Abstract
We present a case study of a patient diagnosed with infective endocarditis (IE) following the initial symptom of meningitis caused by Streptococcus gallate subsp. Pasteur. Identification of IE by clinicians is vital for timely treatment measures and can improve patient prognosis. Therefore, increased awareness and knowledge of IE are crucial for prompt and accurate diagnosis and treatment. Atypical clinical manifestations of IE can result in misdiagnosis, highlighting the need for improved clinical identification. In the instance of extended reoccurring fever coupled with damage to the central nervous system, as described in this article, it is crucial to obtain a comprehensive medical history, perform a thorough physical examination, monitor heart murmur changes dynamically, and expediently conduct blood culture and cardiac color Doppler ultrasound to lessen the possibility of erroneous diagnosis and treatment of IE Currently, there are no reported cases of IE associated with streptococcal meningitis in adults in China.
Keywords:
Background
IE is an inflammatory condition triggered by microorganisms, including bacteria that infect the endocardium or the nearby endo-artery with vegetation. It has an insidious onset and presents with a range of clinical features, making it easy to misdiagnose. The disease carries high morbidity and mortality rates, along with a substantial recurrence risk and poor prognosis. IE is one of the most prevalent acute and critical illnesses, resulting in a very high mortality rate unless treated promptly. The in-hospital mortality rate is approximately 15–20%.Citation1
Neurological complications are frequent in IE, occurring in 20–40% of cases. Although meningitis has been reported in approximately 7% of IE patients,Citation2,Citation3 the link between meningitis and IE has not received much attention, particularly when meningitis is the presenting symptom. In many instances, meningitis may present as an early indication of IE, with over a third of patients who experience meningitis going on to develop further neurological complications, such as ischemic stroke, intracranial hemorrhage, or brain abscess.Citation4
Streptococcus gallolyticus is part of the Streptococcus bovis group in group D streptococcus. It has been reported to cause meningitis and IE,Citation5,Citation6 although these complications are rare. The number of Streptococcus bovis infections has been increasing worldwide due to new detection methods. Here, we present a rare case of both meningitis and IE caused by Streptococcus gallolyticus. It is crucial to examine the relationship between the two ailments from both clinical and epidemiological perspectives.
Case Presented
The 53-year-old male patient was admitted to the hospital with intermittent fever for the last 24 days, along with headache and impaired consciousness for the past 20 days. The patient experienced intermittent fever without any obvious triggers 24 days ago. The maximum body temperature was 39°C, accompanied by low back pain and sweating, and the condition did not improve significantly after self-medication. After 20 days, the patient was admitted to the hospital at 9 p.m. with symptoms of confusion, irritability, slurred speech, and vomiting. On admission, the patient exhibits delirium, disorganized speech, a temperature of 38°C, a pulse of 120 beats/min, respiration of 35 beats/min, finger oxygen saturation of 95%, and a blood pressure of 150/40 mmHg. Physical examination reveals neck stiffness, an uncooperative demeanor, coarse breath sounds in both lungs and crackles in both lower lungs. The patient’s heart rate is 120 beats/min with a sinus rhythm and normal heart sounds. P2 and there are no pathological murmurs in any valve auscultation area nor any pericardial friction rub. After six hours, the patient experienced shortness of breath and a decrease in oxygen saturation, leading to intubation and the use of a ventilator to aid breathing. The patient has previously been diagnosed with hepatitis B and is not currently on any regular medication.
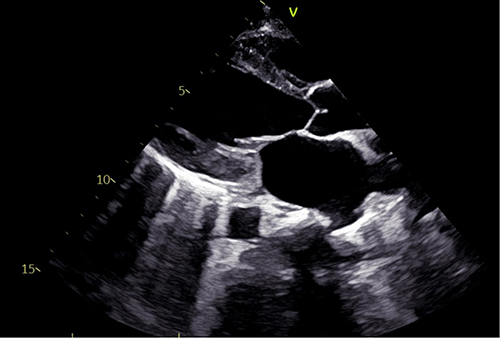
After admission, it is recommended to conduct the necessary etiological examination. The results from the blood and cerebrospinal fluid cultures have indicated the presence of Streptococcus gallate subsp. Pasteur. Additionally, the cerebrospinal fluid pressure was measured at 280mmH20, while the cerebrospinal fluid analysis has shown cerebrospinal fluid protein levels exceeding 3000 mg/L and cerebrospinal fluid glucose levels measuring at 1.60 mmol/L. Cerebrospinal Fluid Analysis: The cerebrospinal fluid appears pale yellow in color and is both transparent and turbid. There are coagulants present, and the Pantheon qualitative test results are highly positive. The white blood cell count is 5650.0 × 106/L, with 20.9% lymphocytes, 8.9% monocytes, and 70.2% neutrophils. A bedside cardiac ultrasound was conducted (refer to ), which revealed no aortic vegetation. Consequently, the diagnosis of sepsis and meningitis was considered. Based on the drug sensitivity results, the patient received anti-infective therapy consisting of ceftriaxone and vancomycin. However, the patient continues to experience intermittent fever with a peak of approximately 40°C and has a Glasgow Coma Scale (GCS) score of E1VTM1.
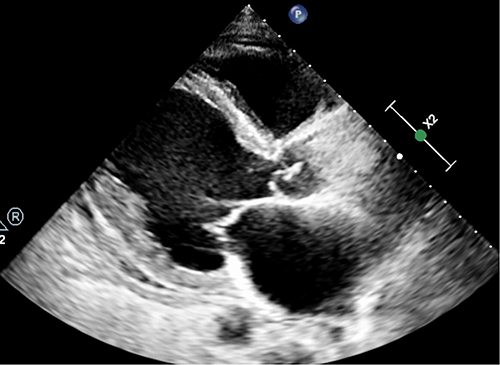
On the 15th day of admission, there was a notable increase in cardiac enzymes and other indicators compared to the time of admission. Additionally, a diastolic murmur was detected using an aortic valve stethoscope. Cardiac echocardiography was performed once again to evaluate the likelihood of vegetation present on the aortic valve (refer to ), severe backflow of blood through the aorta, minor backflow of blood through the tricuspid valve, minor cases of pulmonary hypertension, typical left ventricular systolic function, consideration of IE, and alteration of the antibiotic therapy with penicillin and gentamicin. However, the patient experienced recurrent fever and reached a peak temperature of approximately 39.5°C during treatment. Subsequently, on the 20th day of admission, the patient was transferred to the CICU for further treatment.
After being admitted to the Cardiac Intensive Care Unit, the patient’s GCS score was E1VTM1. The physical examination revealed multiple skin lesions throughout the body, scattered Roth spots in the posterior pole of the eye and around the optic disc, and crackles in both lungs. Additionally, diastolic murmurs were detected in the auscultation area of the aortic valve. Blood culture, cerebrospinal fluid culture, brain MRI, and magnetic sensitivity were pursued, but no indications of cerebral infarction, cerebral hemorrhage, or aneurysm were found. The anti-infective treatment of ceftriaxone, gentamicin, and metronidazole was adjusted, but no positive effects were observed. After reducing the analgesic and sedative drugs during treatment, the patient’s mental status improved and their GCS score was E3VTM3. However, the patient continued to experience intermittent fever during treatment. On day 28 of admission, the patient had a body temperature of approximately 39°C and a serious case of pulmonary edema was discovered via chest CT scan. After an emergency multidisciplinary consultation, surgical contraindications were ruled out, and on day 30 of admission, aortic valve replacement, intracardiac vegetation removal, and tricuspid valvuloplasty were performed. The patient regained consciousness gradually following surgery. The endotracheal intubation was removed on the 7th day post-surgery, and the patient was transferred to the general ward on the 12th day. After 56 days of admission, the patient successfully recovered and was discharged. All organ functions were restored at the time of discharge.
Discussion
A significant correlation exists between Streptococcus bovis infections and intestinal diseases. Up to 50% of patients with streptococcal bacteremia or endocarditis have been diagnosed with colon cancer, whereas other colon diseases, such as inflammatory colitis and polyps, have also been linked to streptococcal infection.Citation7 Streptococcus bovis is a common element of the intestinal microbiota in 5 to 10% of adults.Citation8 However, it can result in bacteremia and systemic infections, including IE (7 to 14% of cases) and septic arthritis.Citation9 While it is also an established, albeit rare, cause of meningitis in children, it is even rarer in adults.Citation10 Due to the connection between Streptococcus bovis infection and intestinal illness, it is deemed plausible that the patient’s hepatitis could be the origin of the infection in this instance.
IE is an infection of the endothelial cells of the heart which occurs in 3 to 10 individuals per 100,000 annually. The 30-day mortality rate can be up to 30%.Citation11 The epidemiology of IE has changed over time and Staphylococcus aureus is now the most common cause at approximately 26.6%,Citation12 followed by virome streptococci (18.7%), other streptococci (17.5%), and enterococci (10.5%).Citation13 The causes of IE comprise prosthetic valve implantation, different interventional procedures, cardiac surgery, intravenous drug addiction, antibiotic abuse, and degenerative valvular disease observed in geriatric patients.Citation14 The clinical signs of IE can vary widely, encompassing fever, heart murmur, and arterial embolism. These can be acute or progress rapidly, or they can be subacute or chronic, generally featuring a low-grade fever caused by pathogenic organisms and underlying cardiac disease. Approximately 90% of patients exhibit general symptoms such as fever, night sweats, fatigue, weight loss, and loss of appetite, with evidence of embolism present in around 25%. In patients exhibiting predisposing risk factors, heart murmurs, and vascular and embolic phenomena connected with IE, the possibility of IE should be carefully assessed.Citation15 Nonetheless, only 18.6% to 32.3% of IE demonstrating these common clinical manifestations have been documented in the literature.Citation16
Meningitis is a frequently occurring infectious disease affecting the central nervous system and is a leading cause of mortality. Haemophilus influenzae, Streptococcus pneumoniae, Streptococcus agalactiae, and Escherichia coli are common causative agents of meningitis. In adults, meningitis owing to Streptococcus bovis infection is exceedingly rare. Streptococcus gallolyticus is classified as a bovine streptococcus that belongs to group D streptococcus. The subspecies of Streptococcus gallates have been classified into three distinct groups by Schlegel et al.Citation17 Streptococcus gallolyticus, Streptococcus gallolyticus Macedonia, and Streptococcus gallate Pasteurii are medically significant. Streptococcus gallolyticus is an opportunistic pathogen that can cause various infections such as endocarditis, bacteremia, colorectal cancer, urinary tract infection, and peritonitis.Citation18 Most of the reported cases involve bacteremia, endocarditis, and gastrointestinal malignancy caused by Streptococcus gallolyticus subspecies gallolyticus, as well as neonatal and infant sepsis and meningitis caused by Streptococcus gallolyticus subsp. Pasteur.Citation19
However, meningitis in adults caused by streptococcus gallic acid is a relatively uncommon occurrence, with patients typically experiencing symptoms of endocarditis before meningitis. This particular patient represents the first reported case in China of an adult being diagnosed with IE caused by gallic acid streptococcus after presenting with meningitis symptoms.
Both meningitis and IE have serious consequences. A study that reviewed 41 adult cases of meningitis found a mortality rate of 27%, and 36% of surviving patients had neurological sequelae.Citation20 Similarly, a review of 15 children with IE found a mortality rate of 27%, and 73% of the children had embolism, of whom 5 (33%) had cerebral embolism.Citation21 Therefore, early diagnosis and treatment are crucial.
Conclusion
In summary, Streptococcus gallolyticus is a significant causative agent of meningitis and its incidence is frequently underestimated. It is a subtype of Streptococcus bovis. Most clinicians are presently unfamiliar with the biological classification and its identification methods, leading to clinical underestimation of Streptococcus bovis-associated diseases. Clinicians should focus on identifying and diagnosing diseases related to Streptococcus bovis and take prompt treatment measures. Similarly, patients diagnosed with endocarditis may also require early multidisciplinary consultation and active surgical intervention if medical treatment is inadequate.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethical Approval of Studies and Informed Consent
This study was approved by the University of Hong Kong-Shenzhen Hospital Ethics Committee (No. [2023]) and written informed consent was obtained from the patient. All authors have read the manuscript and approved its submission to the journal. This manuscript has the consent of the patient for the use of his data and for the publication of the data that appear in the article. All methods were carried out following the relevant guidelines and all methods were carried out under the Declaration of Helsinki.
Consent for Publication
All authors agree to publication.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
All authors declare that they have no competing interests for this work.
Acknowledgments
When we finish this paper, we want to express our heartfelt thanks to all those who helped us in the process of writing this paper. We also thank all the authors for their hard work and the University of Hong Kong-Shenzhen Hospital for giving us such a good opportunity.
Additional information
Funding
References
- Mills MT, Al-Mohammad A, Warriner DR. Changes and advances in the field of IE. Br J Hosp Med. 2022;83(3):1–11. doi:10.12968/hmed.2021.0510
- Gautam S, Sharma NR, Kansakar S, Lamichhane S, Pokhrel M, Basnet A. IE presenting as meningitis: a case report. Ann Med Surg. 2023;85(7):3638–3641. doi:10.1097/MS9.0000000000000895
- Peebles M, Roshani M, Srivastava K. Meningitis and endocarditis as a sequela of streptococcus pneumonia mastoiditis: a case report. Clin Case Rep. 2023;11(7):e7648. doi:10.1002/ccr3.7648
- Pigretti S, Zurrú MC, Arias A, Parcerisa F, Luzzi A, Belziti C. Endocarditis infecciosa: ¿Afectan su pronóstico las complicaciones neurológicas? [Neurologic complications of IE: do they have an impact on prognosis?]. Medicina. 2017;77(2):89–94. Spanish.
- Takarn P, Tharavichitkul P, Malasao R, Boonthum A. Characterization of erythromycin and tetracycline resistance genes of Streptococcus gallolyticus subspecies pasteurianus strains isolated from patients with septicemia and bacteremia in Thailand. Clin Lab. 2019;65(4). doi:10.7754/Clin.Lab.2018.180902
- Nguyen MT, Idriss S, Guzman E, De Oliveira ER. Neonatal meningitis, endocarditis, and pneumonitis due to Streptococcus gallolyticus subsp. pasteurianus: a case report. BMC Pediatr. 2019;19(1):265. doi:10.1186/s12887-019-1645-x
- Smith AH, Sra HK, Bawa S, Stevens R. Streptococcus bovis meningitis and hemorrhoids. J Clin Microbiol. 2010;48(7):2654–2655. doi:10.1128/JCM.02396-09
- Noble CJ. Carriage of group D streptococci in the human bowel. J Clin Pathol. 1978;31(12):1182–1186. doi:10.1136/jcp.31.12.1182
- Waisberg J, Matheus Cde O, Pimenta J. Infectious endocarditis from Streptococcus bovis associated with colonic carcinoma: case report and literature review. Arq Gastroenterol. 2002;39(3):177–180. doi:10.1590/s0004-28032002000300008
- Vilarrasa N, Prats A, Pujol M, Gason A, Viladrich PF. Streptococcus bovis meningitis in a healthy adult patient. Scand J Infect Dis. 2002;34(1):61–62. doi:10.1080/00365540110077128
- Mostaghim AS, Lo HYA, Khardori N. A retrospective epidemiologic study to define risk factors, microbiology, and clinical outcomes of IE in a large tertiary-care teaching hospital. SAGE Open Med. 2017;5:2050312117741772. doi:10.1177/2050312117741772
- Angstwurm K, Halle E, Wetzel K, Schultze J, Schielke E, Weber JR. Isolated bacterial meningitis is the key syndrome of IE. Infection. 2004;32(1):47–50. doi:10.1007/s15010-004-3103-3
- Rajani R, Klein JL. IE: a contemporary update. Clin Med. 2020;20(1):31–35. doi:10.7861/clinmed.cme.20.1.1
- Habib G, Lancellotti P, Antunes MJ, et al. Wytyczne ESC dotyczące leczenia infekcyjnego zapalenia wsierdzia w 2015 roku [2015 ESC Guidelines for the management of IE]. Kardiol Pol. 2015;73(11):963–1027. Polish. doi:10.5603/KP.2015.0227
- Toyoda N, Chikwe J, Itagaki S, Gelijns AC, Adams DH, Egorova NN. Trends in IE in California and New York State, 1998–2013. JAMA. 2017;317(16):1652–1660. doi:10.1001/jama.2017.4287
- Tornos P, Iung B, Permanyer-Miralda G, et al. IE in Europe: lessons from the Euro heart survey. Heart. 2005;91(5):571–575. doi:10.1136/hrt.2003.032128
- Schlegel L, Grimont F, Ageron E, Grimont PAD, Bouvet A. Reappraisal of the taxonomy of the Streptococcus bovis/Streptococcus equinus complex and related species: description of Streptococcus gallolyticus subsp. gallolyticus subsp. nov., S. gallolyticus subsp. macedonicus subsp. nov. and S. gallolyticus subsp. pasteurianus subsp. nov. Int J Syst Evol Microbiol. 2003;53(Pt 3):631–645. doi:10.1099/ijs.0.02361-0
- Jans C, Boleij A. The road to infection: host-microbe interactions defining the pathogenicity of Streptococcus bovis/Streptococcus equinus complex members. Front Microbiol. 2018;9:603. doi:10.3389/fmicb.2018.00603
- Takahashi Y, Ishiwada N, Tanaka J, et al. Streptococcus gallolyticus subsp. pasteurianus meningitis in an infant. Pediatr Int. 2014;56(2):282–285. doi:10.1111/ped.12254
- van de Beek D, de Gans J, Spanjaard L, Sela S, Vermeulen M, Dankert J. Group a streptococcal meningitis in adults: report of 41 cases and a review of the literature. Clin Infect Dis. 2002;34(9):e32–e36. doi:10.1086/339941
- Weidman DR, Al-Hashami H, Morris SK. Two cases and a review of Streptococcus pyogenes endocarditis in children. BMC Pediatr. 2014;14(1):227. doi:10.1186/1471-2431-14-227