Abstract
Purpose
Telehealth is associated with a myriad of benefits; however, little is known regarding substance use disorder (SUD) treatment outcomes when participants join group therapy sessions in a combination in-person and virtual setting (hybrid model). We sought to determine if treatment completion rates differed.
Patients and Methods
Policy changes caused by the COVID-19 pandemic created a naturalistic, observational cohort study at seven intensive outpatient (IOP) programs in rural Minnesota. Virtual-only delivery occurred 6/1/2020-6/30/2021, while hybrid groups occurred 7/1/2021-7/31/2022. Data was evaluated retrospectively for participants who initiated and discharged treatment during the study period. Participants were IOP group members 18 years and older who had a SUD diagnosis that both entered and discharged treatment during the 26-month period. A consecutive sample of 1502 participants (181–255 per site) was available, with 644 removed: 576 discharged after the study conclusion, 49 were missing either enrollment or discharge data, 14 transferred sites during treatment, and 5 initiated treatment before the study initiation. Helmert contrasts evaluated the impact of hybrid group exposure.
Results
A total of 858 individuals were included. Data was not from the medical chart and was deidentified preventing specific demographics; however, the overall IOP sample for 2020–2022, from which the sample was derived, was 29.8% female, and 64.1% were 18–40 years of age. For completed treatment, hybrid group exposure relative to virtual-only had a univariate odds ratio of 1.88 (95% CI: 1.50–2.41, p < 0.001). No significant difference was seen across IOP sites.
Conclusion
These results describe a novel hybrid group approach to virtual care for SUDs with outcome data not previously documented in the literature. While virtual treatment delivery can increase access, these results suggest a benefit is derived from including an in-person option. Further research is needed to identify how an in-person component may change dynamics and if it can be replicated in virtual-only models.
Introduction
Group therapy is a cornerstone of substance use disorder (SUD) treatment due to its effectiveness, practical design, and encouraging environment.Citation1–3 Research has supported in-person group therapy in reducing substance use, improving social functioning, and decreasing co-occurring mental health symptoms.Citation1,Citation4 During the COVID-19 pandemic, many SUD programs transitioned to virtual groups.Citation5 In 2015, a quarter of SUD treatment facilities offered telehealth services; by 2020 year-end, this increased to 58.6%.Citation6
Virtual groups increase accessibility, provide greater anonymity, and are cost-effective.Citation5 These factors may be particularly important for individuals in rural areas, working unconventional hours, or for whom transportation concerns impact treatment.Citation7 However, internet connection and platform malfunction can disrupt virtual group flow and decrease engagement.Citation5 Additionally, virtual groups may lack the social support that in-person groups provide.Citation8 Little is known about how to best enhance outcomes in virtually delivered SUD treatment.Citation5
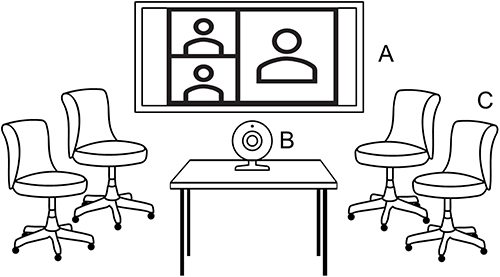
Following 2020 COVID-19 restrictions, Mayo Clinic Health System (MCHS) transitioned outpatient SUD group-based treatment to virtual-only treatment. Due to a 20% census drop during this time and reports that some participants were dissatisfied with virtual groups, we converted group rooms into teleconference rooms (see ). Patients could attend in person and see and interact with their “virtual group” members through a conference camera and large-screen television. We call this a “hybrid” model as patients attended both in person and remotely. We gathered data on treatment completion for the purpose of quality improvement.
Figure 1 Hybrid group therapy set-up.
Materials and Methods
Design
Virtual-only groups occurred 6/1/2020-6/30/2021, while hybrid groups occurred 7/1/2021-7/31/2022. The hybrid period was pre-defined as 13 months, matching the duration of virtual-only delivery. Three cohorts based on delivery-type exposure were naturalistically formed: virtual-only, hybrid-only, and those experiencing both conditions (“dually-exposed”). Participant discharge status was the primary outcome, defined as completed treatment (discharged with medical advice) or premature discharge, which included discharge against medical advice (AMA) and staff-requested discharge (SRD). AMA categorization occurred when participants stopped attending or notified staff they were terminating treatment despite recommendations; SRD would occur due to violence, threats, or similar safety concerns. If a participant’s treatment spanned both virtual-only and hybrid groups, they were classified as dually-exposed.
Participants
Participants were enrolled in intensive outpatient (IOP) SUD treatment at 1 of 7 sites (median population <30,000) affiliated with MCHS. IOP is group-based (8–12 participants), delivered 9 hours weekly for approximately 3 months. The program is abstinence-based (does allow medication for addiction treatment and nicotine/tobacco) and encourages medication management for co-occurring disorders with providers available. Participants complete treatment after sustained abstinence, completed assignments and consistent group attendance/participation. Referrals occur through social workers, other treatment programs, drug courts, and self-referral. Inclusion criteria were 18 years or older, a Diagnostic and Statistical Manual of Mental Disorders fifth edition SUD,Citation9 and enrolled in a MCHS IOP site. Exclusion criteria were if treatment began prior to transition to virtual-only or if discharged after the predetermined study end. Due to deidentification, specific sample characteristics are unavailable. However, displays IOP demographics for 2020–2022, which is the population the study cohort is from.
Table 1 Mayo Clinic Health System Intensive Outpatient Program Participanta
Statistical Analysis
Helmert contrasts evaluated the effects of hybrid delivery. Virtual-only participants were contrasted with participants either in hybrid-only or dually-exposed (HC1). Then, hybrid-only participants were contrasted with dually-exposed participants (HC2). Logistic regression assessed the effect of group (virtual-only, hybrid-only, dually-exposed) on outcome (discharge status) while initially controlling for treatment site however it was removed due to non-significance. Two degrees of freedom (df) (ie, 3 groups) log-likelihood chi-square test compared differences across groups. Odds ratio confidence interval and p-value were obtained through the described logistic regression.
Analyses were performed using R 4.2.1Citation10 with packages car, dplyr, and lubridate. The MCHS IRB deemed this study exempt due to retrospectively analyzed deidentified data originally collected for quality improvement purposes. Patient informed consent was therefore waived by the IRB. This study complies with the Declaration of Helsinki.
Results
Originally there were 1502 participants across 7 sites (181–255 participants per site). After inclusion/exclusion criteria, 644 participants were removed due to the following:
343 discharged after the predefined study endpoint.
233 entered during the hybrid period, however, were in treatment at time of analysis and therefore had no discharge status.
49 were missing enrollment or discharge dates.
14 transferred sites during the study.
5 began treatment prior to the transition to virtual-only groups.
The IOP sample was predominantly White, male, and 18 to 40 years old (). Descriptive measures are seen in . More participants were exposed to hybrid delivery due to the naturalistic study design. HC1 displayed an advantage for hybrid-delivery relative to exclusively virtual-only for completed treatment with OR = 1.88 (95% CI: 1.5–2.37). HC2 displayed an advantage to those dually-exposed relative to those exclusively in the hybrid model for completed treatment with OR = 1.99 (95% CI: 1.65–2.41). For logistic regression, both HC1 (estimate: 0.631, SE: 0.117, p < 0.0001) and HC2 were highly significant (estimate: −0.686, SE: 0.097, p < 0.0001). Likelihood ratio tests showed a significant difference across both HC1 (χ2 = 31.03, df = 1, p-value < 0.0001) and HC2 (χ2=53.38, df = 1, p-value < 0.0001).
Table 2 Descriptive Measures
Discussion
Although many studies have reported benefits with virtual group therapy, this is the first to our knowledge that suggests incorporating an in-person option may enhance those services for SUD treatment. While telehealth increases access and is rapidly scalable,Citation6,Citation11 it remains unclear how removing the in-person component may impact group dynamics such as therapeutic alliance (TA), cohesiveness and overall satisfaction.Citation8,Citation12
The dually-exposed group had a high treatment completion rate, which may reflect a benefit derived following the intervention change. Rates of completed treatment were low for the sample, however, with approximately one-third of all participants meeting that criterion. An analysis of the 2011 Treatment Episode Data Set: Discharge (TEDS-D) database found that 52% of individuals discontinued in person outpatient SUD treatment.Citation13 COVID-19 may have contributed to our studies lower rates of completed treatment, as postponing or avoiding medical care during the pandemic became increasingly common.Citation14
Bronson et al reviewed 122 studies, including nearly 200,000 participants, and found risk factors for SUD treatment discontinuation included low rates of TA.Citation15 TA, or the participants reported connection to their counselor/group facilitator, has been shown to be an important factor across psychotherapy interventions.Citation16 It is unclear how differing SUD treatment delivery may impact TA. Drawing from non-SUD literature, in a cohort of 291 Spanish adults with primarily affective disorders seeking individual therapy, those engaging virtually reported delayed growth in TA as compared to those treated in-person.Citation17 Specific to group therapy, overall cohesiveness of the group, or the level of connection between group members, may also be impacted by virtual groups. This literature is limited however, with previous small studies (samples of 35 and 58) reporting either lower levels of group cohesionCitation18 or increased difficulty connecting with other group members.Citation19
Participant autonomy for how one received treatment may have also been important. The hybrid model allowed participants to express a choice in how they received treatment. This may have enhanced a pro-recovery environment.Citation20 The loss of free will, such as in compulsory, or court-mandated treatment, may be effective for some, however existing evidence calls into question its long-term effectiveness.Citation21 Stigma related to SUDs is also diverse in constructCitation22 with a longitudinal impact.Citation23 Not mandating a certain treatment approach may have allowed hybrid participants to tolerate this with less difficulty.
The interpretation of these results does not question the utility of telehealth. Rather, they propose the thoughtful use of virtual visits in conjunction with in-person options rather than an all-or-none approach. The Consolidated Appropriations Act extended the flexibility afforded to Medicare recipients following COVID-19 for receiving telehealth services through 2024.Citation24 While recommendations vary across healthcare and specialties regarding how often to see patients in-person, further research is needed on the long-term implications of exclusively virtual care, particularly in a group setting. This research may identify what an in-person component adds, and if this could be replicated somehow in virtual-only care.
Limitations
Deidentification prevented controlling for demographics and specific SUDs, which limits generalizability. To maximize data, we grouped hybrid-only and dually-exposed in the comparison with virtual-only; this may have introduced bias, however is consistent with Helmert contrasts. Additionally, data does not exist for hybrid groups at the participant level regarding how often an individual joined virtually versus in-person. Our experience was that there was a fairly even mix of participants who always came in person, some who always attended virtually and those who’s attendance would vary; however, we do not have data to quantify this observation. Therefore, the intervention was “exposure to the hybrid model” and not a reflection on how each participant individually attended the hybrid groups. As this was a naturalistic study, virtual groups occurred earlier and hybrid subsequently later in time. Environmental factors like changes in COVID restrictions may have increased people’s willingness to stay in treatment regardless of treatment delivery options. Finally, as these sites are in a rural setting, it is unclear how these results may translate to a metropolitan-based sample.
Conclusion
This is the first report in the scientific literature to show that a hybrid group model that includes a combined in-person and virtual treatment option is not worse and may enhance rates of completed treatment relative to virtual-only SUD groups. Future prospective studies are needed to evaluate the potential enhancement of virtual delivery by the incorporation of an in-person option. While telehealth has many advantages, in-person options may help augment the treatment experience.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- American Psychiatric Association. Practice guideline for the treatment of patients with substance use disorders: alcohol, cocaine, opioids. Am J Psychiatry. 1995;152(11 Suppl):1–59. doi:10.1176/ajp.152.11.1
- Lopez G, Orchowski LM, Reddy MK, Nargiso J, Johnson JE. A review of research-supported group treatments for drug use disorders. Subst Abuse Treat Prev Policy. 2021;16(1):51. doi:10.1186/s13011-021-00371-0
- Weiss RD, Jaffee WB, de Menil VP, Cogley CB. Group therapy for substance use disorders: what do we know? Harv Rev Psychiatr. 2004;12(6):339–350. doi:10.1080/10673220490905723
- de Andrade D, Elphinston RA, Quinn C, Allan J, Hides L. The effectiveness of residential treatment services for individuals with substance use disorders: a systematic review. Drug Alcohol Depend. 2019;201:227–235. doi:10.1016/j.drugalcdep.2019.03.031
- Oesterle TS, Kolla B, Risma CJ, et al. Substance use disorders and telehealth in the COVID-19 pandemic era: a new outlook. Mayo Clin Proc. 2020;95(12):2709–2718. doi:10.1016/j.mayocp.2020.10.011
- Alvarado HA Telemedicine services in substance use and mental health treatment facilities. The CBHSQ Spotlight; 2021. Available from: https://www.samhsa.gov/data/report/telemedicine-services. Accessed April 22, 2024.
- Barak K, Hen L, Boniel-Nissim M, Shapira N. A comprehensive review and a meta-analysis of the effectiveness of Internet-based psychotherapeutic interventions. J Technol Human Serv. 2008;26(2–4):109–160. doi:10.1080/15228830802094429
- Hedman E, Ljotsson B, Kaldo V, et al. Effectiveness of Internet-based cognitive behaviour therapy for depression in routine psychiatric care. J Affect Disord. 2014;155:49–58. doi:10.1016/j.jad.2013.10.023
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
- R Foundation for Statistical Computing. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; 2022.
- Shaver J. The state of telehealth before and after the COVID-19 pandemic. Prim Care. 2022;49(4):517–530. doi:10.1016/j.pop.2022.04.002
- Riper H, Andersson G, Christensen H, Cuijpers P, Lange A, Eysenbach G. Theme issue on e-mental health: a growing field in internet research. J Med Internet Res. 2010;12(5):e74. doi:10.2196/jmir.1713
- Stahler GJ, Mennis J, DuCette JP. Residential and outpatient treatment completion for substance use disorders in the U.S.: moderation analysis by demographics and drug of choice. Addict Behav. 2016;58:129–135. doi:10.1016/j.addbeh.2016.02.030
- Czeisler ME, Marynak K, Clarke KEN, et al. Delay or Avoidance of medical care because of COVID-19-related concerns - United States. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250–1257. doi:10.15585/mmwr.mm6936a4
- Brorson HH, Ajo Arnevik E, Rand-Hendriksen K, Duckert F. Drop-out from addiction treatment: a systematic review of risk factors. Clin Psychol Rev. 2013;33(8):1010–1024. doi:10.1016/j.cpr.2013.07.007
- Fluckiger C, Del Re AC, Wampold BE, Horvath AO. The alliance in adult psychotherapy: a meta-analytic synthesis. Psychotherapy. 2018;55(4):316–340. doi:10.1037/pst0000172
- Mercadal Rotger J, Cabre V. Therapeutic alliance in online and face-to-face psychological treatment: comparative study. JMIR Ment Health. 2022;9(5):e36775. doi:10.2196/36775
- Lopez A, Rothberg B, Reaser E, Schwenk S, Griffin R. Therapeutic groups via video teleconferencing and the impact on group cohesion. Mhealth. 2020;6:13. doi:10.21037/mhealth.2019.11.04
- Sugarman DE, Busch AB, McHugh RK, et al. Patients’ perceptions of telehealth services for outpatient treatment of substance use disorders during the COVID-19 pandemic. Am J Addict. 2021;30(5):445–452. doi:10.1111/ajad.13207
- Williamson L. Creating an ethical culture to support recovery from substance use disorders. J Med Ethics. 2020;47(12):e9. doi:10.1136/medethics-2020-106661
- Werb D, Kamarulzaman A, Meacham MC, et al. The effectiveness of compulsory drug treatment: a systematic review. Int J Drug Policy. 2016;28:1–9. doi:10.1016/j.drugpo.2015.12.005
- Kulesza M, Larimer ME, Rao D. Substance use related stigma: what we know and the way forward. J Addict Behav Ther Rehabil. 2013;2(2). doi:10.4172/2324-9005.1000106
- Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J Health Soc Behav. 1997;38(2):177–190. doi:10.2307/2955424
- HHS fact sheet: telehealth flexibilities and resources and the COVID-19 public health emergency. U.S. Department of Health and Human Services; 2023. Available from: https://www.hhs.gov/about/news/2023/05/10/hhs-fact-sheet-telehealth-flexibilities-resources-covid-19-public-health-emergency.html#:~:text=Medicare%20and%20Telehealth&text=The%20Consolidated%20Appropriations%20Act%2C%202023%2C%20extended%20many%20Medicare%20telehealth%20flexibilities,than%20only%20in%20rural%20areas. Accessed August 26, 2023.

