 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Event centrality is defined by the extent to which a memory of an event has become central to an individual’s identity and life story. Previous research predominantly focused on the link between event centrality and trauma-related symptomatology. Nevertheless, it can be argued that the perception of (adverse) events as central to one’s self is not exclusive to Posttraumatic Stress Disorder (PTSD). Other disorders where adverse events are linked to the onset of symptoms might also be related to event centrality. This study examined the relevance of event centrality for Social Anxiety Disorder (SAD) and for Major Depressive Disorder (MDD) separately. Moreover, we examined which cognitive and emotion regulation variables (i.e., trait anxiety, rumination, worry, intrusions and avoidance, and posttraumatic cognitions) mediated these relationships. No significant correlation was found between event centrality and social anxiety. However, a significant positive correlation was found between event centrality and depression. In a combined group, this relation was mediated by all cognitive and emotion regulation variables except for worry.
Event centrality is defined by the extent to which a memory of an event has become central to the individual’s identity and life story. Berntsen and Rubin (Citation2006) proposed that the memory of a traumatic event can form a cognitive reference point in autobiographical knowledge and thereby influence the interpretation of past experiences and expectations for future events. Conceptually, event centrality consists of three aspects: (1) the event is seen as a turning point in life; (2) the event is seen as a reference point for understanding other everyday experiences; (3) the event has become part of the life story and identity. The majority of research on event centrality has centred on its association with trauma-related symptomatology, revealing strong positive correlations with intrusions, avoidance, posttraumatic cognitions, and rumination (Berntsen & Rubin, Citation2006, Citation2007; Boals, Citation2010; Brown et al., Citation2010; Gehrt et al., Citation2018; Vermeulen et al., Citation2019). Moreover, the relation between event centrality and Posttraumatic Stress Disorder (PTSD) symptoms may be mediated by these variables (Boelen, Citation2012b; Lancaster et al., Citation2011; Vermeulen et al., Citation2019).
Onset-event-related disorders and event centrality
From a broader theoretical perspective, it is proposed that the perception of (adverse) events as central to one’s identity is not confined solely to PTSD. Other psychological disorders, in which adverse events have been associated with the onset of symptoms might also be related to event centrality. For example, experiences of negative life events (in combination with feelings of shame; Magee, Citation1999), recurrent experiences of negative social situations (e.g., bullying, rejection, humiliation, or exclusion by significant others), and the experience of childhood trauma (De Venter et al., Citation2017) have a significant effect on the development and maintenance of Social Anxiety Disorder (SAD; Rapee & Spence, Citation2004). Moreover, there is a substantial causal relationship between stressful life events and the onset of Major Depressive Disorder (MDD; Kendler et al., Citation1999; Kessler, Citation1997; McCutcheon et al., Citation2009). More specifically, a large body of research has shown a strong relationship between childhood abuse and MDD (Maniglio, Citation2010; Wiersma et al., Citation2009). Taken together, while the diagnosis of PTSD presupposes a traumatic experience, other psychological disorders like SAD and MDD do not necessarily require a specific traumatic event for classification based on DSM criteria. It is crucial, however, to differentiate between the classification criteria outlined in the DSM and the aetiology of a disorder. In the case of PTSD, the diagnosis is explicitly linked to the experience of trauma, whereas for disorders such as SAD and MDD, the origins of symptoms may be more varied, involving a person’s history and the evaluation of key learning moments including adverse events (for an overview, see Beck, Citation2008; Rapee & Spence, Citation2004). This broader perspective suggests that adverse events can still exert a significant impact on symptom development across various psychological disorders.
Therefore, it seems plausible that the event centrality of adverse events would also be related to the onset of SAD and MDD. When the memories of these adverse events become central to the individual, such memories could become a turning point in life, a reference point for understanding neutral, everyday experiences, and part of the life story and identity. This, in turn, could have a continuous impact on how individuals see themself and the world.
SAD and event centrality
Cognitive models of SAD (Clark & Wells, Citation1995; Hofmann, Citation2007; Rapee & Heimberg, Citation1997; Rapee & Spence, Citation2004) converge on the idea that there is a bi-directional relationship between maladaptive cognitions and negative social experiences: The individual underestimates its social abilities and has a biased negative self-representation (Hofmann, Citation2007). This can lead to a feeling of underachieving in social situations, which, on the one hand, is potentially reinforced by an attentional bias towards negative feedback (Clark & Wells, Citation1995). On the other hand, it could also lead to an interpretation bias, where neutral, non-threatening social situations are interpreted as threatening. This, in turn, could evoke behavioural changes, e.g., avoidance of certain social situations and post-event rumination (Hofmann, Citation2007). Experiencing recurrent negative social events like bullying, rejection, humiliation, or exclusion will reinforce or strengthen these maladaptive cognitions (Rapee & Spence, Citation2004). Also, the engagement in avoidance and safety behaviours, in combination with rumination, can be expected to lead to a vicious circle, ultimately maintaining and further exacerbating social anxiety symptoms (Hofmann, Citation2007).
The negative social events might be seen as a reference point for other experiences, where the memory is appraised as an anchoring event. The memory of the negative social event colours neutral memories in hindsight and can continuously impact the expectations for future situations. Also, the negative social event may become part of the individual’s identity; e.g., the individual appraises themselves as someone who does not perform well in social situations. In turn, these appraisals can lead to lower social performance, thereby maintaining social anxiety. Thus, when the individual appraises the memory of a negative social (onset) event as central, this could fuel the development of SAD.
MDD and event centrality
Following Beck’s cognitive model of depression (Beck, Citation1967), the occurrence of negative events can lead to the development of depressive self-referential schemas and dysfunctional attitudes. Negative events, such as the loss of a significant person, or underperforming at certain key moments, act as catalysts in the development of maladaptive self-referential schemas. In these schemas, the meaning attributed to the event becomes deeply ingrained as stable attitudes, integrated into personal identity. For example, beliefs like “if I lose an important person, I’ll be helpless”, or “if I fail at something, it means I’m a total failure” become established. Once these schemas take root, they dynamically interact with an individual’s perception of subsequent events, predisposing them to interpret new situations in alignment with their negative attitudes, serving as a reference point for everyday inferences. The activation of a maladaptive self-referential schema can contribute to an increased vulnerability to depression, acting as a filter through which individuals perceive and evaluate the world. Moreover, the impact of these maladaptive schemas extends beyond the immediate activation by external cues. Appraising the negative event as central to identity could contribute to these maladaptive self-referential schemas: If memories associated with these schemas are easily accessible in autobiographical memory, they can exert a continuous influence even in the absence of explicit external triggers. This persistent influence underscores the enduring nature of maladaptive self-referential schemas and their role in perpetuating and intensifying depressive symptoms over time (Beck, Citation1967, Citation2002).
Empirical findings
As discussed, SAD and MDD have been linked to specific onset events (Kendler et al., Citation1999; Kessler, Citation1997; Magee, Citation1999; McCutcheon et al., Citation2009; Rapee & Spence, Citation2004). Moreover, empirical research has found that both disorders are related to overlapping cognitive and emotion regulation variables which are linked to event centrality, including trait anxiety, rumination and worry, intrusions and avoidance, and posttraumatic cognitions (Ehring et al., Citation2006; Gehrt et al., Citation2018; Muris et al., Citation2005; Vermeulen et al., Citation2019). A small positive association between event centrality and SAD has been reported before (Matos et al., Citation2013). Also, event centrality levels decreased throughout the treatment of social anxiety (O’Toole et al., Citation2018), hinting towards a positive association between event centrality and SAD symptoms. Research on the link between event centrality and depression has, however, provided mixed results. Significant positive correlations were found between event centrality and the amount and severity of depression symptoms (Berntsen & Rubin, Citation2006, Citation2007; Boals, Citation2010, Citation2014; Boelen, Citation2009, Citation2012a; Robinaugh & McNally, Citation2011; Vermeulen et al., Citation2020), over and above anxiety, avoidance, and neuroticism (Boelen, Citation2012a), and repetitive negative thinking (Allbaugh et al., Citation2016). However, other studies could not find a link between event centrality and currently depressed, recovered, and never-depressed groups (Newby & Moulds, Citation2011). In addition, the link between event centrality and depression was not consistently found among different cultures in large cross-cultural studies in community samples (Zaragoza Scherman et al., Citation2015). It has been suggested that depression is affected by the lack of centrality of positive events instead of the increased centrality of negative events (Janssen et al., Citation2015). Moreover, event centrality might have an indirect relation with depression mediated by PTSD symptoms (Vermeulen et al., Citation2020), negative cognitions, rumination, and avoidance (Boelen, Citation2012b). This suggests a positive relationship between event centrality and depression; however, this link might be mediated by several maladaptive emotion regulation variables.
Current study
Most of the above-mentioned studies have been conducted in student or community samples; it is unclear how the relation between event centrality and symptoms manifests in clinical samples. Therefore, the first aim of this study was to explore the association between event centrality and social anxiety/depressive symptoms in a SAD patient sample and an MDD patient sample, where we expected significant positive relations between event centrality and the disorder-specific symptoms. Our second aim was to explore potential mediators (i.e., trait anxiety, rumination, worry, intrusions and avoidance, and posttraumatic cognitions) of this relationship within both groups. Based on the results from PTSD samples, we expected each variable to mediate the relationship between event centrality and disorder-specific symptoms individually.
Method
Participants and design
The current study employed a cross-sectional design, collecting data from two patient groups: a SAD patient group and an MDD patient group. A total of 59 participants were recruited. The sample size was based on resource limitations (number of patients willing to participate within the timeframe allocated by the participating mental healthcare facilities for this study). Patients descriptives of both groups can be found in Table A1. The SAD group consisted of 38 patients (23 females; 61%) from an outpatient centre for specialised mental healthcare in the Netherlands. Participants had a current primary diagnosis of SAD, based on DSM-5 criteria (American Psychiatric Association, Citation2013), as ascertained by a trained psychologist or psychiatrist (or trainee under supervision) from the participating mental healthcare centre as part of their regular intake procedure. Patients with comorbid PTSD, substance abuse, or psychosis were excluded.
The MDD group consisted of 21 patients (12 females; 57%) from a university hospital in Belgium (n = 19) and an outpatient centre for specialised mental healthcare in the Netherlands (n = 2). All participants had a current primary diagnosis of MDD based on DSM-IV-TR criteria (American Psychiatric Association, Citation2000), as ascertained by a trained psychologist or psychiatrist (or trainee under supervision) participating mental healthcare centre as part of their regular intake procedure. Patients with comorbid bipolar disorder, PTSD, SAD, substance use, or psychosis were excluded.
Measures
Episode duration and perceived onset event. Participants were asked for the duration of their current episode of SAD or MDD and were asked whether they had experienced an adverse event which was in their opinion related to the onset of their disorder, and if so, to write down the memory of this event.
Centrality of Event Scale (CES; Berntsen & Rubin, Citation2006; Vermeulen et al., Citation2020). The abbreviated 7-item version of the Dutch CES (Vermeulen et al., Citation2020) was used to measure the centrality of the perceived onset event. The questionnaire consists of seven self-report items, with Likert scale answer options ranging from 1 (totally disagree) to 5 (totally agree). Total scores on the CES range between 5 and 35. The internal consistency in the current samples was α = .79 in the SAD group and α = .84 in the MDD group. Because the abbreviated version of the Dutch CES has shown a similar level of validity as the 20-item version (Vermeulen et al., Citation2023) and need for parsimony, we chose to administer the abbreviated (and thus shorter) 7-item version of the CES.
Beck Depression Inventory-II-NL (BDI-II-NL; Beck et al., Citation1996, Citation2002). The Dutch translation of the BDI-II-NL (Beck et al., Citation2002) was used to measure the severity of depressive symptoms. The questionnaire consists of 21 self-report items (score 0–3). Total scores on the BDI-II-NL range from 0 to 63. The internal consistency in our samples was for the SAD group: α = .89; and MDD group α = .82.
Liebowitz Social Anxiety Scale (LSAS; Liebowitz, Citation1987; Van Vliet, Citation1999). The Dutch translation of the LSAS (Van Vliet, Citation1999) was used to measure symptoms of social anxiety. The questionnaire consists of 24 items, 11 items on social situations, and 13 items on performance anxiety. All items are rated twice: once on the level of anxiety, ranging from none (0) to severe (3), and once on the level of avoidance, ranging from never (0) to usually (3). Total score range between 0 and 144. The internal consistency in the current SAD sample was α = .95 (not assessed in the MDD sample).
Impact of Event Scale (IES; Brom & Kleber, Citation1985; Horowitz et al., Citation1979). The Dutch version of the IES (Brom & Kleber, Citation1985) was used to measure symptoms of intrusions and avoidance related to the memory of the perceived onset event. The questionnaire consists of 15 self-report items, 8 items in the intrusion subscale, and 7 in the avoidance subscale. Items are rated on a 5-point Likert scale, ranging from 0 (not at all) to 4 (extremely). Total score range between 0–28 (Intrusions; 7 items) and 0–32 (Avoidance; 8 items). The internal consistency in the current samples was SAD group: intrusions α = .91; avoidance α = .89; and the MDD group: intrusions α = .88; avoidance α = .56.
Posttraumatic Cognitions Inventory (PTCI; Foa et al., Citation1999; van Emmerik et al., Citation2006). The Dutch version of the PTCI (van Emmerik et al., Citation2006) was used to assess posttraumatic cognitions. Participants rate 33 self-report items on a 7-point Likert scale ranging from 1 (totally disagree) to 7 (totally agree). Total score ranges between 33 and 231. The internal consistency in this sample was SAD group: α = .95; and MDD group α = .91.
State-Trait Anxiety Inventory (STAI-T; Spielberger et al., Citation1970; Van der Ploeg, Citation1980). The Dutch version of the STAI-T (Van der Ploeg, Citation1980) was used to measure trait anxiety. The questionnaire consists of 20 statements, scored on a 4-point Likert scale, ranging from 1 (almost never) to 4 (almost always). Participants indicate how they feel in general regarding each statement. Total score range between 20 and 80. The internal consistency in this sample was SAD group: α = .87; and MDD group α = .86.
Penn State Worry Questionnaire (PSWQ; Meyer et al., Citation1990; Van Rijsoort et al., Citation1999). The Dutch version of the PSWQ (Van Rijsoort et al., Citation1999) was used to measure pathological worry. The questionnaire consists of 16 self-report items scored on a 5-point Likert scale, ranging from 1 (not at all) to 5 (very). Total score range between 16 and 80. The internal consistency in this sample was SAD group: α = .85; and MDD group α = .79.
Ruminative Response Scale (RRS; Raes et al., Citation2009; Raes & Hermans, Citation2007; Treynor et al., Citation2003). The Dutch version of the RRS (Raes & Hermans, Citation2007) was used to measure trait rumination. The questionnaire consists of 22 self-report items scored on a 4-point Likert scale, ranging from 1 (almost never) to 4 (almost always). The total score range between 22 and 88. The internal consistency in this sample was SAD group: α = .90; and MDD group α = .85.
Procedure
Approval for this study was obtained from the Social and Societal Ethics Committee of the KU Leuven (SMEC, reference number G-2014 12 128), the Ethics Committee of Antwerp University Hospital (registration number: B300201629846), and the Ethical Committee of the social science faculty of the Radboud University (ECSW, reference number: ECSW-2018-076).
After completing the informed consent form, participants completed in this order the demographic variables (age, sex, nationality, academic degree, and marital status), the disorder-specific questionnaire (SAD group: LSAS; MDD group: BDI-II-NL), a question about episode duration and the perceived onset event, CES, IES, PTCI, BDI-II-NL (added in SAD group), STAI-T, PSWQ, and the RRS. The questionnaires were completed individually (without the help of the therapist), using paper and pencil.
The SAD group completed the questionnaires as part of their intake process, i.e., before the start of treatment. In the MDD sample, the questionnaires were distributed to patients who were currently in treatment. Patients could choose when and where to complete the questionnaires and returned the questionnaires in a closed envelope to their therapist, who then delivered the anonymous questionnaires to the researcher.
Statistical analysis
All analyses were conducted using R studio. Missingness in the data was handled using multiple imputations. Data on all missing cases were computed using the predictive mean matching approach. The multiple imputation process was carried out using the MICE package (v3.5.0) in R (Van Buuren & Groothuis-Oudshoorn, Citation2011) to impute 100 datasets.
Given the relatively small sample size, Bayesian analyses with weakly informative priors for obtaining reliable results were conducted to answer our research questions (McNeish, Citation2016). Correlational analyses were conducted within patient groups using the Bayesian First Aid (v0.1) package in R (Bååth, Citation2014), which uses wide, uninformative priors. Correlation coefficients with 95% highest-density intervals (HDI) are reported (Kruschke, Citation2018). To reject the null value of a parameter, the results need to express that the null value excludes the posterior 95% HDI. Thus, we considered a correlation “significant” when the 95% HDI interval did not include zero. The total iterations for the correlations were set at 20,000.
Mediation analyses were conducted. Within each patient group, mediation models were tested with CES as an independent variable, the disorder-specific symptoms (LSAS or BDI-II) as a dependent variable, and IES (intrusions and avoidance), PTCI, RRS, PSWQ, STAIT, and BDI-II-NL (only SAD group) as potential mediators. Because of potential power issues, the depression symptom analysis was additionally conducted in the total (SAD + MDD) sample. The priors for the intercept, the coefficients, and sigma (sd*sd) were set to t-distribution (with df = 3) to penalise the estimates for a small sample size. Total iterations for the mediation analysis were set to 5000. The significance of indirect effects was evaluated by constructing 95% HDI intervals around them. The indirect effect was interpreted as credible if the 95% HDI’s did not include zero. Completely standardised indirect effects were calculated (Preacher & Kelley, Citation2011), as these effects can be used to compare the different effect sizes across populations or different metrics in populations (Cheung, Citation2009). The mediation models were fitted using the brms package (v2.9.0) in R (Bürkner, Citation2017). Model components (e.g., coefficients, intercepts, indirect effects) are interpreted as they typically are in mediation models. As typical for Bayesian analysis, no adjustment for multiple testing was made (Gelman et al., Citation2012). Coefficients of the indirect effects were reported by a*b. We report how we determined our sample size, all data exclusions (if any), all manipulations, and all measures in the study. Data, materials, and analysis code for this study are available by e-mailing the corresponding author.
Perceived onset events were scored ad hoc (as suggested by one of our reviewers) on PTSD criterion A (American Psychiatric Association, Citation2013, p. 271), general life events (e.g., divorce, surgery, moving), or social/relational events (e.g., social conflict, bullying) by two independent raters. It was possible for descriptions to be scored in multiple categories as some contained multiple events. Interrater reliability was calculated with Cohen’s Kappa. Disagreements (n = 8) were resolved through discussion. Differences in reporting each category of events between the SAD and MDD groups were tested with Chi-Square tests.
Results
Descriptive statistics
Means and SDs of the descriptive variables per patient group and possible significant differences between the two groups can be found in Table A1. A significant age difference between the two patient groups was found. Regarding the perceived onset event, 26 patients (68.4%) in the SAD group and 18 patients (85.7%) in de MDD group indicated that they had experienced an adverse event which was in their perception related to the onset of their disorder. Differences in participants’ descriptives between those who reported a perceived onset event and those who did not can be found in Table A2, showing no significant difference between these two groups. Missingness analyses showed that 37 (62.7%) participants completed all items across measures. Overall, 8% of missingness was registered.
Correlations
Correlations within the patient groups can be found in Table A3 (the top half [above the diagonal] shows the correlations within the SAD group, the bottom half [under the diagonal] shows the correlations within the MDD group). All correlations were positive, ranging between .10 and .79 in the SAD group and between .29 and .74 in the MDD group. In the SAD group, the results showed that CES scores were significantly correlated, in descending order from large to moderate, with IES-avoidance, IES-intrusions, and PTCI (posttraumatic cognitions) only.
In the MDD group, the CES was significantly and positively correlated, in descending order, from large to moderate, with PTCI (posttraumatic cognitions), IES-intrusions, RRS (rumination), STAI-T (trait anxiety), IES-avoidance, and BDI-II (depressive symptoms), but not to the PSWQ (worry).
Mediation analyses
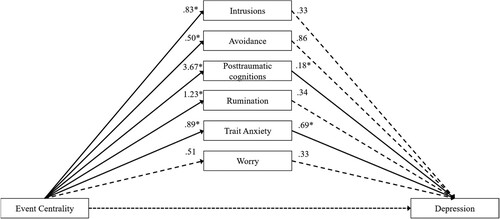
Results of the within-group mediation analyses can be found in and and Tables A4 and A5. In the within-group mediation analyses of the SAD group (Table A4 and ), the results showed that none of the variables (PTCI, IES-intrusions, IES-avoidance, RRS, STAI-T, PSWQ, and BDI-II) mediated the relation between the CES and LSAS; neither significant direct effect nor significant indirect effects could be found. In the MDD group ( and Table A5), a significant direct effect was found between the CES and BDI-II-NL with PSWQ as a mediating variable, indicating no effect of worry as a mediator. Significant indirect effects were found in the analysis with PTCI and STAI-T as mediators, indicating the relation between event centrality and depressive symptoms was mediated by posttraumatic cognitions and trait anxiety.
Figure 1. Mediation analyses of the effect of event centrality on social anxiety symptoms through the different variables in the SAD sample.
Note: None of the variables significantly mediated the link between event centrality and social anxiety symptoms. Dotted lines represent non-significant betas. Total results of the Bayesian mediation analysis can be found in Table A4.
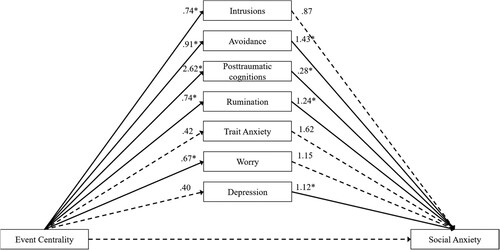
Figure 2. Mediation analyses of the effect of event centrality on depressive symptoms through the different variables in the MDD sample.
Note: Posttraumatic cognitions and Trait Anxiety mediated the link between event centrality and depressive symptoms. Dotted lines represent non-significant betas. Full results of the Bayesian mediation analysis can be found in Table A5.
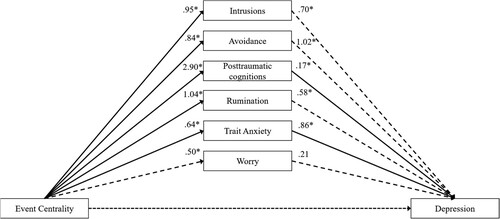
Based on the correlations reported in Table A3, additional significant mediation effects were expected, indicating a possible statistical power issue. Therefore, both patient groups were combined to increase the sample size and, thereby, power. Results can be found in and Table A6. A significant direct effect between the CES and BDI-II-NL was again found for PSWQ as a mediator, again indicating that worry did not mediate the relation between event centrality and depressive symptoms. Significant indirect effects were found in all other analyses with as mediator; IES-intrusions, IES-avoidance, PTCI, RRS, and STAI-T. This indicates that the relation between the event centrality and depressive symptoms was mediated by intrusions, avoidance, posttraumatic cognitions, rumination, and trait anxiety.
Figure 3. Mediation analyses of the effect of event centrality on depressive symptoms through the different variables in the combined sample.
Note: All variables, except worry, mediated the relation between event centrality and depressive symptoms. Dotted lines represent non-significant betas. Full results of the Bayesian mediation analysis can be found in Table A6.
Ad hoc analyses on perceived onset memory content
Interrater reliability of the scored events was high, Cohen’s κ = 0.84. The MDD group reported significantly more PTSD A criterion events than the SAD group, χ2(1) = 7.52, p = .006, whereas the groups did not differ in the number of reported general events, χ2(1) = 2.68, p = .10. Finally, significantly more social/relational events were reported in the SAD group than the MDD group χ2(1) = 4.39, p = .036.
Discussion
Our aim was to study the relation between event centrality and depressive and social anxiety symptoms, and their mediators (i.e., intrusions, avoidance, posttraumatic cognitions, rumination, trait anxiety, and worry) in two clinical groups of patients diagnosed with SAD or MDD.
Event centrality in SAD
Although event centrality was moderate to strong and positively correlated with intrusions, avoidance, and posttraumatic cognitions within the SAD group, contrasting to our hypothesis, event centrality scores were not correlated with social anxiety symptoms. However, the size of the correlations was similar to those reported by Gehrt et al. (Citation2018), where they reached significance, probably due to a larger sample size. In addition, a substantial portion (46%) of individuals in the SAD group did not report a perceived onset event, for which their most negative life event might (which they had in mind while completing the CES) might not have been related to their disorder-specific symptoms. The lack of a significant correlation between event centrality and social anxiety symptoms might also be explained by certain characteristics of SAD. Event centrality represents cognitions and appraisals about a specific (negative) event (Berntsen & Rubin, Citation2006), whereas SAD is characterised by maladaptive cognitions about the self in more general terms (Hofmann, Citation2007), such as low self-esteem (Rapee & Heimberg, Citation1997). SAD typically develops more gradually during adolescence and might be linked to more general schemas related to less salient but common occurrences (e.g., implicit messages that the child is not wanted, Young, Citation1999). Event centrality appraisals such as “this event changed my life” (Berntsen & Rubin, Citation2006) might not be of specific impact on the development and maintenance of SAD as it is in PTSD. Indeed, research has shown that the development of SAD is more often preceded by events of more subtle emotional messages of, for example, shame (Magee, Citation1999; Rapee & Spence, Citation2004), whereas MDD and PTSD are more often linked with intense emotional, physical, and/or sexual (childhood) abuse (Maniglio, Citation2010; Wiersma et al., Citation2009). This aligns with the results of our content analyses of the reported perceived onset events, where the MDD group reported more traumatic events (PTSD criterion A) and the SAD group reported more non-traumatic social/relational events (e.g., social conflict, bullying) as perceived onset events of their symptoms.
Event centrality in MDD
Within the MDD group, event centrality and depressive symptoms were moderately and positively correlated, aligning with our expectations. Event centrality was significantly correlated with all variables except worry. Posttraumatic cognitions and trait anxiety mediated the relation between event centrality and depression in the MDD sample, consistent with the conceptualisation of MDD as a posttrauma disorder (Radell et al., Citation2020) with a high comorbidity with PTSD (Angelakis & Nixon, Citation2015). A remarkable result was the surprisingly low internal consistency of avoidance symptoms as measured with the IES in the MDD group (α = .56). As we are unaware of other studies that reported similar results, we expect this problem to be caused by the small sample size.
In the combined group mediation analysis, all variables except worry were significant mediators of the relationship between event centrality and depression symptoms, indicating preliminary evidence for a transdiagnostic link between event centrality and depressive symptoms. The absence of worry as a mediator indicates that event centrality is typically more focused on the past than the future, challenging the theoretical assumption of event centrality (Berntsen & Rubin, Citation2006) stating that central events form a cognitive reference point, and thereby influence the interpretation of both past experiences and future expectations. This highlights an avenue for future research to explore this aspect more comprehensively.
In sum, our findings confirm the results of earlier studies supporting a direct relation between event centrality and depressive symptoms (Allbaugh et al., Citation2016; Berntsen & Rubin, Citation2006, Citation2007; Boals, Citation2010, Citation2014; Boelen, Citation2009, Citation2012a, Citation2012b; Robinaugh & McNally, Citation2011; Vermeulen et al., Citation2020). Our findings also align with Beck’s cognitive model of depression (Beck, Citation1967), providing a nuanced understanding of how event centrality contributes to depressive symptomatology: The observed direct association between event centrality and depressive symptoms resonates with Beck’s conceptualisation that negative events serve as catalysts for the development of maladaptive self-referential schemas and dysfunctional attitudes.
The results of the mediation analysis are consistent with earlier research (Boelen, Citation2012b; Vermeulen et al., Citation2020), which demonstrated that the relationship between event centrality and depressive symptoms is mediated by PTSD symptoms, negative cognitions, and rumination. Furthermore, our mediation analysis provides concrete evidence that supports the cognitive processes delineated in Beck’s model (Beck, Citation1967, Citation2002). The presence of mediating variables, including PTSD symptoms, negative cognitions, and rumination, signifies a pathway through which event centrality influences depressive symptoms. This mediation pathway echoes Beck’s proposition that maladaptive self-referential schemas dynamically interact with perceptions of subsequent events, predisposing individuals to interpret new situations in a manner consistent with their negative attitudes. Generally, the impact of event centrality appears to be more pronounced in PTSD (Boals & Murrell, Citation2016; Gehrt et al., Citation2018) and MDD than in other disorders such as SAD (as observed in the current study).
Clinical implications
Our findings hold clinical implications. First, there are notable similarities in the correlations of event centrality between PTSD and MDD, and both disorders can develop following a traumatic experience (Angelakis & Nixon, Citation2015; Radell et al., Citation2020). This suggests that specific negative events may contribute to or trigger the onset of both PTSD and MDD, potentially through the mechanism of event centrality. In the case of PTSD, a clear (traumatic) onset event is even a requirement for diagnostic classification. One could argue that a similar criterion should be considered for MDD. However, establishing the causal role of any perceived onset event is highly challenging in MDD. Additionally, many MDD patients do not perceive a specific onset event for their episode. Therefore, we do not recommend including a central onset event in the classification criteria for MDD. Nevertheless, in a more comprehensive diagnostic interview, it might be valuable to inquire about perceived onset events and event centrality as this could guide treatment direction (e.g., identifying key negative cognitions). We did not find any specific evidence to support this approach for SAD, so we will not make these specific recommendations for SAD treatment.
Limitations
Several limitations have to be taken into account when interpreting the results of the current study. The main limitation of our study was the small sample size of the two groups suggesting that some existing correlations (Gehrt et al., Citation2018) might not have been detected in our study due to lack of statistical power (type-II error). Furthermore, there was a large difference in age range between the patient groups (i.e., SAD-Mage = 30.66; MDD-Mage = 49.48). These age ranges fit with the prevalence of these specific disorders thereby reflecting typical patient samples. However, age may have been a confounding factor in the combined group for data analysis. For example, age is a relevant factor in trauma-related psychopathology, where a younger age might be an increased vulnerability to PTSD (Kongshøj & Berntsen, Citation2022). Thus, if possible, future research should control for age range differences by matching groups on age. Moreover, 46% of patients in the SAD group did not report an event linked to the onset of their disorder. This makes it unclear what event they had in mind while answering the questionnaires. We suggest that future studies record a brief description of the specific memory which they had in mind while completing the questionnaires, in addition to requesting a description of their identified onset event. Furthermore, we did not include event centrality assessments for neutral events, positive events, or negative events not perceived as related to the onset of the disorder. Consequently, it is not feasible to determine whether the observed event centrality relations are exclusive to the perceived onset events or if they represent a more general bias towards event centrality bias within individual participants. Future research should include this and control for this possible bias. As a final limitation, the cross-sectional design of this study limits our ability to draw causal inferences from the mediation analyses. Future research should employ a longitudinal design to examine the potential causal effects and the temporal ordering of the hypothesised mediation processes.
Conclusion
In sum, we found that event centrality and social anxiety symptoms were not significantly correlated. A positive strong correlation was found between event centrality and depressive symptoms in the sample of MDD patients. Posttraumatic cognitions and trait anxiety mediated the role between event centrality and depressive symptoms in this group. In the combined transdiagnostic sample, we found that intrusions, avoidance, posttraumatic cognitions, rumination, and trait anxiety mediated the relation between event centrality and depressive symptoms. Our results indicate that event centrality may play a larger role in MDD (or trauma-related disorders such as PTSD and MDD) than SAD. When treating MDD (but not SAD), it might be important to ask whether the client associates the onset of their symptoms with a particular event, and if so, target cognitions of event centrality in treatment. The supported mediators (i.e., intrusions, avoidance, posttraumatic cognitions, rumination, and trait anxiety) might be important for future exploration in understanding the persistence of depression.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Animal rights: This article does not contain any studies with animals performed by any of the authors.
Acknowledgements
We thank all participants for engaging in this research, and Agnes van Minnen, Rianne de Kleine, Jan Spijker, Janna Vrijssen, and all research assistants and interns for the recruitment and admission of patients and data collection.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data, materials, and analysis code that support the findings of this study are available from the corresponding author ([email protected]) upon reasonable request.
Additional information
Funding
References
- Allbaugh, L. J., O’Dougherty Wright, M., & Folger, S. F. (2016). The role of repetitive thought in determining posttraumatic growth and distress following interpersonal trauma. Anxiety, Stress, & Coping, 29(1), 21–37. https://doi.org/10.1080/10615806.2015.1015422
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.).
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596.744053
- Angelakis, S., & Nixon, R. D. V. (2015). The comorbidity of PTSD and MDD: Implications for clinical practice and future research. Behaviour Change, 32(1), 1–25. https://doi.org/10.1017/bec.2014.26
- Bååth, R. (2014). Bayesian first aid: A package that implements Bayesian alternatives to the classical *.test functions in R. UseR! 2014 – The International R User Conference.
- Beck, A. T. (1967). Depression: Clinical, experimental, and theoretical aspects. Harper & Row.
- Beck, A. T. (2002). Cognitive models of depression. In R. L. Leahy & E. T. Dowd (Eds.), Clinical advances in cognitive psychotherapy: Theory and application (Vol. 1, pp. 29–61). Springer Publishing Company, Inc.
- Beck, A. T. (2008). The evolution of the cognitive model of depression and its neurobiological correlates. American Journal of Psychiatry, 165(8), 969–977. https://doi.org/10.1176/appi.ajp.2008.08050721
- Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the Beck depression inventory-II. Psychological Corporation. https://doi.org/10.1037/t00742-000
- Beck, A. T., Steer, R. A., Brown, G. K., & Van Der Does, A. J. W. (2002). BDI-II-NL Handleiding [BDI-II-Dutch manual]. Psychological Corporation.
- Berntsen, D., & Rubin, D. C. (2006). The centrality of event scale: A measure of integrating a trauma into one’s identity and its relation to post-traumatic stress disorder symptoms. Behaviour Research and Therapy, 44(2), 219–231. https://doi.org/10.1016/j.brat.2005.01.009
- Berntsen, D., & Rubin, D. C. (2007). When a trauma becomes a key to identity: Enhanced integration of trauma memories predicts posttraumatic stress disorder symptoms. Applied Cognitive Psychology, 21(4), 417–431. https://doi.org/10.1002/acp.1290
- Boals, A. (2010). Events that have become central to identity: Gender differences in the centrality of events scale for positive and negative events. Applied Cognitive Psychology, 24(1), 107–121. https://doi.org/10.1002/acp.1548
- Boals, A. (2014). Using event centrality to predict depressive symptoms after a romantic conflict: A prospective design. Applied Cognitive Psychology, 28(2), 259–265. https://doi.org/10.1002/acp.2996
- Boals, A., & Murrell, A. R. (2016). I am > trauma: Experimentally reducing event centrality and PTSD symptoms in a clinical trial. Journal of Loss and Trauma, 21(6), 471–483. https://doi.org/10.1080/15325024.2015.1117930
- Boelen, P. A. (2009). The centrality of a loss and its role in emotional problems among bereaved people. Behaviour Research and Therapy, 47(7), 616–622. https://doi.org/10.1016/j.brat.2009.03.009
- Boelen, P. A. (2012a). A prospective examination of the association between the centrality of a loss and post-loss psychopathology. Journal of Affective Disorders, 137(1–3), 117–124. https://doi.org/10.1016/j.jad.2011.12.004
- Boelen, P. A. (2012b). Variables mediating the linkage between loss centrality and postloss psychopathology. Journal of Nervous & Mental Disease, 200(9), 801–806. https://doi.org/10.1097/NMD.0b013e318266ba02
- Brom, D., & Kleber, R. J. (1985). De Schok Verwerkings Lijst [The Dutch version of the impact of event scale]. Nederlands Tijdschrift Voor Psychologie, 40(1), 164–168.
- Brown, A. D., Antonius, D., Kramer, M., Root, J. C., & Hirst, W. (2010). Trauma centrality and PTSD in veterans returning from Iraq and Afghanistan. Journal of Traumatic Stress, 23(4), 496–499. https://doi.org/10.1002/jts.20547
- Bürkner, P. C. (2017). Brms: An R package for Bayesian multilevel models using Stan. Journal of Statistical Software, 80(1), 1–28. https://doi.org/10.18637/jss.v080.i01
- Cheung, M. W. L. (2009). Comparison of methods for constructing confidence intervals of standardized indirect effects. Behavior Research Methods, 41(2), 425–438. https://doi.org/10.3758/BRM.41.2.425
- Clark, D. M., & Wells, A. (1995). A cognitive model of social anxiety. In R. G. Heimberg, M. R. Liebowitz, D. A. Hope, & F. R. Schneier (Eds.), Social phobia: Diagnosis, assessment and treatment (pp. 69–93). Guilford Press.
- De Venter, M., Van Den Eede, F., Pattyn, T., Wouters, K., Veltman, D. J., Penninx, B. W. J. H., & Sabbe, B. G. (2017). Impact of childhood trauma on course of panic disorder: Contribution of clinical and personality characteristics. Acta Psychiatrica Scandinavica, 135(6), 554–563. https://doi.org/10.1111/acps.12726
- Ehring, T., Ehlers, A., & Glucksman, E. (2006). Contribution of cognitive factors to the prediction of post-traumatic stress disorder, phobia and depression after motor vehicle accidents. Behaviour Research and Therapy, 44(12), 1699–1716. https://doi.org/10.1016/j.brat.2005.11.013
- Foa, E. B., Ehlers, A., Clark, D. M., Tolin, D. F., & Orsillo, S. M.. (1999). The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment, 11(3), 303–314. https://doi.org/10.1037/1040-3590.11.3.303
- Gehrt, T. B., Berntsen, D., Hoyle, R. H., & Rubin, D. C. (2018). Psychological and clinical correlates of the centrality of event scale: A systematic review. Clinical Psychology Review, 65(July), 57–80. https://doi.org/10.1016/j.cpr.2018.07.006
- Gelman, A., Hill, J., & Yajima, M. (2012). Why we (usually) don’t have to worry about multiple comparisons. Journal of Research on Educational Effectiveness, 5(2), 189–211. https://doi.org/10.1080/19345747.2011.618213
- Hofmann, S. G. (2007). Cognitive factors that maintain social anxiety disorder: A comprehensive model and its treatment implications. Cognitive Behaviour Therapy, 36(4), 193–209. https://doi.org/10.1080/16506070701421313
- Horowitz, M., Wilner, N., & Alvarez, W. (1979). Impact of event scale: A measure of subjective stress. Psychosomatic Medicine, 41(3), 209–218. https://doi.org/10.1097/00006842-197905000-00004
- Janssen, S. M. J., Hearne, T. L., & Takarangi, M. K. T. (2015). The relation between self-reported PTSD and depression symptoms and the psychological distance of positive and negative events. Journal of Behavior Therapy and Experimental Psychiatry, 48, 177–184. https://doi.org/10.1016/j.jbtep.2015.04.002
- Kendler, K. S., Karkowski, L. M., & Prescott, C. A. (1999). Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry, 156(June), 837–841. https://doi.org/10.1176/ajp.156.6.837
- Kessler, R. C. (1997). The effects of stressful life events on depression. Annual Review of Psychology, 48(1), 191–214. https://doi.org/10.1146/annurev.psych.48.1.191
- Kongshøj, I. L. L., & Berntsen, D. (2022). Is young age a risk factor for PTSD? Age differences in PTSD-symptoms after hurricane Florence. Traumatology, 29(2), 211–223. https://doi.org/10.1037/trm0000389
- Kruschke, J. K. (2018). Rejecting or accepting parameter values in Bayesian estimation. Advances in Methods and Practices in Psychological Science, 1(2), 270–280. https://doi.org/10.1177/2515245918771304
- Lancaster, S. L., Rodriguez, B. F., & Weston, R. (2011). Path analytic examination of a cognitive model of PTSD. Behaviour Research and Therapy, 49(3), 194–201. https://doi.org/10.1016/j.brat.2011.01.002
- Liebowitz, M. R.. (1987). Social phobia. Modern Problems of Pharmacopsychiatry, 22, 141–173. https://doi.org/10.1159/000414022
- Magee, W. J. (1999). Effects of negative life experiences on phobia onset. Social Psychiatry and Psychiatric Epidemiology, 34(7), 343–351. https://doi.org/10.1007/s001270050154
- Maniglio, R. (2010). Child sexual abuse in the etiology of depression: A systematic review of reviews. Depression and Anxiety, 27(7), 631–642. https://doi.org/10.1002/da.20687
- Matos, M., Pinto-Gouveia, J., & Gilbert, P. (2013). The effect of shame and shame memories on paranoid ideation and social anxiety. Clinical Psychology & Psychotherapy, 20(4), 334–349. https://doi.org/10.1002/cpp.1766
- McCutcheon, V. V., Heath, A. C., Nelson, E. C., Bucholz, K. K., Madden, P. A. F., & Martin, N. G. (2009). Accumulation of trauma over time and risk for depression in a twin sample. Psychological Medicine, 39(3), 431–441. https://doi.org/10.1017/S0033291708003759
- McNeish, D. (2016). On using Bayesian methods to address small sample problems. Structural Equation Modeling: A Multidisciplinary Journal, 23(5), 750–773. https://doi.org/10.1080/10705511.2016.1186549
- Meyer, T. J., Miller, M. L., Metzger, R. L., & Borkovec, T. D. (1990). Development and validation of the penn state worry questionnaire. Behaviour Research and Therapy, 28(6), 487–495. https://doi.org/10.1016/0005-7967(90)90135-6
- Muris, P., Roelofs, J., Rassin, E., Franken, I., & Mayer, B. (2005). Mediating effects of rumination and worry on the links between neuroticism, anxiety and depression. Personality and Individual Differences, 39(6), 1105–1111. https://doi.org/10.1016/j.paid.2005.04.005
- Newby, J. M., & Moulds, M. L. (2011). Intrusive memories of negative events in depression: Is the centrality of the event important? Journal of Behavior Therapy and Experimental Psychiatry, 42(3), 277–283. https://doi.org/10.1016/j.jbtep.2010.12.011
- O’Toole, M. S., Watson, L. A., Rosenberg, N. K., & Berntsen, D. (2018). Changes in perceived centrality of anxious events following cognitive behavioral therapy for social anxiety disorder and panic disorder. Journal of Behavior Therapy and Experimental Psychiatry, 59(March 2017), 150–156. https://doi.org/10.1016/j.jbtep.2018.01.007
- Preacher, K. J., & Kelley, K. (2011). Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods, 16(2), 93–115. https://doi.org/10.1037/a0022658
- Radell, M. L., Hamza, E. A., & Moustafa, A. A. (2020). Depression in post-traumatic stress disorder. Reviews in the Neurosciences, 31(7), 703–722. https://doi.org/10.1515/revneuro-2020-0006
- Raes, F., & Hermans, D. (2007). The revised version of the Dutch Ruminative Response Scale [Unpublished instrument].
- Raes, F., Schoofs, H., Hoes, D., Hermans, D., Van Den Eede, F., & Franck, E. (2009). “Reflection” en “brooding” als subtypes van rumineren: Een herziening van de ruminative response scale. Gedragstherapie, 42(3/4), 205–214.
- Rapee, R. M., & Heimberg, R. G. (1997). A cognitive-behavioral model of anxiety in social phobia. Behaviour Research and Therapy, 35(8), 741–756. https://doi.org/10.1016/S0005-7967(97)00022-3
- Rapee, R. M., & Spence, S. H. (2004). The etiology of social phobia: Empirical evidence and an initial model. Clinical Psychology Review, 24(7), 737–767. https://doi.org/10.1016/j.cpr.2004.06.004
- Robinaugh, D. J., & McNally, R. J. (2011). Trauma centrality and PTSD symptom severity in adult survivors of childhood sexual abuse. Journal of Traumatic Stress, 24(4), 483–486. https://doi.org/10.1002/jts.20656
- Spielberger, C. D., Gorsuch, R., & Lushene, R. E. (1970). Manual for the State-Trait Anxiety Inventory. Palo Alto.
- Treynor, W., Gonzalez, R., & Nolen-Hoeksema, S. (2003). Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research, 27(3), 247–259. https://doi.org/10.1023/A:1023910315561
- Van Buuren, S., & Groothuis-Oudshoorn, K. (2011). Mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45(3), 1–67. https://doi.org/10.18637/jss.v045.i03
- Van der Ploeg, H. M. (1980). Validity of the Zelf-Beoordelings-Vragenlijst (A Dutch version of the Spielberger state-trait anxiety inventory). Nederlands Tijdschrift Voor de Psychologie En Haar Grensgebieden, 35(4), 243–249. http://psycnet.apa.org/psycinfo/1981-22544-001
- van Emmerik, A. A. P., Schoorl, M., Emmelkamp, P. M. G., & Kamphuis, J. H. (2006). Psychometric evaluation of the Dutch version of the posttraumatic cognitions inventory (PTCI). Behaviour Research and Therapy, 44(7), 1053–1065. https://doi.org/10.1016/j.brat.2005.07.002
- Van Rijsoort, S., Emmelkamp, P., & Vervaeke, G. (1999). The Penn State worry questionnaire and the worry domains questionnaire: Structure, reliability and validity. Clinical Psychology & Psychotherapy, 6(4), 297–307. https://doi.org/10.1002/(SICI)1099-0879(199910)6:4<297::AID-CPP206>3.0.CO;2-E
- Van Vliet, I. M. (1999). Dutch translation of the Liebowitz Social Anxiety Scale [Unpublished work].
- Vermeulen, M., Brown, A. D., Raes, F., & Krans, J. (2019). Decreasing event centrality in undergraduates using cognitive bias modification of appraisals. Cognitive Therapy and Research, 43(1), 214–225. https://doi.org/10.1007/s10608-018-9936-3
- Vermeulen, M., Smits, D., Boelen, P. A., Claes, L., Raes, F., & Krans, J. (2020). The Dutch version of the centrality of event scale (CES): Associations with negative life events, posttraumatic stress, and depression symptoms in a student population. European Journal of Psychological Assessment, 36(2), 361–371. https://doi.org/10.1027/1015-5759/a000517
- Vermeulen, M., Smits, D., Claes, L., Gandhi, A., Raes, F., & Krans, J. (2023). The Dutch 20 item centrality of event scale: Factor structure, psychometric properties, and prospective value. European Journal of Psychological Assessment, 39(3), 211–221. https://doi.org/10.1027/1015-5759/a000704
- Wiersma, J. E., Hovens, J. G. F. M., Van Oppen, P., Giltay, E. J., Van Schaik, D. J. F., Beekman, A. T. F., & Penninx, B. W. J. H. (2009). The importance of childhood trauma and childhood life events for chronicity of depression in adults. The Journal of Clinical Psychiatry, 70(7), 983–989. https://doi.org/10.4088/JCP.08m04521
- Young, J. E. (1999). Cognitive therapy for personality disorders: A schema-focused approach (3rd ed.). Professional Resource Press/Professional Resource Exchange.
- Zaragoza Scherman, A., Salgado, S., Shao, Z., & Berntsen, D. (2015). Event centrality of positive and negative autobiographical memories to identity and life story across cultures. Memory, 23(8), 1152–1171. https://doi.org/10.1080/09658211.2014.962997
Appendix
Table A1. Means and standard deviations of all variables in the two patient groups and differences between the two groups.
Table A2. Participant’s descriptives and between-group differences of participants who did or not report an onset event.
Table A3. Correlations between all variables within the two patient groups.
Table A4. Within-group mediation analysis for the relation between event centrality and SAD.
Table A5. Within-group mediation analysis for the relation between event centrality and MDD.
Table A6. Combined sample mediation analysis for the relation between event centrality (CES) and MDD.

