Abstract
Aim: We utilized the National Cancer Database to describe the treatment trends in brain metastases from primary testicular cancers. Methods: We analyzed data from the NCDB from 2010 to 2015 for patients with both primary testicular cancers and brain metastases who were treated with brain-directed radiation. We performed multivariable logistic and cox regressions to identify predictors of treatment type and overall survival respectively. Results: Most patients meeting the above criteria received whole brain radiation therapy as opposed to stereotactic radiosurgery (SRS). Predictors of improved survival were age, private insurance coverage, receipt of chemotherapy, and receipt of SRS. The 5-year survival rate was highest for patients who received SRS. Conclusion: This study confirms significantly improved overall survival with the use of SRS.
Plain language summary
Testicular cancer is quite rare, making up just 1% of solid cancers found in men every year. Even rarer is the situation where this cancer spreads to the brain. When this happens, it can be treated in a few different ways: surgery, radiation to the entire brain, a focused type of radiation called stereotactic radiosurgery, or a combination of these methods. Due to its rarity, there isn’t a clear-cut best approach for treating these brain tumors. In our research, we used a massive database, the National Cancer Database (NCDB), to get a clearer picture of this issue. We looked at patients diagnosed with testicular cancer between 2004 and 2015 who also had at least one tumor in the brain. By analyzing this information, we could compare the survival outcomes of patients based on the type of treatment they received and other factors.
We found that brain tumors from testicular cancer are very rare, found in just 0.4% of the patients we studied. We also found that treatment with either focused radiation, whole brain radiation, or chemotherapy significantly improves survival rates compared with no treatment. In addition, focused radiation, called stereotactic radiosurgery, might result in even better survival results than radiation to the entire brain. Receiving this focused radiation was more common in patients who also had tumors in other parts of their body. While our study gives essential insights, it does have some limitations. The database we used doesn’t provide specific details like the size of the brain tumors, the exact treatment doses, and some other crucial patient information. This means that while we now have a better overall picture, more research is needed to give patients and doctors a complete understanding.
Tweetable abstract
Utilizing the National Cancer Database (2010–15), our study on brain metastases from testicular cancers reveals SRS improves overall survival more than whole brain radiation therapy.
Cancers of testicular origin are quite rare, accounting for 1% of solid male cancers annually, with an exceptional five-year survival rate often surpassing 95% [Citation1]. Even more rare is the presence or development of brain metastases from a primary testicular cancer, a situation which shifts both prognosis and treatment options. Treatment options for brain metastases from a testicular primary cancer mirror those which arise from more common primary malignancies: surgical resection, whole brain radiation (WBRT), stereotactic radiosurgery (SRS) or some combination thereof [Citation2–4]. A clear consensus on how to treat brain metastases from testicular cancers does not yet exist, likely due to the rarity of the condition and associated lack of treatment data. A recent single-institution study of 63 patients recently found that higher levels of biologically effective dose of radiation therapy were associated with both overall survival and intracranial control of tumors [Citation5]. However, the study was unable to draw conclusions on the relative survival impact of different forms of brain-directed radiation due to the very small sample size of patients treated for SRS at the institution. We used the National Cancer Database (NCDB) to better characterize how often brain metastases are present at the time of diagnosis of testicular cancer, the relative effectiveness of SRS in comparison to WBRT, and to help develop current practice patterns that exist in the management of brain metastases from testicular primary cancers. Using the NCDB, we conducted the largest multi-institution analysis of the treatment of these rare metastases that currently exists in scientific literature. In addition, we wanted to examine survival outcomes in these patients, compare them to historical outcomes from other primary malignancies, and identify any predictors which may contribute to them.
Materials & methods
This project focused on a retrospective review of the NCDB, which is exempt from IRB review due to the de-identified nature of the dataset. The NCDB dataset is sourced from over 1,500 facilities and accounts for over 72% of newly diagnosed cancers in the US each year [Citation6]. We are required to state that the Commission on Cancer and the American College of Surgeons did not verify the analytic or statistical methodology used, nor are they responsible for the methodology and conclusions drawn from these data by the investigators.
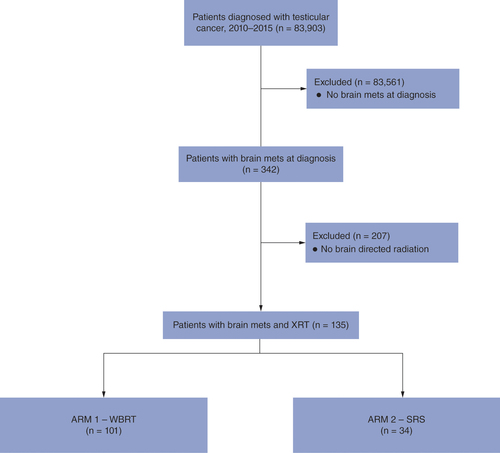
We queried the NCDB for patients diagnosed with cancer of testicular origin during the years 2004–2015 who also had at least one brain metastasis at the time of diagnosis. Of note, the NDCB did not record brain metastases until 2010, thus limiting our dataset to 2010–2015. We then further subdivided this group into those that did and did not receive brain-directed radiation. This was possible because the NCDB includes data on the anatomic target of radiation. We also captured data on delivery of chemotherapy, which in the NCDB, is simply coded as a ‘yes’ or ‘no’; there is no data on type of systemic therapy or number of cycles delivered. The overall selection process for this study is outlined in .
Radiotherapy treatments included whole brain radiation therapy and stereotactic radiosurgery.
Mets: Metastases; SRS: Stereotactic radiosurgery; WBRT: Whole brain radiation therapy; XRT: Radiotherapy.
A variety of demographic and socioeconomic variables are included in the NCDB dataset and were incorporated into our analysis. All patients had their primary cancers diagnosed between 2010–2015. These cancers were characterized as being either seminoma or non-seminoma in origin according to ICD-O-3 histology codes [Citation7]. The median age of the cohort was 28 years, and patients were grouped according to their age in relation to the median. Race was subcategorized as White, Black and other. Quantification of comorbidities used the Charlson/Deyo comorbidity index. Patients were distinguished as having extracranial disease if bone, lung or liver metastases were also present at time of primary cancer diagnosis. The presence of metastases at other sites is unknown because the NCDB only supplies data on the presence of bone, lung and liver metastases while providing no information on quantity or quality of the metastases. Patients’ areas of residence were designated metro, urban, or rural based on population size and degree of urbanization data as outlined by the USDA economic research service. Patient distance from their treatment facility was also recorded as being above or below the average patient distance from a facility, 38.9 miles for this cohort. Insurance status was also included in the dataset. Patients were categorized as being uninsured, having private insurance, or having government insurance. Finally, patients were categorized as receiving whole brain radiation therapy (WBRT), stereotactic radiosurgery (SRS), chemotherapy alone, or no treatment–however, dosage information was not incorporated into the data analysis. Groupings were based on treatment type received with the goal of being able to compare overall survival between groups and to identify significant predictors of treatment type. Grouping based on histologic subtype of primary cancer was not pursued due to the small sample size of individuals with seminomatous cancers compared with those with non-seminomatous ones, preventing a robust comparative analysis between groups based on histologic subtype. Data were analyzed using Medcalc Version 20.106 (Belgium), and baseline characteristics were tabulated. Multivariable logistic regression was performed using patient characteristic data to determine significant predictors of administration of SRS in comparison to WBRT. Cox regression was then performed using the same variables, in addition to treatment type, to produce hazard ratios predictive of death. Confidence intervals of 95% were reported, and a level of 0.05 was used as an indicator of statistical significance. Kaplan-Meier curves were generated to show overall probability of survival over time, as well as differences in survival probability with respect to the treatment received.
Results
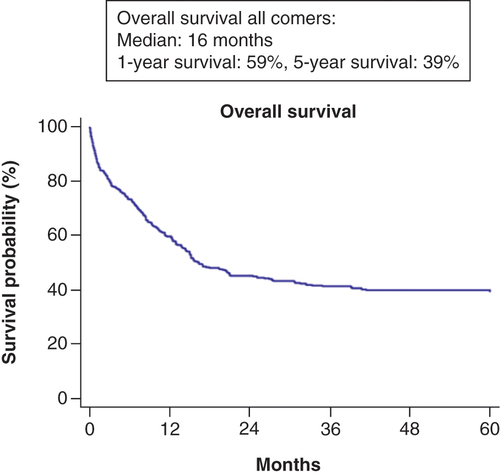
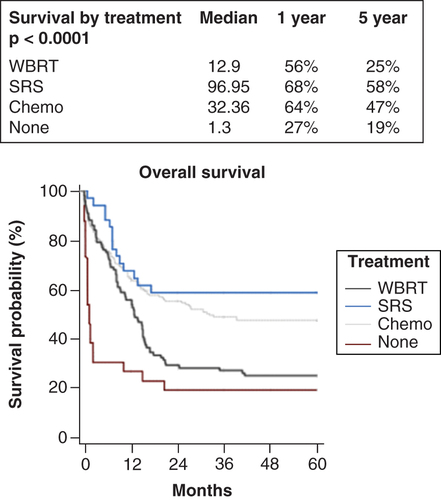
In total, 342 patients with brain metastases at diagnosis were identified as meeting the selection criteria above. Their baseline characteristics are shown in . The majority (329, 96%) of patients had primary cancers of non-seminoma origin. The median age was 28 years (range: 18–83 years). Forty percent (135) of the patients received brain directed radiation, most often in the form of WBRT (75% of brain directed radiation). The median time to radiation was 28.5 days (Range: 0–239 days). The median WBRT dose was 3000 cGy in 10 fractions (1800–5400 cGy) while the median SRS dose was 2400 cGy in 1 fraction (380–4890 cGy). In addition, 91% of patients were diagnosed with other extracranial metastatic diseases, and 89% of patients received systemic therapy in the form of chemotherapy. The multivariable logistic regression of baseline patient characteristics () showed that presence of extracranial disease was a significant predictor of receipt of SRS, meaning that patients with extracranial disease were significantly more likely to receive SRS than patients without extracranial disease (). Multivariable Cox regression showed that significant predictors of improved survival include receipt of SRS and receipt of chemotherapy in comparison to receipt of only WBRT, as well as age greater than 28 years (). The median survival rate of the patient cohort was 16 months, with a 1-year survival rate of 59% and a 5-year survival rate of 39% (). Patients who received WBRT saw a reduced 5-year survival rate when compared with those who received SRS or chemotherapy (25, 58 and 47% respectively). The median survival time for patients with seminomatous primary malignancies was 50.2 months, and those with non-seminomatous primary malignancies had a median survival time of 15.2 months. Recipients of WBRT, SRS and no treatment had a median survival time of 12.9 months, 97.0 months and 1.3 months, respectively ().
Table 1. Characteristics of patients with primary testicular cancer and brain metastases.
Table 2. Multivariable logistic regression for receipt of stereotactic radiosurgery.
Table 3. Multivariable Cox regression for predictors of survival.
Median survival was 16 months. Survival at 1 and 5 years was 59% and 39%, respectively.
The highest 5-year survival rate was observed in patients receiving SRS (58%), followed by chemotherapy (47%) and WBRT (25%) compared with untreated patients (19%).
Chemo: Chemotherapy; SRS: Stereotactic radiosurgery; WBRT: Whole brain radiation therapy.
Discussion
We compared 1- and 5-year OSs of testicular cancer patients with brain metastases treated with chemotherapy, WBRT, and SRS to determine which treatment was most predictive of survival. As stated in our results, the incidence of brain metastases at the diagnosis of primary testicular cancer is quite low, evident in just 0.4% of patients in our study. This rarity underscores the importance of specialized care and insights for such patients. As expected, we found a significant survival benefit to receiving chemotherapy, WBRT, or SRS when compared with receiving no treatment at all. In addition, we showed a likely benefit to SRS when compared with WBRT as seen in terms of 5-year survival probability. However, this benefit may be attributable to the notion that recipients of SRS might have fewer lesions, less extracranial burden, and better performance status, resulting in better initial survival probabilities. These potentially confounding variables are unable to be explored further due to the limited amount of patient data recorded in the NCDB.
In addition, only 40% of patients in the study were listed as having received brain directed radiation. This may be because the NCDB does not record “salvage” WBRT, so it is possible that recipients of salvage therapy were recorded as receiving no brain directed radiation at all despite receiving it after initial systemic therapy. This notion is perhaps supported by times in excess of 200 days for administration of radiation seen in the dataset. It is also possible that the data reflect real-world practice and that brain-directed radiation is less commonly used in patients with primary testicular cancer than in patients with other primary solid malignancies. The presence of extracranial disease at time of diagnosis of brain metastasis was a significant predictor for receipt of SRS (), although the reason behind its predictive power remains unclear due to the NCDB’s lack of specific data on each patient’s unique brain metastasis profile. Predictors of improved survival were receipt of chemotherapy, receipt of SRS, and age over 28 years (). The difference in median survival time between patients with seminomatous and non-seminomatous brain metastases was an interesting finding. The difference may be due to the small sample size of seminomatous patients presenting with brain metastases at time of diagnosis, or that the brain metastases from non-seminoma primary cancers result in worse prognosis than seminomatous metastases to the brain. However, the NCDB does not supply information on size or number of metastases for each patient, so a comparative conclusion on the lethality of the two types of brain metastases cannot be drawn from the dataset.
A few similar comparable retrospective studies have been conducted, all with much smaller sample sizes. One study examined eight patients who were identified as having intracerebral metastases as a result of primary testicular cancer [Citation8]. The goal of the analysis was to better understand patient survival time after brain-directed radiation as precisely as possible. All patients received WBRT and witnessed a 12-month survival rate in the range 60–67%, depending on radiation dose and schedule, which varies slightly in comparison to the 56% survival rate in our cohort. This discrepancy is likely due to the small sample size used in the other study. We expanded on their analysis by determining the 12-month survival rate for patients receiving SRS as opposed to WBRT, which was 68% with an impressive median survival time of about 96 months.
An older report summarized outcomes of patients with brain metastases at time of diagnosis with testicular cancer, which represented 41% of patients in that group [Citation9]. This analysis, done at Hannover University Medical School, determined that patients who received either chemotherapy or radiotherapy saw poor long term survival rates, while those treated with a combination of the two saw better long-term survival. The team concluded that only around 25% of all patients with brain metastases from testicular cancer would be able to achieve long term survival when treated with both chemotherapy and brain-directed radiation. Their figure is far lower than observed in our retrospective analysis of patients treated with SRS (58%) but on par with the survival rate seen in patients treated with WBRT (25%).
There are a few study limitations due to the retrospective nature of the NCDB. A significant selection bias may be present in terms of radiation treatment. The NCDB also does not specify the amount or size of brain metastases present at diagnosis, which would influence both delivered treatment type and eventual outcome. Nor does the NCDB indicate if any patients received surgical intervention for their brain metastases, which can potentially influence outcome. There is no information on the types of systemic agents used, or the number of cycles delivered, which would also impact survival. Furthermore, the NCDB also lacks information on detailed outcomes relevant to this study type that are important in treating patients with brain metastases, such as local failure, toxicity, salvage therapy, and distant brain failure [Citation10]. With these limitations in mind, this project was meant to serve as an analysis of the incidence and trends in treatment for patients with brain metastases as a result of testicular primaries rather than as a comparison of multiple treatment techniques.
Conclusion
Brain metastases resulting from primary testicular cancer, though rare, represent a unique subset of patients requiring specialized therapeutic considerations. This comprehensive study, leveraging the National Cancer Database, is the most extensive of its kind, shedding light on the current practices and potential survival outcomes related to treatment modalities for these patients. The results suggest a notable survival benefit in receiving either chemotherapy, WBRT, or SRS compared with no treatment, with SRS possibly offering superior outcomes to WBRT. In addition, the only clinically significant predictor of patients receiving Stereotactic Radiosurgery (SRS) included the presence of extracranial disease at the time of diagnosis, making it apparent that the presence of distant metastases might impact therapeutic choices. This information can serve as a platform for further research, elucidating whether treatment approaches should be revised based on the full metastatic profile of the patient. Nevertheless, the presence of various confounding factors, largely due to the limitations inherent to the NCDB, may influence these findings. Important variables such as the size and quantity of brain metastases, exact therapeutic regimens, and specific patient profiles remain obscured. Thus, while this study provides essential insights into treatment patterns and their associated outcomes, further detailed and prospective studies are necessary to draw more definitive conclusions on the optimal treatment strategy for testicular cancer patients with brain metastases. Future studies might aim to consider these factors, focusing on individualized patient-centric approaches for this specific cancer subtype.
Testicular cancers are rare, accounting for 1% of solid male cancers, with a 5-year survival rate surpassing 95%. Brain metastases from these cancers are even rarer and affect prognosis and treatment options.
Common treatments for brain metastases from testicular primary cancers include surgical resection, whole brain radiation (WBRT), stereotactic radiosurgery (SRS), or combinations of these methods.
There is no clear consensus on treatment due to the rarity of the condition and the lack of data.
A study using the National Cancer Database (NCDB) sought to understand the frequency of brain metastases at the time of testicular cancer diagnosis and to compare the effectiveness of SRS and WBRT.
The study identified 342 patients with brain metastases from a testicular primary cancer, the majority of which were non-seminoma cancers. Out of these, 40% received brain-directed radiation, most often in the form of WBRT.
Results showed that patients receiving SRS had better 5-year survival probabilities than those treated with WBRT.
Predictors of better survival were treatment with chemotherapy, treatment with SRS, and age above 28 years.
This comprehensive analysis provided insights into treatment patterns and outcomes but is limited by the lack of detailed patient profiles, treatment regimens, and other variables.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Medical writing support was provided by the Health System Publication Support Office (HSPSO), an internal service funded by Allegheny Health Network and to be used by researchers employed by Allegheny Health Network.
Ethical conduct of research
This project focused on a retrospective review of the NCDB, which is exempt from IRB review due to the de-identified nature of the dataset.
Acknowledgments
The authors thank S Carey, MS, J Chang and J Newman of Allegheny Health Network’s Health System Publication Support Office (HSPSO) for their assistance in editing and formatting the manuscript. The HSPSO is funded by Highmark Health (PA, USA) and all work was done in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Additional information
Funding
References
- NaumanM, LeslieSW. Nonseminomatous testicular tumors. StatPearls [Internet]. (2022). https://www.ncbi.nlm.nih.gov/books/NBK568754/
- MarkAJ, KimCS. Brain metastasis. StatPearls [Internet]. (2022). https://www.ncbi.nlm.nih.gov/books/NBK470246/
- MD Anderson Cancer Center. Brain metastases [Internet]. https://www.mdanderson.org/cancer-types/brain-metastases.html
- LinX, DeAngelisLM. Treatment of brain metastases. J. Clin. Oncol.33(30), 3475–3484 (2015).
- CaseyDL, PitterKL, ImberBSet al. High-dose radiation therapy is needed for intracranial control and long-term survival in patients with non-seminomatous germ cell tumor brain metastases. J. Neurooncol.142(3), 523–528 (2019).
- American College of Surgeons. National cancer database [Internet]. https://www.facs.org/quality-programs/cancer/ncdb
- IACR. IACR official website – International Association of Cancer Registries [Internet] (2022). http://www.iacr.com.fr/index.php?option=com_content&view=category&layout=blog&id=100&Itemid=577
- RadesD, DziggelL, VeningaTet al. Overall survival after whole-brain radiation therapy for intracerebral metastases from testicular cancer. Anticancer Res.36(9), 4817–4820 (2016).
- BokemeyerC, NowakP, HauptAet al. Treatment of brain metastases in patients with testicular cancer. J. Clin. Oncol.15(4), 1449–1454 (1997).
- WegnerR, BerginJ, HorneZ. Diagnosis and treatment of brain metastases in patients with gynecologic malignancies. Gynecol. Oncol.158(1), e11–e12 (2020).

