Abstract
Background
The COVID-19 pandemic highlighted the necessity of equipping health professionals with knowledge and skills to effectively use digital technology for healthcare delivery. However, questions persist about the best approach to effectively educate future health professionals for this. A workshop at the 15th Nursing Informatics International Congress explored this issue.
Objective
To report findings from an international participatory workshop exploring pre-registration informatics implementation experiences.
Methods
A virtual workshop was held using whole and small group interactive methods aiming to 1) showcase international examples of incorporating health informatics into pre-registration education; 2) highlight essential elements and considerations for integrating health informatics into curricula; 3) identify integration models of health informatics; 4) identify core learning objectives, resources, and faculty capabilities for teaching informatics; and 5) propose curriculum evaluation strategies. The facilitators’ recorded data and written notes were content analysed.
Results
Fourteen participants represented seven countries and a range of educational experiences. Four themes emerged: 1) Design: scaffolding digital health and technology capabilities; 2) Development: interprofessional experience of and engagement with digital health technology capabilities; 3) implementation strategies; and 4) Evaluation: multifaceted, multi-stakeholder evaluation of curricula. These themes were used to propose an implementation framework.
Discussion
Workshop findings emphasise global challenges in integrating health informatics into curricula. While course development approaches may appear linear, the learner-centred implementation framework based on workshop findings, advocates for a more cyclical approach. Iterative evaluation involving stakeholders, such as health services, will ensure that health professional education is progressive and innovative.
Conclusions
The proposed implementation framework serves as a roadmap for successful health informatics implementation into health professional curricula. Prioritising engagement with health services and digital health industry is essential to ensure the relevance of implemented informatics curricula for the future workforce, acknowledging the variability in placement experiences and their influence on informatics exposure, experience, and learning.
Impact statement
Workshop insights shaped a learner-focused health informatics implementation framework via academic-health services partnerships, essential for a digitally enabled healthcare workforce.
Impact paragraph
Several digital health and informatics frameworks have been published, each detailing essential competencies for pre-registration healthcare students. While these frameworks guide educators on what to implement, how to implement health informatics content remains challenging across healthcare disciplines. Insights from an international participatory workshop at the 15th Nursing Informatics International Congress resulted in experts sharing their implementation journeys, shedding light on processes needed to successfully integrate health informatics into pre-registration education. Four key themes emerged: Design, Development, Implementation, and Evaluation, culminating in an implementation framework. This framework emphasises a learner-centred, iterative approach, stressing the importance of academic-health services partnerships as part of the roadmap for successful integration, ensuring the relevance of informatics curricula for a digitally enabled healthcare workforce.
Plain language statement
Several guides on digital health and informatics knowledge and skills for healthcare students have been published. Though helpful, putting these into practice across healthcare fields is challenging. Insights from a global workshop revealed experts’ experiences in integrating informatics into student education, resulting in a framework that prioritises learner-centred design and health services collaboration to ensure students are ready for modern healthcare.
1. Introduction
Increased global adoption of digital health technology necessitates an urgent assessment of professional digital literacy and capability to ensure that health profession students have a strong level of these abilities when they enter the workforce (Australian Nursing and Midwifery Federation (ANMF), Citation2015; Brunner et al., Citation2018; Canadian Association of Schools of Nursing, Citation2015; Edirippulige et al., Citation2018a; Honey et al., Citation2018; Hubner et al., Citation2018; Procter, Citation2017; Royal College of Nursing, Citation2018). While students enter the classroom with positive attitudes to technology, they lack confidence in their digital literacy for effective learning (Lokmic-Tomkins et al., Citation2022; Wong et al., Citation2023). Nonetheless, students’ positive attitudes to technology and pre-existing digital literacy levels serve as foundations for educators to create health informatics curricula that improve students’ capabilities and workforce readiness to provide safe and efficient person-centred care in digitally driven healthcare environments (McBride et al., Citation2013).
Several digital health and informatics frameworks have been published, each describing essential competencies for pre-registration healthcare students (Honey et al., Citation2017; Honey et al., Citation2018; Hubner et al., Citation2018; Hubner et al., Citation2018; McBride et al., Citation2013; Nagle et al., Citation2014). While these frameworks can assist educators in considering changing their curricula, the issue of ‘how to implement’ health informatics content remains challenging for educators across healthcare disciplines. For example, in the United Kingdom, despite the General Medical Council's accreditation requirements, a survey of medical schools found that 17% of the 76% of respondents had little or no health informatics in their curricula (Walpole et al., Citation2017). A similar conclusion was reached for pharmacy schools in the United States (Clauson et al., Citation2018; Honey et al., Citation2020) and nursing schools in Canada (Nagle et al., Citation2020a, Citation2020b). Lack of resources, informatics expertise, and other structural issues confronting educators exacerbated the difficulty in meaningfully implementing health informatics content into curricula (Aungst & Patel, Citation2020; Edirippulige et al., Citation2018a; Lokmic-Tomkins et al., Citation2022, Citation2023; Nagle et al., Citation2020a, Citation2020b).
Health profession students also enter educational programmes with deeper societal awareness of the role of digital health highlighted by the COVID-19 pandemic (e.g. telehealth, e-prescriptions, mobile health), (Dagliati et al., Citation2021; Mantas, Citation2020). However, the distillation of realistic recommendations reflective of real-world clinical practice to assist educators in implementing digital health and informatics competencies within their curricula is urgently needed. This, combined with rising consumer engagement in healthcare activities (The Commonwealth Fund, Citation2016), increases the pressure on educators to ensure healthcare professionals are knowledgeable and proficient in using digital health technology innovations to support care. (Lombardo et al., Citation2021) While efforts have been made to address the gap in health informatics content within curricula, practical, globally informed guidance remains missing from the literature. For example, while the literature suggests what content should be included (Australian Nursing and Midwifery Federation (ANMF), Citation2015; Canadian Association of Schools of Nursing, Citation2015; Honey et al., Citation2018; Hubner et al., Citation2018; Procter, Citation2017; Honey et al., Citation2017; Egbert et al., Citation2019), rational discussions of health informatics implementation frameworks that an educator can leverage to support pedagogy are missing in the discourse. Furthermore, insights into faculty development mechanisms for educators in the field of health informatics have yet to be thoroughly discussed in the literature (Honey et al., Citation2020; Honey et al., Citation2021).
An international-level workshop was organised to identify a practical framework to help educators implement health informatics content into nursing entry to practice curricula and address implementation of informatics competencies in health professional education. A ‘Development of Curriculum Frameworks: Embedding Health Informatics into Entry-to-Practice Nursing Curriculum’ workshop was held during the 15th International Nursing Informatics Conference. This workshop aimed to (1) showcase international examples of integrating digital health and informatics into pre-registration nurse education; (2) highlight the essential elements and considerations for integrating digital health and informatics into the curricula; (3) identify potential models of integrating digital health and informatics into nursing curricula underpinned by a person-centred framework; and (4) identify core learning objectives, required resources and faculty capabilities for teaching digital health and informatics content.
2. Materials and methods
2.1. Workshop design and structure
The 15th International Nursing Informatics Conference hosted a virtual international workshop (hereafter referred to as the ‘workshop’) via a web-conferencing platform. This workshop utilised a design-based research framework (DBR) (Lindgren et al., Citation2020; The Design-Based Research Collective, Citation2003), providing a forum for robust discourse supporting the need to meet expected nurse education standards for health informatics while ensuring safety and quality care principles were addressed. The workshop was divided into two parts delivered over 150 min. Part one set the stage for the workshop, with expert panel presentations based on examples from international health informatics education approaches. Discussions centred on higher education requirements, curricula accreditation, competency frameworks, and the development of business plans. Part two included a brief presentation describing one nursing school's approach to integrating informatics into a preregistration curriculum. This was followed by small groups discussions structured around workshop goals, which were then summarised and shared with the entire group. Finally, participants were asked to rate the workshop via an online poll. The workshop's reporting adheres to SRQR guidelines for reporting qualitative research studies (Supplementary material) (O'Brien et al., Citation2014).
2.2. Ethics
Research ethics approval was granted by the La Trobe University Institutional Review Board (HREC21245).
2.3. Participants
All attendees of the 15th International Nursing Informatics Conference were eligible to participate.
2.4. Data collection
Voice-recorded data were gathered from three small group break-out room discussions. A group facilitator was assigned to take handwritten notes. Data were gathered from audience questions and comments on the web-conference platform's chat function. Each group discussed four topics: 1) What content should be included in entry-to-practice degrees when implementing health informatics? 2) Are there any current integration models that you know of, and do you support any model for this purpose? 3) Given that some faculties do not have many (if any) academic health informaticians, what supports are required to facilitate implementation? 4) How would you assess the use of health informatics in your curriculum?
2.5. Data analysis
Following verbatim transcription, thematic content analysis was used to analyse workshop recordings, facilitator notes, and audience comments. A qualitative content analysis approach (Lindgren et al., Citation2020) enabled a structured, pragmatic process to overcome potential researcher bias and meet credible data analysis rigour and validation requirements (Graneheim et al., Citation2017; Vaismoradi et al., Citation2016). Data coding and theme development entailed creating meaningful units within the content; this was achieved by establishing sub-categories and categories to explain the phenomena and presenting these as themes through an iterative and reflective process ().
Table 1. Example of content analysis coding and theme development demonstrating one example for each theme.
Four cycles of data analysis were performed. Initially, three reviewers examined the raw data, coding, and emerging categories (MP, LMcK, KR). The second cycle, conducted by MH and ZLT, examined the coded data and categories and consolidated common concepts into themes. The content analysis output from cycles 1 and 2 was then examined by a HA, resulting in further theme refinement. Finally, all reviewers collaborated to reach consensus on themes.
2.6. Workshop evaluation
After the workshop, participants rated the workshop via a short five-question poll (), process deemed consistent with the DBR framework (Creswell & Poth, Citation2018; The Design-Based Research Collective, Citation2003).
Table 2. Workshop evaluation.
3. Results
3.1. Participants and the workshop evaluation
The workshop had 25 attendees, including three workshop organisers from Australia, and five invited international health informatics nursing faculty experts from the United States (n = 2), Canada (n = 1), the United Kingdom (n = 1), and New Zealand (n = 1). Fourteen health informaticians from Australia (n = 7), New Zealand (n = 1), Finland (n = 1), Taiwan (n = 1), the United States (n = 2), Canada (n = 1), and the United Kingdom (n = 1) consented to be research participants. Participants represented higher education institutions ranging from novices to experts in health informatics capability.
3.2. Content analysis
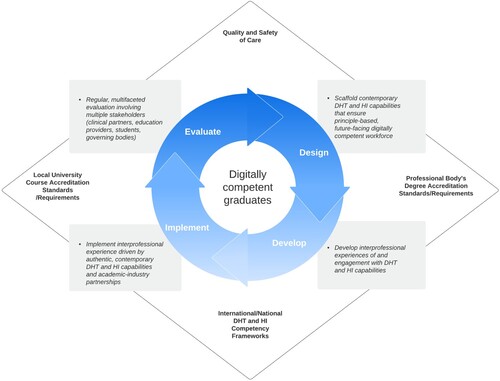
Four themes were identified: 1) Design: scaffolding contemporary digital health technology capabilities; 2) Development: interprofessional experience of and engagement with contemporary digital health technology capabilities; 3) Implementation strategies; and 4) Evaluation: a multifaceted, multi-stakeholder evaluation of the curricula ().
Figure 1. Summary of the workshop concepts and themes. HI = Health Informatics DH = Digital Health, IP = Interprofessional Practice.

3.2.1. Design: scaffolding contemporary digital health technology capabilities
Informatics education must align with the demands of contemporary digitised healthcare environments. Curricula development must provide scaffolded, interprofessional, standardised, essential digital health and informatics capabilities that address employers’ needs, are grounded in principles and are enduring. Course design must consider students’ existing digital and information literacy skills and their data analytics capabilities. While the initial focus may be on the most commonly used digital health technology, such as electronic medical records, telehealth and mobile health apps, innovative applications such as robotics, artificial intelligence, and machine learning must be considered as the curriculum scaffold evolves with future digital health technology developments. Participants emphasised the importance of ensuring students understood that decision support systems were intended to supplement, rather than replace, their critical thinking abilities. Authentic assessment based on realistic case studies were highly desired. There was agreement that a scaffolded pre-registration health informatics curriculum should lead to postgraduate studies and career paths for health informaticians. These pathways may encourage learners to specialise in more complex informatics capabilities, allowing them to advance healthcare professionals’ participation in developing future digital health solutions.
3.2.2. Development: interprofessional experience of and engagement with contemporary digital health technology capabilities
Curricula should include applied learning and reflect current point-of-care technology by implementing appropriate academic digital health technology solutions allowing students to develop their skills in simulated environments. Learning activities including authentic case studies, documentation, and problem-solving activities should be included to increase engagement with contemporary digital health technology. The focus should be on developing critical thinking and reasoning skills in collaboration with digital health technology. Clinical placements that help students consolidate their knowledge and skills in authentic interprofessional clinical settings can supplement this.
3.2.3. Implementation strategies
Implementation strategies for teaching methods recognise that academic staff must have knowledge and experience with modern digital health technologies to teach the subject confidently and competently. Participants proposed that closer relationships be developed with clinical placement providers and chief health informaticians at clinical placement sites for this to occur. One suggested goal of such collaborations is to establish mentoring relationships in which academic educators could mentor health informaticians to help them develop teaching skills. Equally, health informaticians could teach the academics about current digital health initiatives. Such interventions would necessitate the support of multiple stakeholders, including educators, clinical placement providers (hospitals, community care centres, and public health centres), and health informatics officers. Partnerships between education and healthcare organisations would be required. Participants expressed concern that current literature provided little guidance on infrastructure needed to implement health informatics in the curricula. They determined that the faculty needed assistance developing business plan proposals, assessing technological infrastructure requirements, and maintaining cybersecurity. Regarding curriculum development, participants determined that health informatics could be delivered as an integrated component of other content, a separate subject, or a separate course. Regardless, educators must ensure that career paths in health informatics are visible in order to advance health professional involvement in digital health technology development and implementation.
3.2.4. Evaluation: A multifaceted, iterative multi-stakeholder evaluation of the curricula
Curricula must evolve in tandem with digital health technologies. For this to happen, evaluation of health informatics curriculum must be a continuous, iterative process involving multiple stakeholders throughout the curriculum's lifespan. Participants proposed benchmarking health informatics curricula across institutions at the national, and potentially international levels be done regularly to ensure that the curriculum delivered is standardised. This would ensure content remained current, and students would be prepared to practice in a global environment. Furthermore, such benchmarking may aid in ensuring a shift away from teaching a single technology, such as electronic medical records or telehealth, toward broader and more futuristic implementation of digital health technologies, such as wearables, robotics, and artificial intelligence. Participants suggested a collaborative community of practices be established to foster knowledge transfer, including collaborative health services and digital health industry partnerships, and while these could be national, international partnerships were preferred.
3.3. Workshop evaluation
The outcome of the workshop evaluation is presented in .
4. Discussion
The workshop's findings revealed four themes: design, development, implementation strategies, and evaluation, all of which should be considered when incorporating health informatics and related digital health technologies into curricula. The researchers propose a framework using these four themes as pillars to support health informatics implementation in pre-registration nursing curricula (). While these elements are shown separately, they are interconnected, indicating that they all require a learner-centred approach to teaching and learning. This framework emphasises person-centred care, safety and quality in an interdisciplinary setting.
Figure 2. Implementation framework for integration of health informatics (HI) and digital health technology (DHT) competencies in health professional degrees.
Despite the existence of competency frameworks to inform academics about what should be taught in the health informatics curricula (Australian Nursing and Midwifery Federation (ANMF), Citation2015; Hubner et al., Citation2018; Honey et al., Citation2017), discussions revealed academic communities globally face significant implementation challenges. This study confirmed barriers to implementing digital health and informatics capabilities, such as a lack of executive management support, resources, knowledgeable and trained staff, and a general shortage of qualified health informaticians (Booth et al., Citation2021; Pontefract & Wilson, Citation2019; Lokmic-Tomkins et al., Citation2023). In contrast, the discussion offered enablers to support curriculum integration and capacity building, such as developing mentorship models and targeted professional development programmes to engage, advance, and connect faculty; specifically, establishing an international community of practice would be advantageous. Nagle et al. advocate for these types of enablers, suggesting adequately trained staff can engage, connect, and share experiences to support the advancement of informatics capabilities (Nagle et al., Citation2020a).
Each institution must decide which implementation model best meets its needs and resources. An individualised model can include anything from a single subject to a degree with blended content or specialised streams (Aungst & Patel, Citation2020; McBride et al., Citation2013; Pontefract & Wilson, Citation2019). Whatever model is used, educational institutions must form collaborative partnerships with clinical providers where clinical health informaticians collaborate with academic colleagues. Collaboration can ensure that current health informatics practice, which drive modern healthcare decisions, directly benefits the education programme. Mentorship may assist the clinical health informatician in developing transferable academic teaching skills. Practice-Academic collaborations are deemed necessary to keep individual curricula dynamic and reflective of rapidly changing digital health technologies. Importantly, such collaborations would assist educators in remaining acquainted with current content (Kinnunen et al., Citation2017) and align with the World Health 2020–2025 Global Strategy on Digital Health (World Health Organisation, Citation2021).
The proposed curriculum must carefully consider how to empower new health professionals to work with digital health technologies and redefine their professions in their presence. Scaffolding health informatics content in the presence of digital health technologies should support ongoing professional development and pathways in health informatics to promote a sense of professional identity, empowerment, and futurism (Aungst & Patel, Citation2020). Curriculum development should carefully consider how to empower health professionals to collaborate with digital health technologies to redefine their respective professions and generate new empirical knowledge and technology (Booth et al., Citation2021). Curricula development is critical because current curricula expect new graduates to practice safely in digitally driven healthcare environments without understanding how a lack of competencies negatively impacts healthcare delivery safety and quality of care (Aungst & Patel, Citation2020; Edirippulige et al., Citation2018b; Edirippulige et al., Citation2018c; McBride et al., Citation2013).
The importance of cutting-edge academic digital health technologies in developing student capability and preparation before entering clinical placement settings was emphasised. The short lifespan of digital health technologies as newer developments, approaches and applications supersede them complicates the situation, requiring educators to ensure that current digital health technology applications are available for teaching (Aungst & Patel, Citation2020). Due to the rapid development of digital health technologies, significant stressors are placed on decisions regarding which academic digital health technologies to pursue and incorporate into programmes, teaching methods to be used, and the excessive demand for ongoing updating of resources (Aungst & Patel, Citation2020). The proposed framework addresses the need for ongoing access to contemporary academic digital health technologies and point-of-care technology.
Rather than relying on technology to drive practice, emphasis was on developing critical thinking skills needed to practice in digitally augmented realities in collaboration with technology, such as data analytics. For example, when caring for someone with Type 2 diabetes, a discussion and care process should include digital health technologies to help students understand how the individual and their multidisciplinary team use data to make clinical decisions. Such case studies could be expanded in the context of data analytics to consider the total populations impacted by clinical interventions and what competencies are required to evaluate the quality of care. Use of digital health technologies influences how health professionals practice, engage, and connect with those in their care; therefore, rather than relying on technology to drive practice, greater emphasis should be placed on development of critical thinking skills and e-professionalism required to practice in digitally augmented realities, as well as collaboration with technology (Archibald & Barnard, Citation2018; Aungst & Patel, Citation2020). The proposed framework considers how digital health and informatics content and learning experiences can be integrated into existing clinical placement frameworks and learning activities.
Finally, the significance of embracing interprofessional curricula by bringing together various professions via a technology-mediated medium was emphasised (Aungst & Patel, Citation2020). This interprofessional requirement can be strengthened by implementing clinical placements focused on health informatics (Lokmic-Tomkins et al., Citation2021) and related digital health technologies. Interprofessional requirements may be strengthened by implementing clinical placements focused on health informatics and related digital health technologies. Such learning opportunities can capitalise on students’ positive attitudes toward health information technology (Lokmic-Tomkins et al., Citation2022) while allowing students to directly experience the value of health informatics in direct person-centred care (Brinkmann & Kvale, Citation2015 Lokmic-Tomkins et al., Citation2021).
4.1. Limitations
Although the number of people who participated in this virtual workshop and contributed to the data set was small, data saturation was achieved (Easterday et al., Citation2014). Participants came from various countries and cultural backgrounds; however, most were native-English speakers. The nature of the conference precluded interaction with participants from different professional backgrounds. While the discussions focused on nursing preregistration curricula, similar issues are likely to arise in all health professions (Aungst & Patel, Citation2020; Pontefract & Wilson, Citation2019). Participation in the workshop was voluntary, thus, participants’ self-selection bias is likely. Regardless of expertise level, a robust discussion revealed common challenges. Future research could replicate the workshop at a live event, ideally an international conference such as the event chosen for this study. Smaller groups with translators may attract more representatives from non-English speaking backgrounds, improving participant diversity. A critical area for future research is evaluating the proposed framework () and investigating its applicability to an international audience. Limitations regarding the DBR framework were addressed by consensus about the research questions, the guiding theoretical model and selecting research methods before running the workshop.
5. Conclusion
Embarking on implementing health informatics into curricula presents many challenges, including employing more academic educators with sufficient knowledge of health informatics, and systemic barriers such as the digital health technology implementation costs. The workshop outcomes highlight these issues while providing an implementation framework to guide others through the implementation process. Fundamentally, without incorporating health informatics and digital health technologies competencies into curriculum, the safety and quality of healthcare are jeopardised. Feedback from those who use the proposed framework will aid in its future improvements. The most critical implementation facilitator may be formation of a global community of practice and formalised academic-health services and digital health industry partnerships to assist academics in incorporating enduring health informatics and digital health capabilities into curricula.
Acknowledgement
The authors thank the workshop attendees for their generous participation in this publication's workshop discussion and support. The authors also thank the Australian Institute of Digital Health for providing support and a platform for the workshop to occur. A/Professor Zerina Lokmic-Tomkins is a recipient of Monash’s Education Research Fellowship: Framing Postgraduate Curriculum and Assessment for Digital Health.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 15th Nursing Informatics International Congress. (2021). Development of curriculum frameworks: Embedding health informatics into entry-to-practice nursing curriculum. Available from: https://ni2021.org/program/workshops/.
- Archibald, M. M., & Barnard, A. (2018). Futurism in nursing: Technology, robotics and the fundamentals of care. Journal of Clinical Nursing, 27(11–12), 2473–2480. https://doi.org/10.1111/jocn.14081
- Aungst, T. D., & Patel, R. (2020). Integrating digital health into the curriculum-considerations on the current landscape and future developments. Journal of Medical Education and Curricular Development, 7, 2382120519901275.
- Australian Nursing and Midwifery Federation (ANMF). (2015). National Informatics Standards for Nurses and Midwives. Australian Government Department of Health and Ageing. Available from: http://anmf.org.au/documents/National_Informatics_Standards_For_Nurses_And_Midwives.pdf.
- Booth, R. G., Strudwick, G., McBride, S., O’Connor, S., & Solano López, A. L. (2021). How the nursing profession should adapt for a digital future. BMJ, 373, n1190. https://doi.org/10.1136/bmj.n1190
- Brinkmann, S., & Kvale, S. (2015). Interviews: Learning the craft of qualitative research interviewing. Sage Publications.
- Brunner, M., McGregor, D., Keep, M., Janssen, A., Spallek, H., Quinn, D., Jones, A., Tseris, E., Yeung, W., Togher, L., Somlan, A., & Shaw, T. (2018). An eHealth capabilities framework for graduates and health professionals: Mixed-methods study. Journal of Medical Internet Research, 20(5), e10229. https://doi.org/10.2196/10229
- Canadian Association of Schools of Nursing. (2015). Nursing informatics entry to practice competencies for registered nurses Available from: https://www.casn.ca/2014/12/nursing-informatics-entry-practice-competencies-registered-nurses-2/.
- Clauson, K. A., Breeden, E. A., Fingado, A. R., Kaing, C. L., Flynn, A. J., & Cutler, T. W. (2018). A progress report on the state of pharmacy informatics education in US pharmacy schools and colleges. American Journal of Pharmaceutical Education, 82(7), 6332. https://doi.org/10.5688/ajpe6332
- Creswell, J. W., & Poth, C. N. (2018). Qualitative inquiry and research design choosing among five approaches (4th ed.). SAGE Publications Inc.
- Dagliati, A., Malovini, A., Tibollo, V., & Bellazzi, R. (2021). Health informatics and EHR to support clinical research in the COVID-19 pandemic: An overview. Briefings in Bioinformatics, 22(2), 812–822. https://doi.org/10.1093/bib/bbaa418
- Easterday, M., Rees Lewis, D., & Gerber, E. (2014). Design-based research process: Problems, phases, and applications. Proceedings of International Conference of the Learning Sciences, ICLS, 1, 317–324.
- Edirippulige, S., Brooks, P., Carati, C., Wade, V. A., Smith, A. C., Wickramasinghe, S., et al. (2018a). It's important, but not important enough: eHealth as a curriculum priority in medical education in Australia. Journal of Telemedicine and Telecare, 24(10), 697–702. https://doi.org/10.1177/1357633X18793282
- Edirippulige, S., Samanta, M., & Armfield, N. R. (2018b). Assessment of self-perceived knowledge in e-health among undergraduate students. Telemedicine and e-Health, 24(2), 139–144. https://doi.org/10.1089/tmj.2017.0056
- Edirippulige, S., Smith, A. C., Wickramasinghe, S., & Armfield, N. R. (2018c). Examining the influence of E-health education on professional practice. Journal of Medical Systems, 42(11), 215. https://doi.org/10.1007/s10916-018-1084-5
- Egbert, N., Thye, J., Hackl, W. O., Müller-Staub, M., Ammenwerth, E., & Hübner, U. (2019). Competencies for nursing in a digital world. Methodology, results, and use of the DACH-recommendations for nursing informatics core competency areas in Austria, Germany, and Switzerland. Informatics for Health & Social Care, 44(4), 351–375. https://doi.org/10.1080/17538157.2018.1497635
- Graneheim, U. H., Lindgren, B. M., & Lundman, B. (2017). Methodological challenges in qualitative content analysis: A discussion paper. Nurse Education Today, 56, 29–34. https://doi.org/10.1016/j.nedt.2017.06.002
- Honey, M., Collins, E., & Britnell, S. (2018). Guidelines: Informatics for nurses entering practice. The University of Auckland. https://doi.org/10.17608/k6.auckland.7273037.v2
- Honey, M., Collins, E., & Britnell, S. (2020). Education into policy: Embedding health informatics to prepare future nurses-New Zealand case study. JMIR Nursing, 3(1), e16186. https://doi.org/10.2196/16186
- Honey, M., Collins, E., & Britnell, S. (2021). Identifying How to support nurse educators nationally to teach nursing informatics. Studies in Health Technology and Informatics, 284, 124–129.
- Honey, M. L. L., Skiba, D. J., Procter, P., Foster, J., Kouri, P., & Nagle, L. M. (2017). Nursing informatics competencies for entry to practice: The perspectives of six countries. Studies in Health Technology & Informatics, 232, 51–64.
- Hubner, U., Shaw, T., Elias, B., Bell, S., & Blake, R. (2018). EU*US eHealth Work Project H2020-SC1-HCO13-2016.
- Hubner, U., Shaw, T., Thye, J., Egbert, N., Marin, H. F., Chang, P., et al. (2018). Technology informatics guiding education reform - TIGER. Methods of Information in Medicine, 57(S 01), e30–e42. https://doi.org/10.3414/ME17-01-0155
- Kinnunen, U. M., Rajalahti, E., Cummings, E., & Borycki, E. M. (2017). Curricula challenges and informatics competencies for nurse educators. Studies in Health Technology and Informatics, 232, 41–48.
- Lindgren, B. M., Lundman, B., & Graneheim, U. H. (2020). Abstraction and interpretation during the qualitative content analysis process. International Journal of Nursing Studies, 108, 103632. https://doi.org/10.1016/j.ijnurstu.2020.103632
- Lokmic-Tomkins, Z., Brar, S., Lin, N., Khor, M., Mathews, K., & Lawlor, K. (2021). Advancing nursing informatics through clinical placements: Pilot study. Studies in Health Technology and Informatics, 284, 98–102.
- Lokmic-Tomkins, Z., Choo, D., Foley, P., Dix, S., Wong, P., & Brand, G. (2022). Pre-registration nursing students' perceptions of their baseline digital literacy and what it means for education: A prospective COHORT survey study. Nurse Education Today, 111, 105308. https://doi.org/10.1016/j.nedt.2022.105308
- Lokmic-Tomkins, Z., Gray, K., Cheshire, L., Parolini, A., Sharp, M., Tarrant, B., Hill, N., Rose, D., Webster, M., Virtue, D., Brignell, A., Waring, R., Broussard, F., Tsirgialos, A., & Meng Cham, K. (2023). Integrating interprofessional electronic medical record teaching in preregistration healthcare degrees: A case study. International Journal of Medical Informatics, 169, 104910. http://doi.org/10.1016/j.ijmedinf.2022.104910
- Lombardo, L., Wynne, R., Hickman, L., & Ferguson, C. (2021). New technologies call for new strategies for patient education. European Journal of Cardiovascular Nursing, 20(5), 399–401. https://doi.org/10.1093/eurjcn/zvab026
- Mantas, J. (2020). The importance of health informatics in public health during the COVID-19 pandemic. Studies in Health Technology and Informatics, 272, 487–488.
- McBride, S. G., Tietze, M., & Fenton, M. V. (2013). Developing an applied informatics course for a doctor of nursing practice program. Nurse Educator, 38(1), 37–42. https://doi.org/10.1097/NNE.0b013e318276df5d
- Nagle, L. M., Crosby, K., Frisch, N., Borycki, E., Donelle, L., Hannah, K., et al. (2014). Developing entry-to-practice nursing informatics competencies for registered nurses. Studies in Health Technology and Informatics, 201, 356–363.
- Nagle, L. M., Kleib, M., & Furlong, K. (2020a). Digital health in Canadian schools of nursing part A: Nurse educators' perspectives. Quality Advancement in Nursing Education - Avancées en Formation Infirmière, 6(1), 1–17. https://doi.org/10.17483/2368-6669.1229
- Nagle, L. M., Kleib, M., & Furlong, K. (2020b). Digital health in Canadian schools of nursing--part B: Academic nurse administrators' perspectives. Quality Advancement in Nursing Education - Avancées en Formation Infirmière, 6(3), 1–28. https://doi.org/10.17483/2368-6669.1256
- O'Brien, B. C., Harris, I. B., Beckman, T. J., Reed, D. A., & Cook, D. A. (2014). Standards for reporting qualitative research: A synthesis of recommendations. Academic Medicine: Journal of the Association of American Medical Colleges, 89(9), 1245–1251. https://doi.org/10.1097/ACM.0000000000000388
- Pontefract, S. K., & Wilson, K. (2019). Using electronic patient records: Defining learning outcomes for undergraduate education. BMC Medical Education, 19(1). https://doi.org/10.1186/s12909-019-1466-5
- Procter, P. M. (2017). Ubiquitous adoption of innovative and supportive information and communications technology across health and social care needs education for clinicians. Studies in Health Technology and Informatics, 235, 358–362.
- Royal College of Nursing. (2018). Every nurse an e-nurse: Digital capabilities for 21st century nursing. [cited 2022 28th of March]. Available from: https://www.rcn.org.uk/professional-development/publications/pdf-007013.
- The Commonwealth Fund. (2016). Developing a framework for evaluating the patient engagement. Quality, and Safety of Mobile Health Applications. Available at: https://www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_issue_brief_2016_feb_1863_singh_framework_evaluating_mobile_health_apps_ib_v2.pdf.
- The Design-Based Research Collective. (2003). Design-Based research: An emerging paradigm for educational inquiry. Educational Researcher, 32(1), 5–8. https://doi.org/10.3102/0013189X032001005
- Vaismoradi, M., Jones, J., Turunen, H., & Snelgrove, S. R. (2016). Theme development in qualitative content analysis and thematic analysis. Journal of Nursing Education and Practice, 6(5), 100. https://doi.org/10.5430/jnep.v6n5p100
- Walpole, S., Banerjee, A., & Taylor, P. (2017). Health informatics in UK medical education: A survey of current practice. Future Healthcare Journal, 4(Suppl 2), s24. https://doi.org/10.7861/futurehosp.4-2-s24
- Wong, P., Brand, G., Dix, S., Choo, D., Foley, P., & Lokmic-Tomkins, Z. (2023). Pre-Registration nursing students' perceptions of digital health technology on the future of nursing: A qualitative exploratory study. Nurse Educator. Advance online publication. https://doi.org/10.1097/NNE.0000000000001591
- World Health Organisation. (2021). Global strategy on digital health 2020–2025. Available at: https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf.

