit” and “Greenland” (). We identified 280 publications from this research, which was reduced to 151 by removing the duplicated items.
From the 151 publications identified, 100 articles were selected. To be selected, an article had to (i) concern Inuit populations, (ii) concern teeth or oral health.
Finally, 56 articles were included based on different inclusion criteria. To be included, an article had to (i) include the prevalence or DMFT of caries, (ii) be in French or in English concern adults, (iii) be accessible.
We had data concerning Inuit populations of Alaska in 25 articles, of Canada in 17 articles and Greenland in 13 articles. Only one article concerns the three regions. These data are distributed over the time, with 8 articles before the 19th century, 15 articles in the 20th century and 35 articles in the late 20th century and the 21st century.
We extracted prevalence of dental caries of Inuit populations over time, from the 56 relevant articles and analysed. The prevalence is the percentage of individuals with at least one cavity in a population. We found the DMFT of dental caries in 23 articles.
Results
In order to better understand the severity of dental caries in Inuit populations, we compared the DMFT in these populations with other indigenous populations with a hunter-gatherer past and general populations of similar western and industrialised countries in which indigenous populations and general populations cohabit.
In all countries studied, we observed the same pattern with indigenous populations more impacted. In Australia, Aboriginal populations presented a significantly higher DMFT than the general population of Australia (p-value <0.001), 1.90 for Aboriginal populations versus 1.06 for the general population. Similarly, in New Zealand, Māori populations also presented a higher DMFT than the general population i.e 1.86 compared to 1.28 for the general population (p-value >0.05). In Canada, Inuit population had a significantly higher DMFT of 7.22, four times higher than that of the general population of Canada, which is 1.72 (p-value <0.001). First Nations also had a significantly higher DMFT than the general population (p-value <0.001), 5.36 for Natives versus 1.72 for the general population. Finally, in the United States, Alaskan Natives and Native Americans had a significantly higher DMFT of 3.21, nearly three times higher than that of the general population of the United States, which is 1.27 (p-value <0.001). For Native Americans alone, their DMFT is significantly higher than the general population (p-value <0.05), 2.88 for Native Americans against 1.27 for the general population.
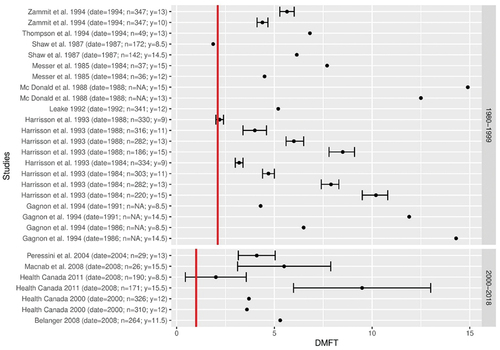
Globally, 87.21% of the studies showed/demonstrated that indigenous populations are more severely affected by dental caries than the general population (). Since dental caries prevalence fluctuates according to time, we took this factor in account in a new analysis splitting the dataset in two (before and after the y. 2000). For studies published between 1980 and 1999 : 91.52% of the studies reported that, indig enous populations had higher rates of DMFT than the corresponding general populations. Similarly, in the 21st century 84.96% of studies on indigenous populations also reported higher rates of DMFT (2000–2018). 87.21% of the studies showed that indigenous populations are more severely affected by dental caries (). This is not due to a bias in the year of study since 91.52% of the studies reported that, in each country, indigenous populations had higher rates of DMFT than the corresponding general populations between 1980 and 1999; and 84.96% of studies on indigenous populations also reported higher rates of DMFT in the 21st century (2000–2018).
Figure 3a. Forest plot of DMFT (number of decayed, missing and failed teeth) in indigenous populations compared to the DMFT in the general populations (red line) of Australia, over two periods, between 1980 and 1999 and between 2000 and 2018, based on a systematic review of the literature.
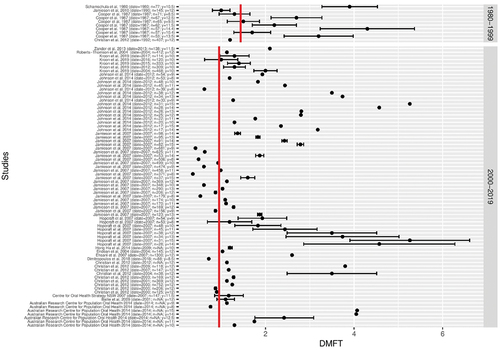
Figure 3c. Forest plot of DMFT (number of decayed, missing and failed teeth) in indigenous populations compared to the DMFT in the general populations (red line) of New Zealand, over two periods, between 1980 and 1999 and between 2000 and 2018, based on a systematic review of the literature.
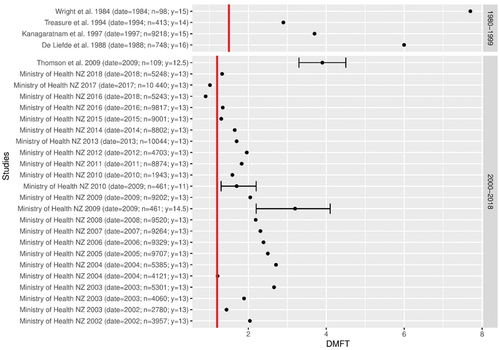
Figure 3d. Forest plot of DMFT (number of decayed, missing and failed teeth) in indigenous populations compared to the DMFT in the general populations (red line) of the United States, over two periods, between 1980 and 1999 and between 2000 and 2018, based on a systematic review of the literature.
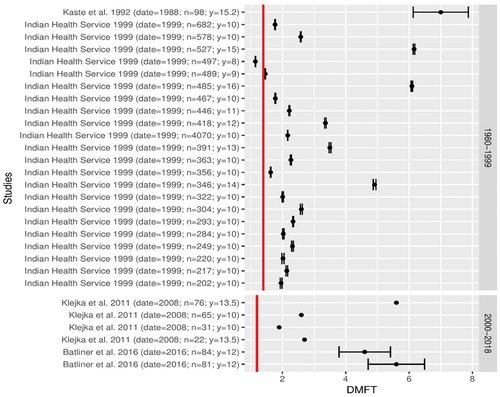
For the indigenous populations of Canada and the United States, 96.55% of the studies showed that indigenous populations have more cavities than the general populations (). American Indians, Alaskan Natives, First Nations and Inuit are the populations most severely affected by dental caries in industrialised countries (). This difference is particularly striking for the indigenous populations of Canada. Inuit in Canada have a DMFT of 7.22, which is four times higher than for the general Canadian population which has a DMFT of 2.5. Therefore, these Inuit populations have the worst DMFT index of all the populations compared. Based on WHO dataset on all populations worldwide, Inuit populations are among the populations with the highest level of DMFT.
Figure 4. Box plot of DMFT (number of decayed, missing and failed teeth) in indigenous populations and the general populations of Australia Canada, New Zealand and the United States between 1980 and 2018, based on a systematic review of the literature.
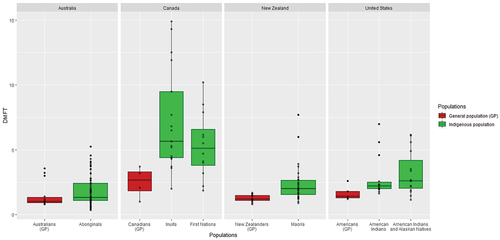
Figure 3b. Forest plot of DMFT (number of decayed, missing and failed teeth) in indigenous populations compared to the DMFT in the general populations (red line) of Canada, over two periods, between 1980 and 1999 and between 2000 and 2018, based on a systematic review of the literature.
In order to understand the origin of this high severity of dental caries in these populations, we retraced the historical evolution of dental caries in Inuit populations based on a literature review of 56 articles with epidemiological data on Inuit populations from the archaeologic period to the 21st century. In this present study, we named “Inuit” the Arctic populations of Canada; “Alaskan Natives” the Arctic populations of the United States; and “Kalaallit” the Arctic populations of Greenland. In 1977, the term “Inuit”, which means “man” in the Inuit language, was adopted by the majority of Arctic populations during the creation of the Inuit Circumpolar Conference, a group whose objective of obtaining greater autonomy and defending the interests of Arctic populations [Citation28,Citation29].
On the 56 articles, 5 are archaeological reports describing the population living between 950 to 1900. All these archaeological reports show a prevalence of caries less than 1%. For instance, Pedersen counted 5 cavities on the 526 skeletons of Kalaallit from Greenland and their 7606 teeth, dating from the 1700s [Citation30]. A study by Mayhall of 1970 reported 2 cavities on the 301 Inuit skeletons dating between 900 and 1650 [Citation31]. Gessain collected 15 skulls from the Ammassalik district in Greenland, dating before 1884. Gessain did not note cavities on the skulls [Citation32].
Early epidemiological studies confirmed that Inuit populations were little affected by caries until the middle of the 20th century. Nine studies in Greenland and Alaska showed that Inuit have a prevalence of caries between 0 and 20%, at the beginning of the 19th century, until the 1930’s ( [Citation30–38]. In Greenland, a study conducted in 1934–1935 by Gessain [Citation39] focused on the Kalaallit during this period of contact with the Danes. Among men, 7 individuals had caries out of 302, i.e. a prevalence of caries of 2.6. Among women, there are 17 individuals with caries out of 325, i.e. a prevalence of 5.2%. Before the contact with the Danes, in the same village of Angmagssalik, Poulsen had found no dental caries in 47 Kalaallit in 1898 [Citation39].
Figure 5. Evolution of the prevalence of caries (%) in the Inuit populations of Canada, Greenland and the United States between 900 and 2008, based on a historical review of the literature.
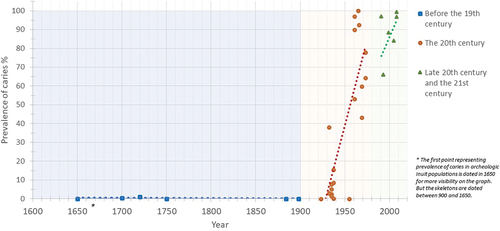
From this point, this prevalence increased to exceed 50% until reaching 90 to 100% in the 1970’s ( [Citation31,Citation32,Citation40,Citation41]. Two longitudinal studies illustrated this increase in prevalence in 1950’s. In the United States, 90 Alaskan Natives of the Nunamiut community, previously free of caries, developed cavities within 8 years, between 1957 and 1965 [Citation41]. Between 1955 and 1957, the dft was 3 and the DMFT was 0.8, and the natives over 30 years of age had a prevalence of caries of 0%. From 1965 onwards, 8 years later, the dft was 5.6 and the DMFT index increased to 3.1 and the natives had a prevalence of 100% [Citation41]. In Canada, Mayhall reported an increase in prevalence of caries between 1969 and 1973 in two Inuit communities in Igloolik and Hall Beach. In Igloolik, the prevalence of caries increased from 59.7% to 77.9% in only 4 years, while in Hall Beach, the prevalence increased from 43.1% to 64.2% [Citation31].
In the late of the 20th century and in the 21st century, 35 studies showed that the prevalence of caries in Inuit populations increased considerably, almost 90% [Citation42] and from the end of the 20th century, Inuit populations had higher indices than the general populations of their country. In the 1980s, 97% of Inuit had cavities compared to 50% for Canadians [Citation42]. In the United States, a 1987 study found that the prevalence of caries among Alaskan Natives aged 3 to 5 years was 44 to 85% compared to 5 to 11% for Americans [Citation43]. In the 21st century, in the United States, the Native Americans and the Alaskan Natives aged 3 to 5 had a DMFT three to four times more high than American children of European descent [Citation7]. In Greenland, the DMFS 15-year-old Kalaallit children was 9.2 in 2008, while it was only 2.3 for Danish children [Citation9].
The increase in cultural contact with other populations and the transition from a traditional diet high in proteins to an industrial diet high in sugars have been associated to the increase in dental caries [Citation22,Citation38]. The speed of the transition was emphasised by Bang et al. [Citation41], who showed that in some Inuit populations, in 10 years, the total percentage of calories obtained from proteins decreased by 50% while carbohydrates increased by 50%. Interestingly, while there are various factors which impact caries prevalence, the review of literature suggested that the impact of key factors for caries changed during the 20th century in the Inuit populations. For example, a low socio-economic level, a low exposure to European education or life in rural areas were protective factors for dental caries in Inuit populations in the middle of the 20th century [Citation39] []. These populations had a traditional diet rich in protein and did not have financial, cultural and geographical access to industrial food. While in the 21st century, these same factors are aggravating factors, because access to prevention programmes and health care is difficult for Inuit populations living in isolated areas and with a low socio-economic level resulting in lack of dental insurance, lack of affordability of oral hygiene supplies and lack of healthy foods [Citation6,Citation43,Citation44]. Given that this finding (previously protective factors becoming aggravating) is based on the study of limited historical sources, in the face of a global phenomenon over a vast and diverse area, we suggest that this hypothesis should be further investigated to confirm (or refute) it, and ultimately better understand the causes of caries prevalence in these populations.
Table 1. Comparison and evolution of the risk factors for caries in Inuit populations protective factors (+) and harmful factors (-) in Inuit populations in the 21th century and in the 20th century, and in general populations.
To summarise, Inuit populations were almost unaffected by cavities, until the first half of the 20th century. Alaskan Natives had a DMFT close to 1 and a prevalence of caries of 0% for adults and Inuit in Canada had a DMFT of 2 and a prevalence of caries less than 10%. In a few decades, starting in the second half of the 20th century, dental caries increased dramatically in these populations. In Alaska, the DMFT multiplied by 3 in 10 years and the prevalence of caries reached 100%. In Canada, the DMFT multiplied by 10 and the prevalence of caries is also close to 100%. In the middle of the 20th century, Inuit populations started interacting with Populations of European ancestry and a few years of contact were enough to drastically change the oral health of these populations.
Discussion – conclusion
Our study has shown that indigenous populations living in Western countries are significantly more affected by caries than the general population of the same countries. In line with our original hypothesis, this shared high prevalence of caries suggested a common element that unites these populations. It is important to note that Aboriginal, Maori, Inuit and Native American populations have very different genetic backgrounds, live in very different environments and have very different histories and cultures. What they do have in common is that they were only “recently” in contact with European populations and they are culturally as well as sometimes geographically distant from the general population of these countries. Importantly, we have shown that Inuit populations are more affected by caries than other indigenous populations in the study. It should be noted that, like the Inuit populations, the First Nations are also still highly affected by caries. The prevalence of caries in this population has risen from 0 to 100% for the over 30s in just 10 years [Citation41]. It should be noted that during this contact phase and contrary to today, it has been observed that the “distance effect” (cultural and/or geographical) plays a protective role. Indeed, the more individuals or populations keep a traditional lifestyle and diet, the less they are affected by caries. It is therefore very likely that the high prevalence of caries is a maladaptation of the Inuit populations with this new diet. It is important to note that this phenomenon took place within a generation. Thus, the people who lived through this transition saw a very painful and then unknown disease gradually affect all the individuals in the community, starting with the children. So there were no or few traditional responses. This is very different from populations of European origin where the prevalence of caries has increased in stages since the adoption of agriculture in the Neolithic period. The factors contributing to this disease may have environmental roots, it is vital to pinpoint traits specific to Arctic populations. In future research, investigating the historical prevalence of caries among the Sami populations in Scandinavia, for instance, could shed light on the matter. The Sami community grapples with a severe caries burden, exhibiting a higher DMFT than the general population of their country [Citation45]. Just like Inuit populations, the Sami have implemented local preventive programmes, yet challenges concerning healthcare accessibility persist [Citation46,Citation47]. Nonetheless, when compared to other indigenous groups, the Sami exhibit a lower DMFT and a prevalence close to that of the general population of their country [Citation45]. This underlines the significance of delving into the historical trajectory of caries prevalence among the Sami, as it may offer valuable insights into understanding their comparatively lower DMFT.
In each of these countries, the prevalence of the general population has recently decreased due to prevention efforts [Citation15,Citation23]. Our study reinforces the idea that the remoteness of Inuit populations currently makes modern preventive strategies less effective, and is at the root of the higher rate of caries in Inuit populations. Difficulties linked to cultural and geographical remoteness are well known and have already been documented [Citation6,Citation8,Citation9,Citation11,Citation25,Citation48,Citation49], particularly in the implementation of prevention policies (language barrier, traditional medicine, non-accepted prevention measures…) and in access to care (rural areas difficult to access, population dispersed over vast territories, lack of health professionals, poor water supply…). For example, water fluoridation is difficult in the Arctic region due to climatic conditions and the lack of water supply systems [Citation11,Citation25,Citation48,Citation49]. In Canada, in the Inuvik region, only the town of Inuvik is supplied with fluoridated water [Citation49]. In the United States, 30% of Alaskan villages have no piped water and only 8% of villages have a fluoridated water system compared to 72% of Americans [Citation27]. Fluoridated water is transported in trucks and distributed via cisterns in these regions, but the fluoridated water in these cisterns has a lower concentration of fluoride than that found in the piped water [Citation12]. Especially, fluoridated water is an important factor in the prevention of caries, decreasing caries rates by 30–50 [Citation25]. To alleviate the problem of water supply, in Greenland, the government established the sale of fluoridated salt in 2010, but due to the excessive price, we are unable to observe the effect of this measure [Citation9]. The cultural barrier complicated the study of new means of prevention, like a trial on xylitol chewing gum on pregnant Alaskan Native women which could not be carried out due to a lack of participants [Citation50]. In contrast, community-based interventions promising oral health developed within the communities with a local dental therapist are appreciated and showed to reduce the severity of caries. But these local prevention programmes require more staff and to train dental therapist in the community who would be more available, and high-risk subgroups require more intensive interventions and better access to health care [Citation50,Citation51]. Furthermore, access to health care is complicated in the Arctic. The smallness of villages and the dispersion of Inuit populations over a large territory do not allow a dentist to work full time [Citation8]. In Canada, some regions populated by Inuit are more deficient than others, 79% of Inuit in Inuvialuit received care compared to 38% in Nunatsiavut [Citation31]. In addition to the dispersion of the populations, some regions are difficult to access. In the Inuvik region of the Canadian Arctic, 10 of the 13 communities in the region are accessible only by air [Citation49]. Nevertheless, the present study underscores that the high rate of caries among Inuit populations is not an inevitable outcome. While these populations have been extensively affected in recent memory, they were immune to such conditions just a few generations ago. Awareness of this fact might boost motivation to launch of more specific studies on the subject and find innovative solutions.
Finally, these results suggest that unlike other populations, there may not have been ancient biological or cultural adaptations of Inuit populations to caries. It would be interesting to study whether genetic and biological characteristics such as enamel thickness, bacterial flora or dental morphology are more common predisposing factors in Inuit populations than in other indigenous populations. Understanding the biological and cultural predisposing factors would allow the implementation of patient-centred dentistry in Inuit populations and the adaptation of oral prevention policies in these populations.
Acknowledgments
We are very grateful to Mrs. Karen Anderson, Professor Carle Paul and Professor Catherine Nabet for the correction.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Institute of Health Metrics and Evaluation (IHME). Global burden of disease collaborative network. global burden of disease study 2019 (GBD 2019). 2020.
- Peres MA, Macpherson LMD, Weyant RJ, et al. Oral diseases: a global public health challenge. Lancet Lond Engl. 2019 juill 20;394(10194):249‑60.
- Selwitz RH, Ismail AI, Pitts NB. Dental caries. Lancet Lond Engl. 2007 janv 6;369(9555):51‑9.
- Bayetto K, Cheng A, Goss A. Dental abscess: A potential cause of death and morbidity. Aust J Gen Pract. 2020 sept;49(9):563‑7. doi: 10.31128/AJGP-02-20-5254
- Shetty A. Significance of sugar intake in young adults: a review. Int J Adolesc Med Health. 2021 oct 26;33(6):375‑8.
- Canada HC, Nunavut Tunngavik incorporated. Inuit oral health survey report, 2008-2009. Ottawa: Health Canada; 2011.
- Health Service I, Phipps K, Ricks T, et al. The 2010 Indian health service oral health survey of American Indian and Alaska native preschool children. Indian Health Serv Data Brief. 2013;31.
- Bolin KA. Assessment of treatment provided by dental health aide therapists in Alaska: a pilot study. J Am Dent Assoc. 2008 nov;139(11):1530‑5. 1939 discussion 1536-1539. doi: 10.14219/jada.archive.2008.0080
- Ekstrand KR, Qvist V. The impact of a national caries strategy in Greenland after 4 years. Int J Paediatr Dent juill. 2015;25(4):255‑66. doi: 10.1111/ipd.12138
- Atkins CY, Thomas TK, Lenaker D, et al. Cost-effectiveness of preventing dental caries and full mouth dental reconstructions among Alaska Native children in the Yukon–Kuskokwim delta region of Alaska. J Public Health Dent. 2016;76(3):228‑40. juin. doi: 10.1111/jphd.12141
- Curzon ME, Curzon JA. Dental caries prevalence in the Baffin Island Eskimo. Pediatr Dent. 1979 sept;1(3):169‑74.
- Hardwick JL. The incidence and distribution of caries throughout the ages in relation to the Englishman’s diet. Brit Dent J. 1960;108:9‑17.
- Holm AK. Caries in the preschool child international trends. J Dent. 1990 déc 1;18(6):291‑5.
- Petersson GH, Bratthall D. The caries decline: a review of reviews. Eur J Oral Sci. 1996;104(4):436‑43. doi: 10.1111/j.1600-0722.1996.tb00110.x
- Hillson S, Technique and Application in Dental Anthropology. The current state of dental decay. Disponible sur. 2008 cité 14 nov 2019; http://core/books/technique-and-application-in-dental-anthropology/current-state-of-dental-decay/F8428CC1D529CB4957165897DAD0FE28
- Ju X, Do L, Ha D, et al. Association of Modifiable risk factors with dental caries among indigenous and Nonindigenous children in Australia. JAMA Netw Open. 2019 mai 3;2(5):e193466.
- Northridge ME, Kumar A, Kaur R. Disparities in access to oral health care. Annu Rev Public Health. 2020 avr 2;41(1):513–12.
- Holve S, Braun P, Irvine JD, et al. Early childhood caries in indigenous communities. Pediatrics juin. 2021;147(6):e2021051481. doi: 10.1542/peds.2021-051481
- Levy BB, Goodman J, Eskander A. Oral healthcare disparities in Canada: filling in the gaps. Can J Public Health Rev Can Sante Publique. 2022 sept 23;114(1):139–145.
- Harris EF, McKee JH. Tooth mineralization standards for blacks and whites from the middle southern United States. J Forensic Sci. 1990 juill 1;35(4):859‑72.
- Nasidze I, Li J, Quinque D, et al. Global diversity in the human salivary microbiome. Genome Res. 2009 janv 4;19(4):636‑43.
- Pedersen PO. Dental investigations of Greenland Eskimos.[Summary.]. Proc R Soc Med. 1947 oct 1;40(12):726‑32.
- World Health Organization. Rapport sur la santé bucco-dentaire dans le monde 2003. 2003. p. 48.
- Broadbent JM, Thomson WM. For debate: problems with the DMF index pertinent to dental caries data analysis. Community Dent Oral Epidemiol déc. 2005;33(6):400‑9. doi: 10.1111/j.1600-0528.2005.00259.x
- Klejka J, S M, Whistler B, et al. Dental caries in rural Alaska Native children – Alaska 2008. MMWR Morb Mortal Wkly Rep. 2011 sept 23;60:1275‑8.
- R Core Team. R: a language and environment for statistical computing [Internet]. Vienna, Austria: R Foundation for Statistical Computing; 2017. Disponible sur https://www.R-project.org/
- Wickham H. ggplot2: elegant Graphics for data analysis [Internet]. New York: Springer-Verlag; 2016. doi: 10.1007/978-3-319-24277-4_9.
- Mailhot J. L’étymologie de « Esquimau » revue et corrigée. Etud Inuit. 1978;2(2):59‑69.
- Laugrand F Notre terre, le Nunavut. Vie Idées [Internet]. 22 déc 2011 [cité 1 nov 2019]; Disponible sur: http://www.laviedesidees.fr/Notre-terre-le-Nunavut.html
- Pedersen PO. Investigations into dental conditions of about 3,000 ancient and modern greenlanders. Am J Orthod Oral Surg. 1938;24(7):702‑4.
- Mayhall JT Cultural and environmental influences on the Eskimo dentition. • Arctic health. Pages 215-227 AA Dahlberg TM Graber Eds Orofac Growth Dev Mouton Hague [Internet]. 1977 [cité 2020 mars 8]. Disponible sur: https://arctichealth.org/en/permalink/ahliterature1599
- Gessain R, Plénot HR. La dentition des Ammassalimiut (Eskimo de la côte est du Groenland). Bull Mém Société Anthropol Paris. 1982;9(4):321‑32. doi: 10.3406/bmsap.1982.3867
- Leigh RW. Dental pathology of the Eskimo. Philadelphia: S.S. White Dental Manufacturing Co.; 1925 cité 2021 mai 10. [Internet] Disponible sur: http://name.umdl.umich.edu/0527912.0067.001
- Pedersen PO. Dental caries in Greenland 1935-1969. Pre-war Greenland and its population. Dtsch Zahnarztl Z. 1971 nov;26(11):1023‑7.
- Kirkeskov L, Kristiansen E, Bøggild H, et al. The association between fluoride in drinking water and dental caries in Danish children. Linking data from health registers, environmental registers and administrative registers. Community Dent Oral Epidemiol Juin. 2010;38(3):206‑12. doi: 10.1111/j.1600-0528.2009.00526.x
- Zitzow RE. The relationship of diet and dental caries in the Alaska Eskimo population. Alaska Med. 1979 mars;21(2):10‑3.
- Ritchie SG, Bagnell JS. The dentition of the western and central Eskimos. F.A. Acland • XII (book chapter). 1923;XII:59‑66.
- Collins HB. Caries and crowding in the teeth of the living Alaskan Eskimo. Am J Phys Anthropol. 1932;16(4):451‑62. doi: 10.1002/ajpa.1330160415
- Gessain R. La dentition des Eskimo d’Angmassalik ; génétique, croissance et pathologie. Bull Mém Société Anthropol Paris. 1959;10(4):364‑96. doi: 10.3406/bmsap.1959.2747
- Russell AL, Consolazio CF, White CL. Dental caries and nutrition in Eskimo Scouts of the Alaska national guard. J Dent Res. 1961 mai 1;40(3):594‑603.
- Bang G, Kristoffersen T. Dental caries and diet in an Alaskan Eskimo population. Scand J Dent Res. 1972;80(5):440‑4. doi: 10.1111/j.1600-0722.1972.tb00310.x
- Zammit MP, Torres A, Johnsen DC, et al. The prevalence and patterns of dental caries in Labrador Inuit Youth. J Public Health Dent. 1994;54(3):132‑8. doi: 10.1111/j.1752-7325.1994.tb01204.x
- Chi DL, Hopkins S, O’Brien D, et al. Association between added sugar intake and dental caries in Yup’ik children using a novel hair biomarker. BMC Oral Health. 2015 oct 9;15(1):121.
- Hussain A. Key challenges for indigenous peoples of Canada in terms of oral health provision and utilization: a scoping review. Int J Dent. 2022 sept 27;2022:e7511213. doi: 10.1155/2022/7511213.
- Bongo AKS, Brustad M, Jönsson B. Caries experience among adults in core Sámi areas of Northern Norway. Oral Epidemiol. 2021;49(5):401‑9. doi: 10.1111/cdoe.12613
- Holde GE, Oscarson N, Tillberg A, et al. Methods and background characteristics of the TOHNN study: a population-based study of oral health conditions in northern Norway. Int J Circumpolar Health. 2016 févr 19;75(1):10.3402/ijch.v75.30169.
- Brustad M, Sara Bongo AK, Hansen KL, et al. Oral health in the indigenous Sámi population in Norway - the dental health in the North study. Acta Odontol Scand. 2020 mars;78(2):98‑108. doi: 10.1080/00016357.2019.1654615
- Rea E, Thompson G, Moffatt ME, et al. Adult dental health in the Keewatin. J Can Dent Assoc. 1993 févr;59(2):117‑8, 122‑5.
- Leake J, Jozzy S, Uswak G. Severe dental caries, impacts and determinants among children 2-6 years of age in Inuvik region, Northwest Territories, Canada. J Can Dent Assoc août. 2008;74(6):519.
- Chi DL. Reducing Alaska Native paediatric oral health disparities: a systematic review of oral health interventions and a case study on multilevel strategies to reduce sugar-sweetened beverage intake. Int J Circumpolar Health InternetDisponible sur. 5 août 2013 [cité 7 nov 2019];72(1):21066. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3873640/.
- Mathu-Muju KR, McLeod J, Donnelly L, et al. The perceptions of first nation participants in a community oral health initiative. Int J Circumpolar Health. 2017;76(1):1364960. doi: 10.1080/22423982.2017.1364960