Abstract
Introduction
Epilepsy is a chronic non-communicable disease of the brain that affects millions of people worldwide. A significant number of children are affected globally, and most live in developing countries, often with physical and cognitive disabilities. Regardless of these factors, epilepsy is poorly controlled, particularly in the developing countries. Thus, this study aimed to assess the magnitude of treatment outcomes and its predictors among pediatrics patients with epilepsy who were followed-up at the Dessie Comprehensive Specialized Hospital, Northeast Ethiopia.
Methods
Hospital-based cross-sectional study was conducted from 1 June 2022 to 30 August 2022. A total of 200 patients with epilepsy were included in this study. Data were collected through face-to-face interviews, and by reviewing medical records. The collected data were entered into Epi-data version 4.6 and exported to SPSS version 25.0. Descriptive statistics such as frequencies, percentages, means and standard deviations were computed. Binary and multivariate logistic regression analyses were performed. Variables with p < 0.25 in bivariate analysis were entered into multivariable logistic regression. In multivariable analysis, adjusted odd ratio with 95% CI and p-value less than 0.05 were considered statistically significant.
Results
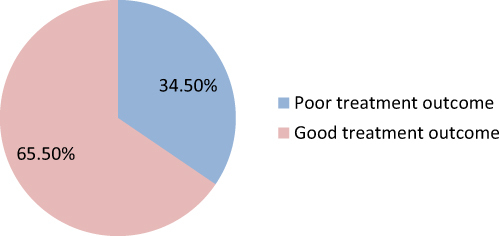
Of 200 pediatric patients with epilepsy, 66 (34.5%) had poor treatment outcomes. In the multivariate analysis, 11–15 years of age (AOR = 4.08; 95% CI = 1.202, 13.848), poor treatment adherence (AOR = 3.21; 95% CI = 1.421, 7.249), history of more seizure frequency before starting treatment (AOR = 4.19; 95% CI = 1.984, 8.834) and history of head injury (AOR = 3.03; 95% CI = 1.502, 6.112) were significantly associated with poor treatment outcomes in pediatric patients with epilepsy.
Conclusion
Significant proportion of pediatric patients with epilepsy had poor treatment outcomes. Therefore, health-care workers should strictly follow patient treatment especially for pediatric epileptic patients’ who have poor treatment adherence, more seizure frequency history, head injury history and whose age were 11–15 years old.
Introduction
Epilepsy is a severe neurological disorder affecting more than 70 million people worldwide, ranging from neonates to late adulthoods.Citation1 It is a chronic disorder of the brain characterized by the long-term occurrence of epileptic seizures which happened because of too much discharge of neuron in the central nervous system.Citation2,Citation3 Physical injuries like head, soft tissue, dental and burn are common among epilepsy patients and the occurrence of physical damage has a negative impact and a higher mortality rate on the affected individuals.Citation4,Citation5
The goal of epilepsy management is to prevent seizures without side effect of drugs by incorporating optimum patient education regarding adherence of medications while maintaining the best quality of life.Citation5–7 Evidence revealed that more than half people with epilepsy could become seizure free with the proper use of anti-seizure drugs.Citation8–11 However, children and young people have many unresolved concerns about their medications and some do not fully appreciate the consequences of not taking antiepileptic medicines.Citation12 Other patients had developed one or more antiepileptic drugs related adverse effects.Citation5,Citation8,Citation13,Citation14
A study indicated that juvenile myoclonic epilepsy is associated with seizures that do not occur at a specific point during the awake sleep cycle and have a reduced response to antiepileptic drugs.Citation15 Another study revealed that the predictors of poor outcomes include partial seizure presentation, mesial temporal sclerosis or bitemporal epilepsy, and the use of several antiepileptic drugs.Citation16 Different studies showed that medication adherence was significantly associated with treatment outcome.Citation5,Citation7,Citation13,Citation17 A study at the University of Gondar Teaching Hospital also showed that female sex was significantly associated with treatment outcomes.Citation17
In contrast, the overall prevalence of non-adherence to antiepileptic medications among patients with epilepsy attending the referral hospital was 38.5%. Divorced and widowed marital status, long treatment duration, presence of comorbidity, side effects of antiepileptic medications, epilepsy-related stigma, absence of health information, and negative attitude towards antiepileptic medications were significantly associated with non-adherence to antiepileptic medications. This results in poor treatment outcomes in patients undergoing follow up treatment.Citation18
Studies documented that low IQ predicts lower chances of seizure freedom after resective epilepsy surgery. However, a large proportion of patients had a reduction in seizure frequency at long-term follow-up, indicating resective surgery as an important palliative potential for intellectual disability patients with epilepsy.Citation19,Citation20
In general, uncontrolled epilepsy treatment outcome might result in a decrease quality of life, stigma in the community, physical injuries and increased mortality.Citation5,Citation21,Citation22 Some antiepileptic medications such as valproate also reduce cognitive abilities and performance levels in children. Reduced right-handedness and verbal vs non-verbal abilities might be attributable to changes in cerebral lateralization induced by exposure to antiepileptic drugs.Citation23–25 In Ethiopia, the lack of acceptance of modern antiepileptic drugs and negative medication beliefs highly influenced patients and the community, as they perceived epilepsy to be treated by traditional healers and spiritual holy water, which may push them to not take the medicine.Citation3,Citation21,Citation26–28
Although various studies have been conducted in different parts of the world, studies regarding treatment outcomes among pediatric patients with epilepsy in Ethiopia are scarce, especially in the study region. Therefore, the aim of this study was to assess treatment outcomes and related factors among pediatric patients with epilepsy who were followed-up at Dessie Comprehensive Specialized Hospital, Northeast Ethiopia, as this hospital serves millions of people who come from South Wollo, North Wollo, Oromia special zones and some parts of the Afar region.
Methods
Study Area and Period
This study was conducted at Dessie Comprehensive Specialized Hospital, which is located in Dessie Town Administration, Northeast Ethiopia. Dessie Town is located in the Amhara region, 480 km from the capital of the region, Bahir Dar and approximately 401 km from Addis Ababa. Dessie Town is the capital city of the South Wollo Zone administration. Dessie Comprehensive Specialized Hospital provides service for more than 8 million people. In DCSH, different follow-up clinics provide service to clients. Pediatric follow-up clinic provide service for more than one million children from the South Wollo zone, Oromia special zone, and some parts of the Afar region. The study was conducted from 1 June 2022 to 30 August 2022 (three months’ duration).
Study Design
Hospital based cross-sectional study was conducted by using document review and face-to-face interviews in the outpatient department of DCSH pediatric epilepsy follow-up clinic.
Source Population and Study Population
All pediatric patients with epilepsy who were followed up at DCSH pediatric OPD were the source population, whereas all pediatric epileptic patients who visited pediatric OPD of DCSH during the study period were the study population.
Inclusion and Exclusion Criteria
All clinically diagnosed patients with epilepsy age less than 18 years who attended the pediatric follow-up clinic during the study period were eligible for the study. However, patients with epilepsy who were lost to follow-up before three months or new patients who had less than three months of treatment follow-up were excluded from the study.
Sample Size Determination and Sampling Technique
Since the total numbers of pediatric patients with epilepsy who met the inclusion criteria in DCSH follow-up clinic per three months were small (200) which means that every patient had an appointment every three months for clinical evaluation and medication refill. Therefore, we took all 200 pediatric epileptic patients who had follow-up during the data collection period without sample size calculation. All eligible participants were interviewed, and their medical records were reviewed during the appointment follow-up period. Therefore, further sampling techniques were not required.
Data Collection Tool and Procedure
The data were collected using structured questionnaires. The questionnaire was adopted from different studies, with modifications for face-to-face interviews and overlooking of medical records. The questionnaire contained socio-demographic variables, clinical variables, and variables related to treatment modality and treatment outcome. The data extraction format was used to retrieve the children’s clinical information and medication experience, such as the status of treatment outcome, types of epilepsy, seizure frequency, duration of follow-up, types of AEDs, and AED-related adverse effects from patients’ medical records (Supplementary Material 1).
Two data collectors (nurses) were recruited for data collection. After informing the parents about the purpose of the study and the importance of their participation, socio-demographic data were collected through interviews by data collectors. Data regarding clinical-related variables, treatment modalities and treatment outcomes were also collected by reviewing the medical records.
Data Quality Control
To ensure data quality, the questionnaire was initially prepared in English, translated to Amharic (the local language), then then returned to Amharic for consistency. Prior to the start of data collection, training was provided to the data collectors by investigators regarding the objective of the study, data collection procedures, confidentiality of the information, and each component of the questionnaire. Principal investigator frequently checked the data collection procedures for consistency. Additionally, the principal investigator checked the collected data daily to ensure completeness and clarity.
Prior to the actual data collection, the questionnaire was pretested on 10% of the total sample size at Borumeda Hospital, which is not part of the actual data collection area but has no geographical or cultural variations. Based on the pre-test, some modifications were made to the questionnaire. The final modified Amharic questionnaire was used to collect the data. To test the reliability of the Amharic version tool, Cronbach alpha was calculated and was found to be 0.72.
Operational Definitions
Good treatment outcome: Patients who had a maximum of three seizure episodes in the three months after the start of antiepileptic treatment.
Poor treatment outcome: Patients who had four or more seizure episodes within three months after the start of antiepileptic treatment.Citation17
Excellent Adherence: If patients took more than 90% of their monthly medication.
Good Adherence: If patients took 85–90% of their monthly medication.
Poor Adherence: If patients took less than 85% of their monthly medication.Citation17
Emotional stress: The feeling of emotional tension and uneasiness produced by situations of danger, threat, loss of personal security, internal conflicts, frustrations and sadness.
Sleep deprivation: Refers to no sleep or a reduction in the usual sleep time, exists when an individual routinely sleeps less than the amount required for optimal functioning.
Data Processing and Analysis
The investigators visually checked the collected data. Data were coded, entered into Epi Data version 4.6, and exported to the SPSS version 25 software for analysis. Descriptive summaries such as frequencies and percentages were presented in the form of graphs and tables. Bivariable analysis was performed for the Crude Odds Ratio (COR), and multivariate analysis was used to calculate the Adjusted Odds Ratio (AOR). All variables were entered into the multivariable model by considering a p-value of <0.25 in bivariable analysis. Statistical significance was set at P < 0.05 in multivariable analysis, at 95% confidence intervals.
Results
Socio-Demographic Characteristics
In the current study, the respondents had a 100% response rate. The median age of participants was 8.0 (SD ± 3.52). A total of 105 participants (52.5%) were females. Approximately half (49.5%) of the care givers were farmers in their occupation. Approximately two-thirds (63%) of respondents lived in rural areas ().
Table 1 Socio-Demographic Characteristics of Pediatric Patients with Epilepsy in DCSH, Northeast Ethiopia, 2022 (n = 200)
Clinical Conditions of Pediatric Patients
In this study, 48.4% of the participants showed excellent adherence to epileptic medication. Among the 200 study participants, 25.5% had a history of discontinuing medication. Among the study participantsCitation7 who had neurological problems, 13 (43.3%) had motor weakness, 11 (36.7%) had learning difficulties and 6 (20%) had hearing problems. Among the epileptic pediatric patients who had a history of triggering factors (n = 66) during the onset of epilepsy; 19 (28.8%) experienced emotional stress, 38 (57.6%) experienced sleep deprivation, and 9 (13.6%) had missing medication. Of all participants, 74 (37%) were developed status epilepticus ().
Table 2 Clinical Conditions of Pediatric Patients with Epilepsy in DCSH, Northeast Ethiopia, 2022
Medical Conditions of Epileptic Pediatric Patients
Of 200 pediatric patients with epilepsy, 122 (61%) had a history of mono-therapy modes of treatment at the start of medication in health facilities. Among the 80 patients, the reasons for shifting from the first to the second treatment category were drug side effects 21 (26.25%), absence of drugs 23 (28.75%), high cost of drugs 5 (6.25%), and poor control by first drugs 31 (38.75%). Among all the participants, 29 (14.5%) had a history of delayed mile stones ().
Table 3 Medical Conditions of Pediatric Patients with Epilepsy in DCSH, Northeast Ethiopia, 2022
Treatment Outcome Among Epileptic Patients
Among the 200 pediatric patients with epilepsy, 66 (34.5%) had poor treatment outcomes ().
Factors Associated with Treatment Outcomes of Epileptic Pediatric Patients
In multivariable regression analysis, the age of pediatric patients, treatment adherence, frequency of seizures before starting treatment, and history of head injury were determinant factors for treatment outcome. Patients age group of 11–15 years were 4.08 times more likely to have poor treatment outcomes than those aged groups of patients <5 years (AOR = 4.08; 95% CI = 1.202, 13.848). Patients with poor adherence to their medication were 3.21 times more likely to have poor treatment outcomes than those with excellent adherence (AOR = 3.21; 95% CI = 1.421, 7.249). Epileptic pediatric patients who had a history of seizure frequency greater than five per month were 4.19 times more likely to have poor treatment outcomes than those with a seizure frequency of less than or equal to five (AOR = 4.19; 95% CI = 1.984, 8.834). Patients having history of head injury were 3.03 times more likely had poor treatment outcome than those not having history of head injury (AOR = 3.03; 95% CI = 1.502, 6.112) ().
Table 4 Factors Associated with Treatment Outcomes Among Epileptic Pediatric Patients in DCSH Northeast Ethiopia, 2022
Discussion
Epilepsy is a crucial global public health problem, especially in Ethiopia. Scientific investigations of the outcomes of epileptic treatment and associated factors among children are necessary to design appropriate interventions. Thus, this study aimed to assess the magnitude of treatment outcomes and associated factors in pediatrics patients with epilepsy in Northeast Ethiopia. This finding revealed that 34.5% of the patients had poor treatment outcomes. The reason for the poor treatment outcome in the current study may be due to the study setting, which was conducted in a comprehensive specialized hospital in which most patients with epilepsy who were noncompliant to antiepilepsy drugs and had complications were referred to this hospital. In addition, poor medication adherence in the current study (27.5%) may have contributed to the poor treatment outcomes. This finding was in line with a study conducted on newly diagnosed epilepsy patients, where 30–40% of participants had uncontrolled seizure activities with antiepileptic drugs.Citation10 However, the current findings were lower than those of studies conducted in follow-up clinics of epileptic patients in resource poor settings (43.3%),Citation8 Mettu Karl Comprehensive Specialized Hospital (43.96%),Citation29 Ambo Hospital (44.7%),Citation7 tertiary care hospital (65.6%),Citation5 Mizan-Tepi University Teaching Hospital (60.8%)Citation13 and Ayder Comprehensive Specialized Hospital (53.4%).Citation3 However, the current finding was higher than that of a study conducted at the University of Gondar referral and teaching hospital, where 17.56% of patients did not have well-controlled seizure status in the last three month follow-up period.Citation14 The possible reason for the different findings across various studies may be the difference in the study design used, differences in study participants (children and adults), methods used to measure the treatment outcome of antiepileptic drugs, differences in socio-demographic characteristics of participants, presence of variation in data collection periods, and study area difference. Additionally, it may be due to differences in the availability of resources, such as the level of patient care and epilepsy management protocols.
In the multivariate analysis model, the age of pediatric patients, adherence to treatment, frequency of seizures, and history of head injury were factors associated with the outcome variable. Patients whose age group is 11–15 years are more likely to have poor treatment outcomes than younger patients. This might be due to the decrease in maternal and paternal care for children in these age groups when we compared those of the younger ones so that they might not take their medications properly. Patients with poor medication adherence on their medication were more likely to have poor treatment outcomes than those with excellent medication adherence. This was congruent with a study conducted at the University of Gondar Teaching Hospital, where excellent adherence to antiepilepsy treatment was significantly associated with successful treatment outcome.Citation17 Low medication adherence was also a predictor of uncontrolled seizures during follow-up at the neurological clinic of the Ayder Comprehensive Specialized Hospital.Citation3 A possible explanation for this finding might be that epileptic patients who had drug therapy problems were more likely to develop poor treatment outcomes than those who had no drug therapy problems, indicating that any problem with therapy resulted in poor treatment outcomes.Citation29 In Ethiopia, there is a high burden of antiepileptic drug non-adherence among individuals with epilepsy, which requires clinicians to give more concern for monitor and evaluate antiepileptic medication adherence in the health-care service to obtain good treatment outcomes.Citation30
Epileptic pediatric patients who had history of seizure frequency greater than five per month were more likely had poor treatment outcome than those having less than or equal to five seizure frequency history. This was in line with research conducted at Mizan-Tepi University Teaching Hospital, in which a high frequency of seizure attacks before antiepileptic drug initiation was a predictor of uncontrolled seizures.Citation13 Patients with history of head injury were more likely to have poor treatment outcomes than those without history of head injury. This was similar to a study conducted at Mettu Karl Comprehensive Specialized Hospital and Mizan-Tepi University Teaching Hospital.Citation13,Citation29
This study had several limitations. First, because we used a cross-sectional study design, the direction of the relationship between the variables could not always be determined. Second, this study was carried out at the Dessie Comprehensive Specialized Hospital; therefore, our findings may not be representative at the national level. Third, this study used a quantitative method that lacked triangulation with qualitative study.
Conclusion
The magnitude of the poor treatment outcomes in pediatric patients with epilepsy was found to be high. Factors such as being 11–15 years of age, poor adherence to treatment, higher seizure frequency before starting treatment, and history of head injury were significantly associated with poor treatment outcomes in patients with epilepsy. Therefore, to improve the treatment outcomes in patients’ regional health bureaus and the Ministry of Health should pay close attention to the identified factors. Health-care providers should continuously counsel mothers and patients on proper treatment adherence and more attention to patients with a history of head injury and a high frequency of seizure attacks before antiepileptic drug initiation to improve treatment outcomes in children. This reveals the need for clinicians to pay more attention to the monitoring and evaluation of antiepileptic drug adherence in health-care services to achieve good treatment outcomes. Future research should conduct further investigations on multi-center facilities using mixed quantitative and qualitative approaches.
Abbreviations
AEDs, Antiepileptic drugs; AOR, Adjusted Odds Ratio; CI, Confidence interval; COR, crude odds ratio; DCSH, Dessie comprehensive specialized hospital; EB, Ethiopian birr; IQ, Intelligence quotient; OPD, Outpatient department; SD, Standard deviation; SPSS, Statistical Package for Social Sciences.
Ethical Consideration
Ethical clearance was obtained from Wollo University College of Medicine and Health Science Research Ethical review committee. The ethics reference number is RCSPG-129-14. Communication with hospital administrators was conducted using formal letters. Written informed consent was obtained from all parents or legal guardians of the study participants prior to study commencement after information was provided about the purpose of the study, non-invasiveness of the data collection procedure, confidentiality of the information, and the risks and benefits of the study. Data collectors were read written informed consent in local language for parents or legal guardians who were unable to read/write to get their written informed consent for their children to participate in this study. This study was conducted in accordance with the principle of the Declaration of Helsinki.
Consent for Publication
Not applicable. Individual personal details, images, or videos were not used.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas, took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest for this work.
Acknowledgments
The authors acknowledge the data collectors, supervisors, and study participants for their valuable contributions to this study.
Data Sharing Statement
The data-sets used and analyzed during this study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Thijs R, Surges R, O’brien T, Sander JW. Epilepsy in adults. Lancet. 2019;393(10172):689–701. doi:10.1016/S0140-6736(18)32596-0
- Duncan JS, Sander JW, Sisodiya SM, Walker MC. Adult epilepsy. Lancet. 2006;367(9516):1087–1100. doi:10.1016/S0140-6736(06)68477-8
- Niriayo YL, Mamo A, Kassa TD, et al. Treatment outcome and associated factors among patients with epilepsy. Sci Rep. 2018;8(1):17354. doi:10.1038/s41598-018-35906-2
- Bifftu BB, Tadesse Tiruneh B, Mekonnen Kelkay M, et al. Seizure-related injuries among people with epilepsy at the outpatient department of the University of Gondar Hospital, Northwest Ethiopia: cross-sectional institutional-based study. Neurol Res Int. 2017;2017:1–5. doi:10.1155/2017/4970691
- Nasir BB, Yifru YM, Engidawork E, Gebrewold MA, Woldu MA, Berha AB. Antiepileptic drug treatment outcomes and seizure-related injuries among adult patients with epilepsy in a tertiary care hospital in Ethiopia. Patient Relat Outcome Meas. 2020;Volume 11:119–127. doi:10.2147/PROM.S243867
- Kerr M, Scheepers M, Arvio M, et al. Consensus guidelines into the management of epilepsy in adults with an intellectual disability. J Intellectual Disability Res. 2009;53(8):687–694. doi:10.1111/j.1365-2788.2009.01182.x
- MekonenTefera G, Woldehaimanot TE, Angamo MT. Etiyopya Ambo Hastanesi’nde epilepsi hastalarında kötü tedavi sonuçları ve ilişkili faktörler [Poor treatment outcomes and associated factors among epileptic patients at Ambo Hospital, Ethiopia]. Eur J Ther. 2015;21(1):9–16. Turkish.
- Gurshaw M, Agalu A, Chanie T. Anti-epileptic drug utilization and treatment outcome among epileptic patients on follow-up in a resource poor setting. J Young Pharm. 2014;6(3):47. doi:10.5530/jyp.2014.3.8
- Meyer A-C, Dua T, Ma J, Saxena S, Birbeck G. Global disparities in the epilepsy treatment gap: a systematic review. Bull World Health Organ. 2010;88(4):260–266. doi:10.2471/BLT.09.064147
- Brodie M, Barry S, Bamagous G, Norrie J, Kwan P. Patterns of treatment response in newly diagnosed epilepsy. Neurology. 2012;78(20):1548–1554. doi:10.1212/WNL.0b013e3182563b19
- Chen Z, Brodie MJ, Liew D, Kwan P. Treatment outcomes in patients with newly diagnosed epilepsy treated with established and new antiepileptic drugs: a 30-year longitudinal cohort study. JAMA Neurol. 2018;75(3):279–286. doi:10.1001/jamaneurol.2017.3949
- Lewis SA, Noyes J, Hastings RP. Systematic review of epilepsy self‐management interventions integrated with a synthesis of children and young people’s views and experiences. J Adv Nurs. 2015;71(3):478–497. doi:10.1111/jan.12511
- Zewudie A, Mamo Y, Feyissa D, Yimam M, Mekonen G, Abdela A. Epilepsy treatment outcome and its predictors among ambulatory patients with epilepsy at Mizan-Tepi University Teaching Hospital, southwest Ethiopia. Neurol Res Int. 2020;2020:1–8. doi:10.1155/2020/8109858
- Birru EM, Shafi M, Geta M. Drug therapy of epileptic seizures among adult epileptic outpatients of University of Gondar Referral and Teaching Hospital, Gondar, North West Ethiopia. Neuropsychiatr Dis Treat. 2016;3213–3219. doi:10.2147/NDT.S119030
- Uchida CGP, de Carvalho KC, Guaranha MSB, et al. Phenotyping juvenile myoclonic epilepsy. Praxis induction as a biomarker of unfavorable prognosis. Seizure. 2015;32:62–68. doi:10.1016/j.seizure.2015.09.011
- Roy PL, Ronquillo LH, Ladino LD, Tellez-Zenteno JF. Risk factors associated with drug resistant focal epilepsy in adults: a case control study. Seizure. 2019;73:46–50. doi:10.1016/j.seizure.2019.10.020
- Beyene A, Ayalew AF, Mulat G, Simachew Kassa A, Birhan T, Russo E. The treatment outcomes of epilepsy and its root causes in children attending at the University of Gondar teaching hospital: a retrospective cohort study, 2018. PLoS One. 2020;15(3):e0230187. doi:10.1371/journal.pone.0230187
- Tilahun M, Habte N, Mekonnen K, Srahbzu M, Ayelegne D, de Carvalho M. Nonadherence to antiepileptic medications and its determinants among epileptic patients at the university of gondar referral hospital, Gondar, Ethiopia, 2019: an institutional-based cross-sectional study. Neurol Res Int. 2020;2020:1–9. doi:10.1155/2020/8886828
- Reinholdson J, Olsson I, Tranberg AE, Malmgren K. Low IQ predicts worse long-term seizure outcome after resective epilepsy surgery–A propensity score matched analysis. Epilepsy Res. 2023;191:107110. doi:10.1016/j.eplepsyres.2023.107110
- Novais F, Andrea M, Andrade G, Loureiro S, Pimentel J, Pestana LC. Intelligence quotient (IQ) as a predictor of epilepsy surgery outcome. Epilepsy Behav. 2022;132:108708. doi:10.1016/j.yebeh.2022.108708
- Muluneh AT, Haileamlak A, Tessema F, et al. Population based survey of chronic non-communicable diseases at gilgel gibe field research center, southwest Ethiopia. Ethiop j Health Sci. 2012;22(S):7–18. doi:10.1001/jama.289.18.2363
- Mehta S, Tyagi A, Tripathi R, Kumar M. Study of inter-relationship of depression, seizure frequency and quality of life of people with epilepsy in India. Mental Illness. 2014;6(1):1–4. doi:10.1108/mi.2014.5169
- Meador KJ, Baker GA, Browning N, et al. Fetal antiepileptic drug exposure and cognitive outcomes at age 6 years (NEAD study): a prospective observational study. Lancet Neurol. 2013;12(3):244–252. doi:10.1016/S1474-4422(12)70323-X
- Meador K, Baker G, Browning N, et al. Effects of fetal antiepileptic drug exposure: outcomes at age 4.5 years. Neurology. 2012;78(16):1207–1214. doi:10.1212/WNL.0b013e318250d824
- Cohen MJ, Meador KJ, May R, et al. Fetal antiepileptic drug exposure and learning and memory functioning at 6 years of age: the NEAD prospective observational study. Epilepsy Behav. 2019;92:154–164. doi:10.1016/j.yebeh.2018.12.031
- Gugssa SA, Haidar J. Knowledge, attitude, and practice towards epilepsy among religious cleric and traditional healers of Addis Ababa, Ethiopia. Seizure. 2020;78:57–62. doi:10.1016/j.seizure.2020.03.006
- Baheretibeb Y, Wondimagegn D, Law S. Holy water and biomedicine: a descriptive study of active collaboration between religious traditional healers and biomedical psychiatry in Ethiopia. BJPsych Open. 2021;7(3):e92. doi:10.1192/bjo.2021.56
- Deresse B, Shaweno D. General public knowledge, attitudes, and practices towards persons with epilepsy in South Ethiopia: a comparative community-based cross-sectional study. Epilepsy Behav. 2016;58:106–110. doi:10.1016/j.yebeh.2016.02.037
- Bekele F, Gezimu W. Treatment outcome and associated factors among epileptic patients at ambulatory clinic of Mettu Karl Comprehensive Specialized Hospital: a cross-sectional study. SAGE Open Med. 2022;10:20503121221125149. doi:10.1177/20503121221125149
- Belayneh Z, Mekuriaw B. A systematic review and meta-analysis of anti-epileptic medication non-adherence among people with epilepsy in Ethiopia. Arch Public Health. 2020;78(1):1–14. doi:10.1186/s13690-020-00405-2