ABSTRACT
PURPOSE: To investigate the effects of SSRIs on cornea and lens density, intraocular pressure (IOP) and anterior chamber parameters, including anterior chamber volume (ACV), anterior chamber depth (ACD), corneal volume (CV) and central corneal thickness (CCT), in patients with depression during a three-month follow-up period.
METHOD: In this prospective study, 31 total patients, who were prescribed SSRIs for depression, were recruited. Sertraline, 50 mg/daily, was given to ten patients; 11 received Escitalopram, 10 mg/daily; and ten were treated with Fluoxetine, 20 mg/daily. The parameters recorded were corneal density (CD), lens density (LD), IOP, ACV, ACD, CV and CCT at the start of treatment, as well as at one-week, one-month, and three-month follow-ups.
RESULTS: The study revealed that there was no risk of cataract development from three months of SSRI intake. Significant decrease in ACD was recorded at the one-week follow up; however, after three months, this decrease was insignificant compared to the baseline. ACV, CV, CCT, CD and LD showed no significant alterations in any of the follow up examinations over the three-month period. IOP, however, significantly fell (a P value of 0.004).
CONCLUSION: In this study, SSRI use does not seem to be associated with an increased risk of cataract or glaucoma or with changes in CD and LD. Long-term follow-up is necessary to determine the actual risk of cataract or glaucoma with SSRI intake.
Introduction
Major depressive disorder (MDD) is the world's leading mental disorder, with the World Health Organization (WHO) reporting that more than three million people suffered from this disease in 2018 – a significant 18% rise in incidence from 2005 to 2015 [Citation1]. As a result of this rapid increase, antidepressant use has risen dramatically in many Western countries [Citation2].
Although the complex pathophysiology of MDD remains unknown, it has been suggested that dysfunction in adrenergic and/or serotonergic systems, which modulate a wide range of neurological processes, may lead to MDD development. Thus, inhibiting noradrenaline and/or serotonin reuptake has proven to be a clinically effective antidepressant treatment [Citation3].
Serotonin (5-hydroxytryptamine, 5-HT) is a biogenic monoamine, having multiple actions on the central and peripheral nervous systems. Therapeutic actions of selective serotonin reuptake inhibitors (SSRIs), based on presynaptic inhibition of the serotonin transporter, with an increased availability of serotonin in the synaptic cleft, lead to higher serotonin levels in the brain [Citation4].
After the FDA approved SSRI use for depression, anxiety and other mood disorders, such as the negative symptoms of eating disorders [Citation4], SSRIs became the most effective and most commonly prescribed drugs for MDD. It is estimated that approximately 10% of U.S. residents take antidepressants, mainly SSRIs, making antidepressants the third most commonly prescribed class of medication in the U.S[Citation5].
In addition to their desired effects, SSRIs may cause unwanted side effects requiring medical attention. The increasing use of SSRIs has necessitated new studies assessing their safety and adverse effects. However, the systemic side effects of this neurotransmitter – including weight gain, anxiety, insomnia, increased appetite, vertigo, nausea, sexual problems and itching – are not well researched in humans[Citation6], though some preliminary studies have been performed in animal models[Citation7].
SSRIs work by increasing serotonin levels in the brain, and serotonin receptors have been identified in the lens, aqueous humour and iris of the human eye[Citation8,Citation9]. In animal models, serotonin has been shown to play a critical role in lens transparency, and, thus, it is postulated that increased levels of serotonin may be associated with lens opacity in human eyes, as well[Citation7]. Recently, several studies have indicated that serotonin may play a causal role in cataract development[Citation10,Citation11]. Cataracts are a disease of the eye characterized by partial or complete crystalline opacity of the lens, impairing vision. They are the primary cause of blindness worldwide, making them a public health burden. In 2010, WHO declared cataracts to be the cause of vision loss in 51% of cases globally[Citation12].
Since cataracts are the most common cause of blindness, and since SSRIs are often first-line treatment for MDD, examining the effects SSRIs have on the eye is becoming more important for adequate monitoring and providing follow-up advice to patients.
Therefore, the goal of this study was to investigate the effects of SSRIs on corneal density (CD) and lens density (LD) in patients with depression over a three-month follow-up period. In addition, intraocular pressure (IOP) and anterior chamber parameters, including anterior chamber volume (ACV), anterior chamber depth (ACD), central corneal thickness (CCT) and corneal volume (CV) were evaluated via three drugs in the SSRI group (Sertraline, Escitalopram and Fluoxetine) over the same three-month span. This study may provide a clearer understanding of drugs’ risk stratification, on an individual level, for the risk of cataract development.
Methods
Study design and participants
This prospective, randomized study was conducted in a tertiary hospital between February 2018 and June 2018. The study was approved by the Institutional Ethics Committee (Prot. no: 260) and was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all subjects prior to enrolment in the study. The patients, who were diagnosed with MDD according to The Diagnostic and Statistical Manual of Mental Disorders, fourth edition, revised (DSM) criteria (American Psychiatric Association)[Citation13] and who were scheduled to begin taking SSRIs through an experienced psychiatrist (F.Ö.O.), were referred to the Department of Ophthalmology. The patients made up a relatively homogeneous group, and the study had a comparatively small sample size (31); so, analyses of MDD subtypes were not conducted. The patients were evaluated independently of the ophthalmologist. The treatments were selected naturalistically, and each patient's clinical condition influenced treatment choice. The treatments began by titrating a half dose of the SSRIs for the first four days and then titrating the full, initial dose. Titration was performed to reduce drug-related side effects.
Initially, 67 patients were diagnosed with MDD and began SSRI treatment, including Sertraline, Paroxetine, Citalopram, Escitalopram and Fluoxetine. After all exclusion criteria were applied, the study sample included 31 patients prescribed Sertraline, 50 mg/daily, Escitalopram, 10 mg/daily, or Fluoxetine, 20 mg/daily for MDD. Patients were included if they had scheduled follow-ups at the three-month mark and took their prescribed medicine regularly.
Patients were excluded from the study if they were less than 18 or more than 50 years old, had any psychiatric disease(s) other than MDD, received any topical or systemic medication except SSRIs, were active or former smokers, had hypertension or diabetes mellitus, were pregnant or lactating, had previous ocular trauma or surgery, had active or former ocular inflammation, had glaucoma, had corneal or retinal disease, had narrow iridocorneal angles, or had refractive errors greater than ± 3 dioptres (D). The presence of exclusion criteria was determined by examining or questioning the patients ().
All patients underwent a complete ophthalmologic examination, which included refraction, best corrected visual acuity, slit lamp examination, IOP measurement with a Goldmann applanation tonometer, fundoscopy and gonioscopy. In the gonioscopy measurements, the iridocorneal angle was wide (35°–45°) or moderately open (20°–35°) open for all cases. Both eyes of each participant were measured, the parameters recorded were IOP, ACD, CV, ACV, CD, LD and CCT. These were recorded at the start of treatment, as well as during the one-week, one-month and three-month follow-ups. To avoid diurnal variations, all examinations and measurements were performed at the same time of day.
Cornea and lens densitometry measurement techniques
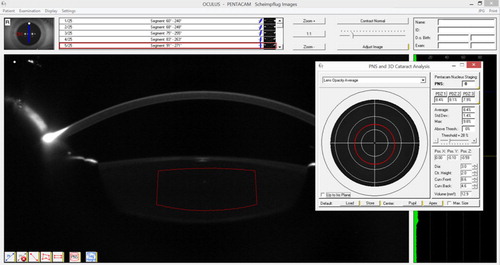
The Pentacam HR (Oculus Inc, Wetzlar, Germany) was performed before SSRI treatment and after SSRI treatment at one-week, one-month and three-month follow-ups. In all visits, anterior segment parameters were assessed using Pentacam HR, without applying any drops before fundoscopy, to evaluate ACD, CV, ACV, CD and CCT. After pupil dilatation with 0.5% tropicamide, the Pentacam HR process was repeated to perform LD (3D) measurements, and a 1 mm (vertical) × 2 mm (horizontal) rectangle was drawn (). The values of the 1 mm (vertical) and 2 mm (horizontal) lines were selected to maintain standardization, although some adjustments were made due to individual nucleus dimension variabilities. CD measurements were manually performed on the apex of the cornea manually (). All Pentacam HR measurements were performed by the same clinician (A.B).
Statistical analysis
To analyse outcomes, SPSS 22.0 software for Windows (SPSS Inc., Chicago, IL) was used for statistical analysis. A Kolmogrov-Smirnov test was also used to determine whether the variables were normally distributed. Repeated measures ANOVA analyzed the differences between the results for the seven parameters from each of the four measurement sessions (before SSRI treatment and at one-week, one-month and three-month follow-ups). When determining if there were differences between the means, if the assumption of sphericity was provided, the Sphericity Assumed test was used, but, if the assumption of sphericity was not provided, the Greenhouse-Geisser test was used. A two-tailed case was considered in all instances, and a P value of <0.05 was regarded as significant.
Results
During the study period from February 2018 to June 2018, a total of 62 eyes, from 31 patients, were examined at initiation of SSRI treatment and then at one-week, one-month and three-month follow-ups. The sample consisted of four (12.9%) males and 27 (87.1%) females, with a mean age of 24.3 ± 7.4 years. Sertraline, 50 mg/daily, was given to ten patients; 11 received Escitalopram, 10 mg/daily; and ten were treated with Fluoxetine, 20 mg/daily. There was no difference between the three groups in terms of mean age (P = 0.309), while the Sertraline group was different, in terms of gender, from the other two groups (P < 0.00).
Overall analysis of SSRI groups
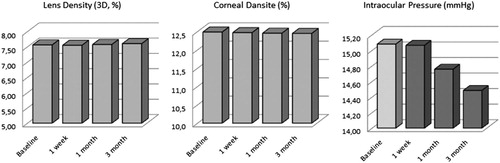
Overall, there was no risk of cataract development at three months after beginning SSRI treatment. CD and LD also did not alter over the three-month period. A significant decrease in ACD was recorded at the one-week follow up; however, after three months, this decrease was insignificant compared to the baseline. ACV, CV, CCT, CD and LD showed no significant alterations in any of the three-month follow-up examinations. IOP, however, significantly fell, with a median value of 15.0 at baseline to 14 at the one-month and three-month points (P = 0.004). This may indicate a decreased risk of developing glaucoma in patients taking SSRIs. These parameters clearly show that SSRIs, in the short-term, have no causal association with glaucoma and cataract development ().
Individual drug analysis
Sertraline
No significant change was observed at the three-month follow-up, but IOP was significantly lower, compared to the baseline ().
Table 1. Results of repeated measures ANOVA for Sertraline, 50 mg/daily, on ocular parameters.
Escitalopram
Except for IOP, which was significantly lower, no ocular parameters showed any significant change at the three-month follow-up ().
Table 2. Results of repeated measures ANOVA for Escitalopram, 10 mg/daily, on ocular parameters.
Fluoxetine
ACD showed significant increase at the three-month follow-up. However, IOP showed no significant change ().
Table 3. Results of repeated measures ANOVA for Fluoxetine, 20 mg/daily, on ocular parameters.
Discussion
The purpose of the current study was to investigate the association between changes in anterior chamber parameters (such as ACV, ACD, CCT, IOP, CD and LD) and three SSRI drugs (Sertraline, Escitalopram and Fluoxetine) at the three-month follow-up after beginning SSRI treatment. To achieve the most reliable results, patients were excluded if they had any systemic or ocular diseases or if they were taking medications except SSRIs, which may affect the anterior or posterior segments of the eye.
Previous literature has reported ocular side effects of SSRIs, such as cataracts[Citation10,Citation11], central retinal vein occlusion[Citation15], acute angle-closure glaucoma[Citation16], optic neuropathy[Citation17] and diplopia[Citation18]. In the present study, the patients, who began SSRI treatment, were examined for possible ocular effects at one week, one month and three months after starting treatment, and no patients presented these side effects.
In individuals with glaucoma and suspected glaucoma, elevated IOP may irreversibly damage the optic nerve and can cause permanent blindness. Therefore, it is imperative to know the risk factors in these patients. Some studies have been conducted to find associations between SSRIs and the risk of acute angle-closure glaucoma (AACG)[Citation19–21]. The potential mechanism underlying this association is unclear but may be related to effects on serotonin receptors in the iris and ciliary body of the eye. The effect of serotonin on 5-HT7 receptors, which have been identified at the pupil sphincter, leads to relaxation of the sphincter muscle and can cause mydriasis[Citation8,Citation22,Citation23]. Mydriasis could trigger a glaucomatous attack when it occurs in eyes that already have narrow iridocorneal angles. However, in the present study, all patients were examined by gonioscopy, and they had wide (35°−45°) or moderately open (20°−35°) angles. All narrowed angles were excluded, so no glaucomatous attacks were observed. The patients, who began SSRI treatment, were observed to have decreased IOP at one-week, one-month and three-month follow-ups. This was especially noted with three-month use of both Sertraline and Escitalopram. These results show that Sertraline, Escitalopram and Fluoxetine can be used, for at least a three-month period, in individuals with open angle glaucoma. IOP becoming relatively lower may indicate a better prognosis for reducing the risk of open angle glaucoma in SSRI users.
To understand the mechanism for the risk of cataract development with SSRIs, the pharmacodynamics of SSRIs must first be examined. Animal models have clearly proven that there is a large number of serotonin receptors in the eye lens, which play a significant role in maintaining lens transparency[Citation7]. Increased serotonin levels in the lens milieu have been shown to induce lens opacity in these animal models, which predicts cataract development. Serotonin is also a component of the aqueous humour, which regulates IOP. Changes in serotonin levels are associated with increased IOP, which increases the risk of cataracts[Citation9].
The current research was a prospective study to determine the effects of SSRIs on cataract development risk factors in the early months of SSRI prescription. Several factors, like ageing, use of corticosteroids, hypertension, smoking, diabetes and exposure to excessive UV light, have also been associated with cataract development[Citation24,Citation25]. Thus, to achieve the most reliable results, patients presenting risk factors that could lead to cataract formation were excluded. This research is unique because it is a pioneer study assessing this modifiable risk factor for a debilitating disease of the eye: cataracts. Although this study did not find any association between SSRIs and cataract risk during three months of SSRI treatment, several significant pieces of data were observed. The current study also demonstrated that parameters like CV, CD, LD, ACD and ACV need not be monitored in early SSRI treatment for ruling out cataract development in patients taking antidepressants. Therefore, ocular monitoring may be advised later for patients taking SSRIs.
Recent research from the Rochester Epidemiology Project – a population based, case control study conducted in 2011 in Olmsted County, Minnesota, U.S. – shows that the risk of cataract surgery increases in patient staking SSRIs after one year of drug intake[Citation14]. Two other population based studies from the U.S. and Canada confirm the increased risk of cataract development in SSRI users[Citation26]. A 2018 meta-analysis from China also indicates increased risk of cataracts with SSRI use. In this study, a significant, direct association with cataract indigence was seen with Fluoxetine and Fluvoxamine administration. Other SSRIs were not associated with the risk of cataract development[Citation7]. It illustrates that, although the mechanisms of all SSRIs are similar, some of them may predominantly affect the eye lens. This suggests that some drugs may have different side effects, even if they begin to the same group. Thus, related drugs must be examined separately. The present study was able to assess patients with uninterrupted follow-ups using three different SSRIs (Sertraline, Escitalopram and Fluoxetine).
Similar to the current research, Becker et al. (2017), working in the U.K., fails to show any positive association between SSRIs and cataract development using the U.K. based Clinical Practice Research Data link. Their study, using data from 1995 to 2005, includes 206,931 cases and age controls (>40)[Citation11]. They conclude that long-term prescriptions of SSRIs (>20 years) were not associated with increased cataract development risk. However, in the 40–64 age group, a slightly increased risk of cataract development was seen compared to non-users of SSRIs. In the current study, patient age, with a mean of 24.3 ± 7.4 years, was between 18 and 50, and there was no statistically significant difference in LD (3D) value among the patients in this age range.
Anterior chamber parameters and CD are important for affecting keratometric values and changing patients’ refractive status. If refractive surgery is planned, it should be ensured that a patient's refractive status remains stable. A previous study reported that serotonin induces cell inflammation and apoptosis in corneal epithelial cells[Citation27]. Since this effect may lead to changes in CD, the present research performed CD measurements by Pentacam HR, finding that SSRIs made no significant changes in anterior chamber parameters, LD or CD at the three-month follow-ups. This indicates that SSRI users can undergo refractive surgery during the first three months of drug administration.
The strength of this study lies in the variety of investigations done for the ocular examination and analysis of each patient's parameters during three months of regular follow-ups. The Pentacam HR test for anterior chamber analysis is a standardized test and was prospectively applied here. The limitations of the study were its short follow-up period, small sample size and sample size allocation, which may not be a predictor of the country's entire population. Additionally, MDD subtypes were not analyzed, and structure tests, such as SCID-I, were not performed to determine depression severity and calculate dose equivalents for SSRIs. The authors intend to extend the study with a more robust sample size and a longer duration to better assess the relationship between SSRIs and cataracts. Other confounding factors like diabetes, smoking and age (including cases over 50) can be considered in future studies.
Conclusion
In summary, this study did not find any causal association between SSRIs (Sertraline, Escitalopram and Fluoxetine), cataract, glaucoma or changes in CD and LD over a three-month period. Patients prescribed these medications for short durations seem not to be at any risk of developing cataracts or glaucomatous attacks in this small sample study. However, considering the reports in the literature, regular eye examinations should be recommended to patients using SSRIs until the ocular effects of each SSRI drug is clearly known.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from each participant included in the study.
Disclosure Statement
No potential conflict of interest was reported by the authors.
References
- WHO. Fact Sheet. 22nd March 2018.
- Cetin M, Acikel C. In perspective of meta-analyses: are all of the antidepressants similar? Bul Clin Psychopharmacol. 2009;19(2):87–92.
- Akkaya C, Kırlı S, Eker S, et al. Comparison of the efficacy and safety of sertraline, reboxetine, and venlafaxine in patients with major depressive disorder: a pooled analysis of four randomized, open-label trials. Bul Clin Psychopharmacol. 2010;20:274–287. doi: 10.1080/10177833.2010.11790673
- NICE Clinical Guidelines. CG90. Depression in adults: the treatment and management of depression in adults. Appendix 19: clinical evidence forest plots. National Collaborating Centre for Mental Health (UK). Leicester (UK): British Psychological Society; 2010.
- Brody DJ, Pratt LA, Hughes JP. NCHS Data Brief, February 2018.
- Balikci A, Uzun O, Erdem M, et al. Side effects that cause noncompliance to antidepressant medications in the course of outpatient treatment. Bul Clin Psychopharmacol. 2014;24(1):69–75. doi: 10.5455/bcp.20120827114140
- Fu Y, Dai Q, Zhu L, et al. Antidepressants use and risk of cataract development: a systematic review and meta-analysis. BMC Ophthalmol. 2018;18(1):31. doi:10.1186/s12886-018-0699-0.
- Costagliola C, Parmeggiani F, Semeraro F, et al. Selective serotonin reuptake inhibitors: a review of its effects on intraocular pressure. Curr Neuropharmacol. 2008;6:293–310. doi: 10.2174/157015908787386104
- Veglio F, De Sanctis U, Schiavone D, et al. Evaluation of serotonin levels in human aqueous humor. Ophthalmologica. 1998;212:160–163. doi: 10.1159/000027268
- Kisilevsky E, Margolin EA. Case of rapid bilateral cataract development in teenager using selective serotonin reuptake inhibitors. Can J Ophthalmol. 2014;49:e114–e115. doi: 10.1016/j.jcjo.2014.06.005
- Becker C, Jick SS, Meier CR. Selective serotonin reuptake inhibitors and cataract risk. Ophthalmology. 2017;124(11):1635–1639. doi:10.1016/j.ophtha.2017.05.002.
- WHO. Blindness and vision impairment prevention report. 2018.
- Diagnostic and statistical manual of mental disorders, text revision (DSM-IV-TR). 4th ed Washington (DC): American Psychiatric Association; 2000.
- Erie JC, Brue SM, Chamberlain AM, et al. Selective serotonin reuptake inhibitor use and increased risk of cataract surgery: a population-based, case-control study. Am J Ophthalmol. 2014;158(1):192–197.e1. doi:10.1016/j.ajo.2014.03.006.
- Retianl Hardisty AD, Hemmerdinger CM, Quah SA. Citalopram-associated central retinal vein occlusion. Int Ophthalmol. 2009 Aug;29(4):303–304. doi:10.1007/s10792-008-9231-5.
- Chen HY, Lin CL, Lai SW, et al. Association of selective serotonin reuptake inhibitor use and acute angle-closure glaucoma. J Clin Psychiatry. 2016 Jun;77(6):e692–e696. doi:10.4088/JCP.15m10038.
- Lochhead J. SSRI-associated optic neuropathy. Eye. 2015 Sep;29(9):1233–1235. doi:10.1038/eye.2015.119.
- Eray S, Ucar HN, Vural AP. Sertraline-induced diplopia. Bul Clin Psychopharmacol. 2016;26(2):213–214. doi:10.5455/bcp.20160109124021.
- Seitz DP, Campbell RJ, Bell CM, et al. Short-term exposure to antidepressant drugs and risk of acute angle-closure glaucoma in older adults. J Clin Psychopharmacol. 2012;32:403–407. doi: 10.1097/JCP.0b013e31825420a1
- Health Canada. Summary safety review—antidepressants—assessing the potential risk of serious eye disorder (angle-closure glaucoma). [cited 2016 Aug 12]. Available from: http://www.hc-sc.gc.ca/dhp-mps/medeff/reviews-examens/antidepress-eng.php.
- Kirkham J, Seitz D. Evidence of ocular side effects of SSRIs and new warnings. Evidence Based Mental Health. 2017;20(1):27. doi:10.1136/eb-2016-102528. Epub 2016 Dec 19.
- Costagliola C, Parmeggiani F, Sebastiani A. SSRIs and intraocular pressure modifications. CNS Drugs. 2004;18:475–484. doi: 10.2165/00023210-200418080-00001
- Gündüz GU, Yener NP, Kılınçel O, et al. Effects of selective serotonin reuptake inhibitors on intraocular pressure and anterior segment parameters in open angle eyes. Cutan Ocul Toxicol. 2018;37(1):36–40. doi:10.1080/15569527.2017.1330270.
- Das GK, Boriwal K, Chhabra P, et al. Presenile cataract and its risk factors: a case control study. J Family Med Prim Care. 2019;8(6):2120–2123. doi:10.4103/jfmpc.jfmpc_267_19.
- Lindblad BE, Håkansson N, Wolk A. Smoking cessation and the risk of cataract: a prospective cohort study of cataract extraction among men. JAMA Ophthalmol. 2014;132(3):253–257. doi:10.1001/jamaophthalmol.2013.6669.
- Aboujaoude E, Koran LM. The American psychiatric publishing textbook of psychopharmacology. 4th ed Washington (DC): American Psychiatric Publishing; 2009.
- Zhang X, Yin Y, Yue L, et al. Selective serotonin reuptake inhibitors aggravate depression-associated dry eye via activating the NF-jB pathway. Invest Ophthalmol Vis Sci. 2019;60:407–419. doi:10.1167/iovs.18-25572.