ABSTRACT
India has been historically challenged by an insufficient and heterogeneously clustered distribution of healthcare infrastructure. While resource-limited healthcare settings, such as major parts of India, require multidisciplinary approaches for improvement, one key approach is the recruitment and training of a healthcare workforce representative of its population. This requires overcoming barriers to equity and representation in Indian medical education that are multi-faceted, historical, and rooted in inequality. However, literature is lacking regarding the financial or economic barriers, and their implications on equity and representation in the Indian allopathic physician workforce, which this review sought to describe. Keyword-based searches were carried out in PubMed, Google Scholar, and Scopus in order to identify relevant literature published till November 2023. This state-of-the-art narrative review describes the existing multi-pronged economic barriers, recent and forthcoming changes deepening these barriers, and how these may limit opportunities for having a diverse workforce. Three sets of major economic barriers exist to becoming a specialized medical practitioner in India – resources required to get selected into an Indian medical school, resources required to pursue medical school, and resources required to get a residency position. The resources in this endeavor have historically included substantial efforts, finances, and privilege, but rising barriers in the medical education system have worsened the state of inequity. Preparation costs for medical school and residency entrance tests have risen steadily, which may be further exacerbated by recent major policy changes regarding licensing and residency selection. Additionally, considerable increases in direct and indirect costs of medical education have recently occurred. Urgent action in these areas may help the Indian population get access to a diverse and representative healthcare workforce and also help alleviate the shortage of primary care physicians in the country. Discussed are the reasons for rural healthcare disparities in India and potential solutions related to medical education.
Introduction
Healthcare in India has historically been unfavorably distributed and inaccessible for a large majority of the population, with considerable and persistent rural-urban inequality [Citation1]. This is superimposed on a dearth of physicians, given that data from 2019 indicated that India had merely 70 physicians per 100,000 people [Citation2]. Further, Indian citizens have historically had to bear the brunt of healthcare expenditure – as of 2020, the average per capita health expenditure by the government in India was 3 Indian National Rupees (INR) per day, covering only 30% of the total costs incurred [Citation3]. With only a minority having health insurance coverage [Citation4,Citation5], these costs are largely borne through out-of-pocket spending. In a country where 273 million live below the poverty line, a number that has only expanded with the COVID-19-associated economic recession, these conditions represent a challenging scenario [Citation6,Citation7]. These challenges become compounded by the heterogeneous mix of public and private coverage of healthcare costs, with patients caught in between, unlike countries that have healthcare for all [Citation2,Citation8–10].
While bridging the gap in resource-limited settings requires multidisciplinary approaches, one of the primary pathways remains the recruitment and training of a healthcare workforce that is representative of the population it serves [Citation11,Citation12]. It is widely recognized that medical students from rural, underserved areas are more likely to practice or return to practice in these areas, providing impetus for their recruitment [Citation11,Citation13].
Over the past years, several authors have extensively described challenges and problems in the evolving Indian medical education system [Citation14–18]]. However, literature is lacking regarding the systemic challenges presented in the training of a representative physician workforce in India from the economic feasibility and equity standpoints. This article sought to review the current status and future trends of inequities and economic barriers to medical education in India, along with factors impacting them. Therefore, keyword-based searches were carried out in PubMed, Google Scholar, and Scopus, using various combinations of ‘India’, ‘medical education’, ‘medical college’, ‘clinical training’, ‘Medical Council of India’, ‘privatization’, ‘economic barrier’, ‘NEET’, ‘National Eligibility cum Entrance Test’, ‘student selection’, ‘residency’, ‘fellowship’, ‘specialization’, ‘financial barrier’, to identify relevant academic and non-academic works, published up until November 2023, which have been summarized below. This narrative review also discusses the existing multipronged inequities in medical education and forthcoming changes that may worsen them and describes how these may limit opportunities for Indian physicians-in-training. Finally, this article describes the conditions behind rural healthcare disparities in India from a lens of medical education and suggests potential solutions for their amelioration.
Medical education in India
A broad overview of the medical education system in India is warranted to understand the nature of the existing and potentially forthcoming economic barriers here. Becoming a medical specialist in India requires a candidate to formally complete five and a half years of medical school training, followed by at least three years of specialization in a residency program [Citation19,Citation20]. As of 2023, annually-held, norm-referenced, standardized entrance examinations – the National Eligibility cum Entrance Test (NEET) Undergraduate (NEET-UG), Postgraduate (NEET-PG), and Super-Specialty (NEET-SS) – determine admission to medical school, residency, and fellowship training respectively [Citation21]. While the concept of NEET was originally introduced in 2013, a series of false starts, problems of test integrity, and legal challenges led to a delayed full national adoption in 2017 [Citation21].
Currently, the sole criterion in India for selection at each stage of training is the rank obtained by the candidate on these norm-referenced tests [Citation21]. This contrasts with the United Kingdom (U.K.) and the United States (U.S.) – two high-income countries whose medical education systems most readers are familiar with – where a more holistic review of each medical school applicant is performed [Citation22,Citation23]. Given the number of applicants in India, the competitiveness is significant at each stage. In 2023, the NEET-UG was taken by over 2 million candidates for admission to medical school, of which there were 108,898 positions available (per capita = 0.052) [Citation24,Citation25]. For comparison, in 2023, about 26,820 candidates in the U.K. competed for about 7,600 medicine positions (per capita = 0.28), a candidate-to-position ratio that was approximately 5 times less competitive than that of India [Citation26].
The supply-demand mismatch extends beyond medical school positions, and candidate numbers remain substantial for residency selection. In India, the number of candidates taking NEET-PG annually (2018–2020) to obtain postgraduate training was three times higher than the number of the United States Medical Licensing Exam (USMLE) examinees and fourteen times greater than that of the U.K.‘s Professional and Linguistics Assessment Board (PLAB) examinees, with a far lower proportion of candidates successfully getting residency seats in India [Citation27–30]. In India, the significantly higher competitiveness of medical education gets compounded by other factors, including several economic barriers.
Inequities in and economic barriers to medical education in India
Barriers to medical education are multi-faceted, historical, and rooted in inequality. This review focuses on financial or economic barriers, and their implications on equity and representation in the allopathic physician workforce. Not discussed in detail in this review, are healthcare practice models that India recognizes as as formal alternatives to allopathic medicine: Ayurveda, Yoga, Naturopathy, Unani, Siddha, Sowa Rigpa, and Homeopathy (AYUSH). The former is more commonly referred to in Indian literature as ‘modern medicine’ while the latter is ‘traditional, complementary and alternative medicine’ (TCAM) [Citation16,Citation31]. Education in TCAM is beyond the scope of this work.
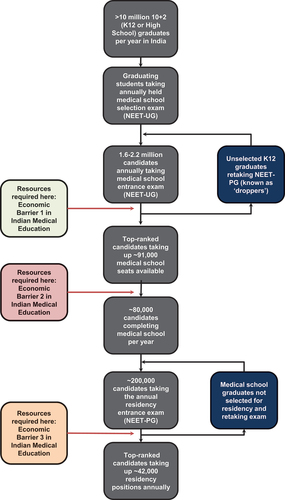
Economic challenges may be considered to confluence into three sets of barriers, which must be crossed by each applicant aiming to become a specialist physician in India: (A) NEET-UG for receiving admission to medical school and its related barriers, (B) Barriers related to resources required for medical school, including tuition costs and educational material, and (C) NEET-PG for getting a residency position and related barriers. Given the extreme heterogeneity and high levels of inequality in India, these barriers are trivial for some and substantial for many [Citation32]. These are summarized in and discussed below. While candidates face considerable financial barriers, we note that these are exacerbated by, and intersect with historically rooted social and caste-based disparities, which we touch upon briefly.
Figure 1. Summary of the three major financial barriers to medical education in India, which limit the training of a diverse and representative healthcare workforce.
(A) Economic barriers related to medical school admissions
The first set of barriers pertain to admission into medical school (). As of November 2023, India has 706 medical schools offering 108,898 training positions for a Bachelor of Medicine, Bachelor of Surgery (MBBS) degree [Citation25]. Candidates aiming for these positions through the NEET-UG are graduates of senior secondary school (grade 12, also known locally as 10 + 2), who either take the exam soon after graduation, or after one or more ‘drop years’ for exam preparation. The NEET-UG examination carries major educational and cultural significance in India, with considerations of a chance at major upward social mobility featuring centrally, similar to the Chinese Gaokao examination [Citation33,Citation34]. Over 2 million applicants (20 lakhs in Indian context) registered for the NEET-UG 2023 exam (24).
The NEET-UG exam consists of 180 multiple-choice questions (MCQs) that are administered in a paper-based format. The exam is held once-a-year simultaneously across the nation, after which each test-taker gets an all-India rank (A.I.R.) and a ‘category rank’. This AIR is utilized in a nationwide process called ‘counseling’. ‘Counseling’ occurs using individual’s AIR and individual’s rank in their respective affirmative action category reported as ‘general category’, scheduled castes’, ‘scheduled tribes’, ‘other backward class’, ‘economically weaker section’, etc. During ‘counseling’, the candidate digitally submits a rank order list of preferred schools, with each school being filled in order of increasing A.I.R [Citation35]. The choice of the institution gets assigned after considering the individual’s affirmative-action-based-category rank, their institutional rank list, and the number of positions remaining. Thus, the first ranker is able to choose any school in the country, while an individual with an A.I.R. of 20,000 is precluded from admissions to the vast majority of top medical schools in India, unless belonging to any category other than the general category – a racial/caste-based framework that some have argued creates further financial inequity, by not prioritizing socio-economic status [Citation36,Citation37]. Here, it must be noted, the marks obtained in the MCQ-based examination decide the ranking of candidates for medical school, while subjective attributes such as communication skills and empathy do not come into the picture [Citation38–40].
The structure of NEET-UG predominantly follows the most widely used high school syllabus – that of the Central Board of Secondary Education (CBSE) [Citation41]. While little or no peer-reviewed literature exists regarding the content and validity of the NEET-UG questions, extensive anecdotal experience, including that of the authors, clearly indicates that NEET-UG’s questions are often far beyond the standard high school curricula. This makes additional preparatory resources necessary for pre-medical applicants, i.e., a parallel curriculum, particularly for those attending conventional high schools.
To bridge the gap between teaching at a standard high school and that needed to score well on the NEET-UG, multiple private coaching institutions (tutoring programs) have also emerged, offering preparatory courses from the 11th grade, but also reported to be as early as the 6th grade [Citation42], the latter being seven years before a student’s designated exam date. Enrollment at one of these institutions, typically concurrent with enrollment in high school or, less commonly, after high school (during dedicated ‘drop years’), has been a historically consistent and strong surrogate for success on the NEET-UG. Data from 2017–2019 indicate that over 50% of the top 100 rank holders in NEET-UG have been trained at one of these coaching institutions [Citation43]. Further, at India’s highest-ranked medical school, the All-India Institute of Medical Sciences (AIIMS), New Delhi, most of the incoming class of 2019 had attended the same private coaching institute [Citation44]. To prevent exhaustion from the parallel curriculum, several institutions, called ‘dummy schools’, have evolved that ask students to only sit for each grade’s final exams and not attend regular high school classes, instead focusing on NEET-UG preparation [Citation45]. These dummy schools ensure that students receive focused tutoring for NEET-UG, either by providing it themselves, or by collaborating with major established tutoring firms. The emergence of these dummy schools adds greater credence to the pre-eminent role of coaching for NEET-UG in admissions to medical schools.
The converse association related to additional training has also been true – candidates not taking additional coaching have significantly lower odds of high ranks in the NEET-UG. In Tamil Nadu – a state with high literacy rates that is acknowledged for its above-average quality of school education – fewer than 2% of 2019 NEET-UG examinees who did not avail of private coaching obtained a medical training position [Citation46,Citation47]. Direct causal evidence, along with peer-reviewed literature, remains lacking as to the impact of coaching institutions on medical school selection in India. However, the presently existing indirect and anecdotal evidence lends support to their ‘perceived’ value to applicants, which has been increasing in recent years. Considering this, it is not unreasonable to conclude that the utilization of private tutoring programs (coaching centers) has become not just an additional source of education, but a perceived necessity for high ranks in the high-stakes, single-shot (per year) NEET-UG.
Major barriers to those under-represented in medicine come up in the form of annual fees for these institutions, analogous to the costs of private tutoring afforded by privileged candidates for the Medical College Admissions Test (MCAT) in the U.S (). The tuition fees in Indian pre-medical coaching institutes are frequently far more than that of high schools, ranging from 50,000 to 100,000 INR (USD 611–1233) [Citation48–58]. These expenses are widely known to be difficult to pay for the vast majority of the populace, given the average, unadjusted, annual per-capita income of Indian citizens is just over 100,000 INR [Citation49]. Thus, the first pillar of inequity in the path to physician training in India has become the need for preparation-related resources required to beat the extremely competitive NEET-UG assessment.
Table 1. Attendance costs at popular coaching institutes for the medical school entrance examination (NEET-UG) with prices detailed as listed on the official institute websites [Citation50–58].
(B) Economic barriers related to medical school attendance
The second set of economic barriers and inequity in the Indian medical education system is the expenditure involved in attending and succeeding in medical school (). Two tiers of allopathic medical education exist in India, one tier comprising heavily subsidized positions and the other tier being completely self-funded in nature.
There exist significant differences in quality and extreme differences in cost between the two tiers of allopathic medical education [Citation14,Citation16–18,Citation21,Citation59,Citation60,Citation60–62]. Generally, the subsidized education consists of (1) all positions at publicly funded institutions, more widely known in India as Government Medical Colleges (GMCs), or (2) some positions in select privately funded institutions where the state government has ensured a quota of subsidized positions and annual tuition fees typically are between INR 10,000 and INR 40,000 (~ USD 100–500). Meanwhile, the remaining positions, typically always in private institutions, make up the other tier and demand typically 1–3 orders of magnitude higher tuition fees than subsidized positions from candidates. Typical annual tuition costs, as seen from the websites of these institutions, are over INR 20,00,000 (~ USD 25,000) [Citation59,Citation63]. The relative affordability of government-funded medical schools renders them significantly more competitive, notwithstanding their generally higher quality of clinical training as well [Citation17]. In 2023, only 2.8% of all NEET-UG takers were able to join GMCs [Citation64]. Most privately funded medical schools offer significant financial barriers for the average candidate, allowing only the more affluent to attend [Citation60,Citation65]. Strict regulation of fees in private medical schools was relaxed nearly two decades ago after the judicial decision of the Supreme Court of India in the landmark case of ‘T.M.A. Pai Foundation and Others’ vs ‘State of Karnataka and Others’ and related judgments. The apex court ruled on the right of citizens to establish and administer private educational institutions and charge fees higher than those set in public medical schools for economic and non-economic reasons [Citation66,Citation67]. The judicial decision also explicitly permitted their own selection criteria, which morphed into years of multiple parallel medical school application systems, each with their own, sometimes exorbitant, costs [Citation60]. One expected indirect consequence of the introduction of NEET-UG in 2016 was a reduction in some of these costs, although currently that goal has not been fully realized [Citation67,Citation68].
However, recent years have seen rising inequity in subsidized education as well, with several state governments enacting tuition fee increases such as Punjab (75% increase), Haryana (95%), and Gujarat (400%) [Citation69–71]. These fee increases make it more challenging for applicants with limited resources to enroll even at government-funded institutions here, and thus may contribute to making the in-training workforce less representative of the population it serves.
In addition to tuition fees, requisite medical school course material also represents a not-insignificant expenditure for candidates. For example, the classic textbook Harrison’s Principles of Internal Medicine, often considered a required purchase for the internal medicine (general medicine) coursework for MBBS in the Indian setting, costs nearly INR 10,000, with similar costs involved for the remaining subjects in Indian curricula [Citation72]. With most institutional libraries carrying a limited number of copies for short-term borrowing, purchasing one’s own remains the only way forward for most medical students. Anecdotally, the total expenditure on required textbooks alone may go up to INR 20,000 per year, resulting in students from less-privileged backgrounds opting for either old textbooks or foregoing purchases completely.
Thus, the expenses incurred in attending medical school represent the second set of economic barriers in Indian medical education. However, a dearth of medical education-related research in India results in evidence being lacking regarding how these expensive resources for medical school may disenfranchise those from underprivileged backgrounds. Urgent work is needed to quantify the rapidly increasing inequities associated with the costs of attending medical school and how these may be linked with preexisting socio-economic disparities.
(C) Economic barriers related to residency selection and training
Upon completing medical school, candidates who wish to pursue residency training in India must take the NEET-PG, another national standardized examination held once a year [Citation73]. For a few, highly coveted institutions, called ‘Institutes of National Importance (INI)’, candidates must take the INI-Common Entrance Test (INI-CET), which also functions like the NEET-PG but only offers a few hundred positions [Citation74]. Similar to medical school admissions, a substantial supply-demand mismatch exists at the residency level. Merely a fourth of all candidates writing the exam manage to get any residency position, with far fewer getting the specialty of their choice [Citation75,Citation76]. For the sake of clarity, we will restrict our narrative in this section to the NEET-PG, which determines candidate selections for the vast majority of available training spots, while the INI-CET determines selections for far fewer spots.
As with the NEET-UG, a gap exists between the preparation required for completing medical school and that required to attain high ranks on the NEET-PG, which allows candidates to pick their specialty and institution of choice. Specifically, medical school training heavily focuses on clinically relevant material. Meanwhile, the NEET-PG, in addition to clinical knowledge, has a heavy focus on the recall of public health statistics and basic science minutiae, such as identifying chromosomal loci of specific gene mutations behind rare diseases [Citation77]. This curricular mismatch gives rise to the utility of enrollment in private coaching institutions for medical students and graduates.
While academic literature regarding their significance and perceived utility in preparing for the NEET-PG is lacking, some low-quality observational data provide high support for their ‘perceived value’. For example, a single coaching institute trained the majority of the top rank holders in the NEET-PG in 2022 [Citation78]. Meanwhile, in all the Indian institutions the authors of this work are affiliated to, over 80% of students had been utilizing some form of NEET-PG coaching, either offline or online. Thus, the argument can be made that, like NEET-UG, enrollment and utilization of coaching companies have increasingly become a surrogate for excellent performance in the NEET-PG.
Attendance at these coaching institutions, increasingly seen as a necessary condition for success in NEET-PG, comes accompanied by significant costs. The tuition costs for attending the most popular institutions have been summarized in , through data collection from online sources and personal inquiries [Citation78–84].
Table 2. Attendance costs at popular coaching institutes for the residency entrance examination (NEET-PG) with prices detailed as listed on the official institute websites [Citation78–84].
INR, Indian National Rupees; DAMS, Delhi Academy of Medical Sciences; DBMCI, Dr. Bhatia Medical Coaching Institute. N.A., Not Available.
While this review discusses tuition fees at Indian medical schools, it underestimates the true costs incurred by omitting several tangibles. For online classes that came to the fore in India after COVID-19, these include, but are not limited to a good internet connection and a smartphone, laptop, or tablet for viewing – laptops and tablets being digital devices that are not widely available or affordable to all Indian students. For in-person sessions, costs related to transportation to, and accommodation in cities where these sessions are held also have to be accounted for. In an effort to curb these costs, one of the largest health universities in the country, to which dozens of medical schools are affiliated, announced plans for an affordable, university-led coaching regimen for NEET-PG [Citation85]. While it remains to be seen whether the services offered here can match that of popular coaching institutions, such an initiative underscores the perceived necessity of such programs. Given that education loans in India do not cover tuition costs related to attendance at private coaching institutions, students from unprivileged backgrounds continue to face substantial difficulties in accessing a resource perceived as necessary for getting a residency position.
There are nearly 620 medical schools and hospitals offering residency training in India [Citation86]. In contrast to US, UK, Canada, where residency trainees have guaranteed salary from institutions, India does not have the same homogeneity in trainee salaries, to the extent that some institutions do not pay their residents [Citation87]. Where they do receive a salary, it is typically meager [Citation88]. Further, most institutions charge residents tuition fees. Merely 16% of these institutions have been previously reported to have annual fees for residency training of less than INR 100,000, while 18% had annual fees between INR 300,000–500,000, and 43% more than INR 500,000 [Citation86]. Institutions with lower tuition fees and much better residency stipends, usually being government-funded medical schools or hospitals, are far more competitive.
Overall, residency training could result in a major short-term financial expense, particularly where these fees are significant. Meanwhile,candidates who could afford to settle for lower ranked residency programs that charge significant tuition fees, after not attaining ranks high enough, are typically well-off, so can again choose to pursue these opportunities, while less privileged candidates are unable to do so. Frequently, the latter group overlaps heavily with the same set of candidates who lacked the resources for high-quality NEET-PG preparation, including attendance at private coaching institutions. This situation gets compounded by federal policies that allow NEET-PG test-takers of certain historically disadvantaged ethnicities scoring in the zero percentile to be eligible for residency training – privileged candidates with dangerous standards of medical knowledge are thus able to choose extremely expensive private/self-funded residency programs, while less privileged candidates are precluded from such programs.
Thus, entry to residency, and residency training itself, represent the third major set of financial barriers for Indian medical candidates (). The system works against individuals coming from difficult backgrounds while supporting those with financial resources, resulting in, at the end of the pipeline, a workforce that is wholly different from the population it serves.
Potential inequities related to forthcoming educational reforms
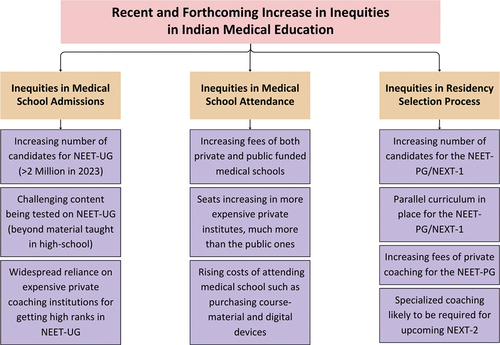
These preexisting economic barriers may be further exacerbated by several recent and forthcoming changes in medical education, the most important of which are: (A) the introduction of an MBBS exit exam and (B) proposed changes in the structure and timing of the residency selection exam ().
Figure 2. Multidimensional increases in inequities in medical education secondary to recent and forthcoming changes and educational trends in India.
Currently, the 5.5-year MBBS course in India includes a year of ‘internship’, which begins once the student qualifies the ‘MBBS Final Professional Part-II’ exams. Medical school exams assess both theoretical knowledge and practical skills; they are criterion-referenced tests, i.e., they test for the presence or absence of a predetermined level of competence. During this internship year, students rotate with various clinical departments and are provided with a provisional license to practice under supervision. A full license and a permanent medical degree are both awarded after completion of internship, unlike in the U.K. or U.S., where the internship year is not considered a part of medical school [Citation89,Citation90]. After receiving their medical degree and full license, graduates may opt to work as primary care physicians, in lieu of, or before undertaking, further residency training.
In July 2021, the Indian government announced the forthcoming plan to discontinue the NEET-PG and INI-CET [Citation91] and replace them with the National Exit Test (NEXT), the introduction of which was originally slated for 2023, but was deferred (deferred till further notice.) [Citation92]. The purported functions of NEXT are two-fold: (A) assessing the competence of students completing medical school, as a standardized nation-wide exit exam, and (B) sorting candidates through a norm-referenced process for residency selection.
NEXT has been planned to contain two parts: (A) NEXT-1, a multiple-choice test with a similar structure to NEET-PG, and (B) NEXT-2, an in-person live examination assessing clinical skills [Citation91]. Candidates will have to achieve a minimum passing score in both NEXT-1 and NEXT-2 to secure licensure. In addition to this, each candidate’s NEXT-1 score will be used to determine their competitiveness for residency training selection. With this proposed design, NEXT, particularly NEXT-1, will be directed to act as both a criterion- and a norm-referenced test – it will be expected by test providers to perform the function of both an exit exam and a ranking exam [Citation91].
Given the proposed design, NEXT-1 closely resembles its predecessor, the NEET-PG. While it may be appropriate for ranking purposes, it carries the risk of furthering inequity if used for licensing. If cut-off scores are set too high, it could complicate licensure requirements by skewing success toward candidates able to afford private coaching services. This scenario, with NEXT-1 serving as both a norm-referenced and criterion-referenced test, was one that U.S. medical licensing boards steered away from, beginning in early 2022 [Citation93]. Specifically, USMLE Step 1, an exam originally intended only for licensure, had evolved as a significant determinant of admission to residency, with many residency programs stratifying candidates by setting ‘cut-off’ Step 1 scores to determine which candidates received interview invitations. Over time, the disproportionate importance of the USMLE Step 1 score led to several pitfalls, including the development of a ‘parallel curriculum’ [Citation93,Citation94], wherein students prioritized studying for USMLE examinations over their medical school curriculum. Mitigating this trend was one reason for U.S. regulatory boards to convert USMLE Step 1 score reporting from a three-digit number to a pass/fail outcome [Citation93,Citation95]. It is possible that, with time, NEXT-1 may bring about similar concerns in Indian medical training.
Meanwhile, although NEXT-2 is slated to be a practical exam assessing clinical competence, reported in a pass-or-fail format, it is likely that here too, private coaching programs will emerge as a key player in passing this exam. This assertion, rooted in history, is derived from the numerous courses of testing companies geared toward candidates taking the practical components of licensing exams in the U.S. (the now defunct USMLE Step 2 C.S.), the U.K. (PLAB Part 2 or UKMLA clinical skills assessment), and Canada (the NAC-OSCE exam) [Citation96,Citation97]. As discussed earlier, this continued reliance on coaching and the incurred expenses could exacerbate financial struggles for disadvantaged Indian medical students. One particularly problematic scenario is the possibility of underprivileged trainees, who could not afford tutoring/coaching, failing NEXT, thereby neither securing a residency position nor a license to practice as a primary care physician.
This aside, a standardized, English practical exam, similar to USMLE Step 2 C.S. or PLAB 2, is neither feasible nor realistic in India. Each state is a microcosm of Indian society with various languages and dialects. The average Indian citizen may not be fluent in English or even classical Hindi, requiring that Indian doctors display competence that is also appropriately tailored to their loco-regional circumstances. Stakeholder consultation is warranted regarding a nuanced approach and consensus-based decision-making by administrators regarding the assessment criteria for NEXT-2.
Towards a US-style medical education system: implications for Indian healthcare
The Indian medical education system, in its acceptance of barriers to selection, high tuition costs, and debt burden to graduates, may be seen as analogously creeping towards trends seen in the medical education industry in the United States (U.S.). Over the last three decades, more than 75% of graduating medical students in the U.S. have belonged to affluent households [Citation98]. Further, in 2017, the median debt for graduating U.S. medical students was $192,000 [Citation99], representing a catastrophic expense where the median income is about one-third of this [Citation100]. Escalating educational costs facilitate the education of privileged non-minority students and those from affluent households [Citation101]. In addition to disproportionate access to high-performing institutions at every level of education, underprivileged students are victims of implicit bias of admissions committees who, for example, may prioritize students with expensive extracurricular activities such as sailing or crew [Citation102]. Moreover, student debt incurred in medical school represents a major discouraging factor for low-income, first-generation students who wish to pursue medical training in the U.S. Unfortunately, the National Medical Council (N.M.C.) of India does not report data on matriculating classes of students, including their financial and socio-economic status, unlike the American Association of Medical Colleges (AAMC).
These recent changes to the Indian medical school admission and licensure system, particularly with their financial implications, may exacerbate a skewed system, with potential repercussions extending to specialty training choice. Indeed, a longitudinal study of almost five thousand U.S. medical students found that approximately one-third of trainees who once intended to complete a primary care specialty switched to a higher-paying specialty by the final year, primarily in anticipation of the debt burden [Citation99]. In a parallel manner, Indian medical students, especially the ones scoring well on NEET-PG/NEXT-1, could edge away from primary-care specialties that are substantially needed, such as general internal medicine, family medicine, pediatrics, and obstetrics-gynecology. Additional repercussions include a potential greater inclination to relocating away from rural India upon graduation, further increasing disparities in healthcare access. Thus, while the current physician-in-training workforce may not represent the population it serves, these forthcoming changes could worsen the non-representativeness.
Barriers to rural practice, lessons, and potential solutions
Rural India suffers from a lack of access to healthcare facilities and shortages of doctors and paramedical professionals. While two-thirds of the Indian population reside in rural areas, only one-third of all healthcare workers works in these areas [Citation103]. This has led to an increasing number of untrained practitioners, typically non-physicians serving as the first point of care [Citation104]. Working conditions in these areas and the financial burden of medical training have led to doctors being less likely to take up needed but lower-paying specialties, and to work in deprived areas. Physicians, particularly specialists, often choose to work in urban areas instead of rural ones because of greater earning potential, better access to advanced facilities, a safer working environment, and better living conditions for their families in these areas [Citation105]. In addition, most Indian states do not have a workforce policy to ensure that doctors in the public health system are rotated between rural and non-rural postings, generating concern that once a trainee is posted to a village, they will be unable to relocate to a city of their choice [Citation106]. Further, institutional factors such as government rule changes, recruitment delays, and a lack of transparency in job postings, promotions, and transfers, compromise public sector efforts to hire and retain health workers in rural healthcare positions [Citation107].
Many proposed education-focused solutions to improve healthcare access in rural India have focused on training either mid-level, non-physician, or informal providers [Citation108–110]. For example, in 2001, the state of Chhattisgarh introduced a 3-year diploma course for rural medical assistants (R.M.A.s), with Assam instituting a similar course in 2004 [Citation104]. Meanwhile, Jishnu Das and colleagues, in 2016, reported findings from a seminal randomized controlled trial (RCT) of short-term training to non-credentialed informal providers conducted in rural India. Out of 304 informal providers, 152 received training over 9 months at a cost of $175/provider, resulting in 14% higher rate of correct case management, but no significant difference in utilization of unnecessary drug therapy [Citation111]. Private organizations have also contributed to these initiatives – the Liver Foundation has trained approximately 2200 practitioners in the states of West Bengal and Jharkhand, for over 150 hours each, with many of these providers being the only source of care in their respective villages. These initiatives, while well-meaning, have met legal challenges, including from the Indian Medical Association (I.M.A.). Concerns have been raised regarding the need for a separate regulatory framework, the lack of a clear career trajectory for R.M.A.s after training, and the ethics of substandard care [Citation104,Citation112]. Other efforts by medical regulatory bodies have focused on ensuring newly trained physicians, just after their MBBS, residency, or fellowship, work in rural medical centers in their state of training, for variable durations of time, through legally binding ‘bonds’ [Citation113]. After serving this period, they are free to practice elsewhere. While these efforts may ensure healthcare access in the short to mid-term, it can be argued that neither mid-level providers, nor a constantly changing cohort of freshly graduated physicians who are only working there due to legal obligations, constitute equitable access for the rural population. Thus, long-term initiatives must focus on attracting and retaining trained physicians in these areas to ensure truly equitable access.
Increasing public health spending, including providing higher salaries and other facilities for MBBS degree holders to work in villages, may reduce healthcare-related disparities. The World Bank data show that countries with a significant public share of healthcare funding and consumption expenditure per capita have better healthcare outcomes [Citation114]. However, budgetary allocations to healthcare in India has historically represented only about 1% of GDP [Citation66]. Notably, increased budgetary allocations to the National Rural Health Mission led to significantly improved health outcomes in rural areas [Citation115]. Thus, rural centers and programs should further be aided with medical equipment and renovation costs to enable qualified practitioners to have theresources to provide the requisite standard of clinical care. Further, efforts must be made to attract medical students to these communities to ensure sustainable improvement and a continuous pipeline of newly trained physicians. Funds should be set aside to better compensate MBBS degree holders to incentivize rural relocation, including relocation costs. These cost-effective incentives for early career physicians, may prevent federal expenditure of large incentives down the line in order to incentivize established physicians to relocate.
Worldwide, evidence suggests that medical students recruited from underserved or rural communities are more likely to return to those communities after completing their training, while sensitization of medical students to the issues in rural areas can improve recruitment [Citation116]. In a systematic review of over 100,000 medical students, the authors noted that belonging to an underserved community or ethnic minority, and exposure to underserved populations were associated with more favorable attitudes towards the underserved. They reported that experiential community-based learning, including volunteering in free clinics and social accountability-focused curricula, has demonstrated the best results amongst educational interventions [Citation116]. To this end, Morris et al., from the U.S., reported that physicians training at community health centers, rather than university centers, were almost three times more likely to work in an underprivileged area [Citation117]. A survey study of senior medical students from four Nepalese medical schools found that 12% wanted to practice in rural areas, with these students found to have a greater likelihood of being male, having been born in rural area, or to having been a recipient of rural service-based scholarship from the Ministry of Education [Citation118]. In Thailand, multi-sectoral planning activities that facilitated rural recruitment and hometown placement programs, where graduates were placed in their hometowns, have significantly improved the retention rate in underserved areas [Citation119].
Some medical schools are utilizing innovative models of medical education improving the recruitment of disenfranchised students, and incentivizing work in rural areas. In the U.S., following a large endowment gift in 2018, the New York University (NYU) Grossman School of Medicine no longer charges tuition for any of its medical students, regardless of merit or need [Citation120,Citation121]. Expected downstream benefits included the greater recruitment of local students, students from minority communities, as well as a greater proportion of graduates going into primary care and serving in rural areas [Citation122]. In rural India, Sri Madhusudan Sai Institute of Medical Sciences & Research (SMSIMSR), which received NMC approval in 2023, covers all student expenses without exception, including tuition and accommodation, deriving funding from donations [Citation123]. Following their training, students are required to work for a duration of five years in one of the institute’s affiliated hospitals, all of which provide tertiary care to patients completely free of charge. Recruitment of underprivileged students from rural areas is prioritized, who will go on to serve in these rural areas [Citation123,Citation124]. In 2023, SMSIMSR, admitted its first cohort of medical students, many of whom were from rural India and belonged to the lower socioeconomic strata [Citation125]. In South Africa, the Walter Sisulu Medical School, Mthatha enrolls students from the surrounding areas, which are among the country’s poorest [Citation126]. The medical school’s educational, research, and service initiatives are influenced heavily by the local populations’ needs, and recent data showed that almost 70% of their graduate doctors continued to work in these impoverished rural areas [Citation127]. Caution and thorough evaluation are however necessary, as data from the Nepalese survey found, surprisingly, that medical students at federally funded government medical schools, with lower tuition fees, had similar levels of intention to practice in Nepal as those at private medical schools [Citation118].
These examples bolster the notion that the medical trainee community must adequately represent rural and underserved populations. Prior literature has shown that patients prefer physicians from the same background, and diversity in the clinical team improves patient outcomes. If economic barriers keep these underrepresented students out of the system, India will likely continue to have crippling disparities in rural healthcare stemming from a lack of fresh graduates moving to these areas of their own volition, a point that has been raised previously [Citation128–130]. Thus, in such geographical areas with a health workforce scarcity, the Indian government would do well to recruit students with rural backgrounds through efforts such as reserving positions for these students in medical schools and reducing tuition fees for these students, among others. Additionally, on a national level, efforts must be made to introduce targeted education regarding underserved populations to sensitize students regarding the need for trained physicians in these areas [Citation103].
Additionally, the primary healthcare and generalist approach, when applied to medical education, indicates that health professionals must be able to provide a range of care for numerous conditions across a patient’s life cycle, for which their training must make them competent. Unfortunately, current medical education in the country is geared toward specialized tertiary care practice settings, contributing to the lack of motivation among medical students to take up primary care [Citation114]. For example, a survey of > 700 medical students across public and private institutions in 2013, by Diwan et al., found that > 90% wanted to specialize and > 60% wanted to practice in urban areas [Citation131]. Lessons may be learned from Queensland, Australia, where medical education is geared toward a generalist approach and specifically includes ‘training in community-based primary medical practice, health facility–based secondary medical practice, and hospital and community-based public health practice’ [Citation114,Citation131]. Several states in India do train family doctors to perform emergency procedures like cesarean sections or administer anesthesia for such procedures [Citation107], while there are a few notable Indian institutions that specifically offer primary care-oriented education. For example, in Christian Medical College, Vellore, and St. John’s Medical College, Bangalore, both in India, during their mandatory rural service, medical graduates are offered long-distance training in Family Medicine, to support the quality provision of primary healthcare in rural settings [Citation114]. Thus, in addition to improving the recruitment of students from rural backgrounds, leaders in medical education should promote greater emphasis on adequate primary care training during medical school. Finally, given that India lacks any dual degree medical school programs, efforts may be made to offer such services to increase the competency of the Indian healthcare workforce [Citation132]. These include programs offering, in addition to the MBBS degree, education in business administration (master of business administration – M.B.A.) or public health (master of public health – M.P.H.), or health-services-related science (master of science – MSc), Graduates of these programs can help tackle inequity – candidates having education in healthcare leadership may lead efforts in targeted infrastructure development and resource allocation, while those with an MSc in health services research can help quantify hitherto under-studied geographic disparities.
Conclusions
While academic literature on inequity in medical education in India is lacking, this article describes three major levels of economic barriers to becoming a clinical specialist in India, as well as downstream consequences for the Indian healthcare system ( and ).These barriers include barriers to get selected into a medical school in India, barriers to pursue medical school, and barriers to secure a residency position. Urgent action on these inequities may help the Indian population get access to a representative and inclusive workforce and may also help alleviate the shortage of primary care physicians in the country. Equitable care requires urgent redressal of increasing costs associated with medical training in India. Policy-related reforms, standardization of Indian medical education, and legislative action, can together potentially enable candidates an equitable opportunity to care for the nation’s most vulnerable groups and help ensure population-wide just outcomes.
Consent for publication
All authors provide consent for publication of this manuscript.
Contributorship Statement
All authors approve the manuscript as it is written.
Authors’ contributions:
FR conceptualized, drafted, edited, and revised the manuscript. VB conceptualized, drafted, edited, and revised the manuscript. AO conceptualized, drafted, edited, revised the manuscript, and corresponded with the journal. DD edited and revised the manuscript. MSA revised the manuscript. All authors reviewed the final version of this manuscript.
Acknowledgments
The authors wish to thank Prof. Michael McDermott, M.D., Chief Medical Executive of Miami Neuroscience Institute for his thoughtful edits and Prof. Jishnu Das, PhD, Professor at Georgetown University for his feedback during the manuscript revisions.
Disclosure statement
Manmeet Singh Ahluwalia: Grants: AstraZeneca, B.M.S., Bayer, Incyte, Pharmacyclics, Novocure, MimiVax, Merck. Consultation: Bayer, Novocure, Kiyatec, Insightec, G.S.K., Xoft, Nuvation, Cellularity, SDP Oncology, Apollomics, Prelude, Janssen, Tocagen, Voyager Therapeutics, Viewray, Caris Lifesciences, Pyramid Biosciences, Varian Medical Systems, Cairn Therapeutics, Anheart Therapeutics, Theraguix. Scientific Advisory Board: Cairn Therapeutics, Pyramid Biosciences, Modifi Biosciences. Stock shareholder: Mimivax, Cytodyn, MedInnovate Advisors. Faique Rahman, Vivek Bhat, Ahmad Ozair, and Manmeet Ahluwalia completed medical school in India. All other authors declare no relevant disclosures.
Additional information
Funding
References
- Banerjee S. Determinants of rural-urban differential in healthcare utilization among the elderly population in India. BMC Public Health. 2021;21(1):1–17. PMID: 34001026. doi: 10.1186/s12889-021-10773-1
- The World Bank. Physicians (per 1,000 people) - India, United Kingdom. World Health Organization’s Global Health Workforce Statistics, OECD, supplemented by country data. [cited 2023 Jan 31]. Available from: https://web.archive.org/web/20230307055138/. https://data.worldbank.org/indicator/SH.MED.PHYS.ZS?locations=IN-GB
- Business Standard. Rs 3 per day: That’s how much India spends for each Indian’s health. 2018 June 23 [cited 2022 Sep 3]. Available from: https://web.archive.org/web/20230307055816/https://www.business-standard.com/article/current-affairs/rs-3-per-day-that-s-how-much-india-spends-for-each-indian-s-health-118062100103_1.html
- Business Standard. Health insurance coverage up in India but not robust yet, says NFHS. 2022 May 13 [cited 2023 May 12]. Available from: http://web.archive.org/web/20230513052840/https://www.business-standard.com/article/current-affairs/health-insurance-coverage-up-in-india-but-not-robust-yet-says-nfhs-122051301517_1.html
- The Commonwealth Fund. India | international health care system profiles. 2020 June 5 [cited 2023 May 12]. Available from: http://web.archive.org/web/20230513053132/https://www.commonwealthfund.org/international-health-policy-center/countries/india
- The World Bank. Poverty and equity brief. South Asia, India; 2020 Apr [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20230307060727/https://databankfiles.worldbank.org/public/ddpext_download/poverty/33EF03BB-9722-4AE2-ABC7-AA2972D68AFE/Global_POVEQ_IND.pdf
- Madhok D India’s billionaires got richer while coronavirus pushed millions of vulnerable people into poverty. CNN Business. 2021 July 06 [cited 2022 Apr 6]. https://web.archive.org/web/20230131201246/https://edition.cnn.com/2021/07/05/economy/ambani-adani-india-covid-billionaires-intl-hnk/index.html
- Office for National Statistics. Healthcare expenditure, UK Health Accounts; 2020 [cited 2023 Jan 1]. Available from: https://web.archive.org/web/20230121212550/https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthcaresystem/bulletins/ukhealthaccounts/2020
- Das J, Daniels B, Ashok M, et al. Two Indias: the structure of primary health care markets in rural Indian villages with implications for policy. Soc Sci Med. 2022;301:112799. doi: 10.1016/j.socscimed.2020.112799
- Das J, Hammer J. Money for nothing: the dire straits of medical practice in Delhi, India. J Dev Econ. 2007 May 1;83(1):1–36. doi: 10.1016/j.jdeveco.2006.05.004
- Woloschuk W, Tarrant M. Do students from rural backgrounds engage in rural family practice more than their urban-raised peers? Med Educ. 2004 Mar;38(3):259–61. PMID: 14996334. doi: 10.1046/j.1365-2923.2004.01764.x
- Brahmapurkar KP, Zodpey SP, Sabde YD, et al. The need to focus on medical education in rural districts of India. Natl Med J India. 2018 May-Jun;31(3):164–168. PMID: 31044766. doi: 10.4103/0970-258X.255761
- Shipman SA, Wendling A, Jones KC, et al. The decline in rural medical students: a growing gap in geographic diversity threatens the rural Physician workforce. Health Aff. 2019 Dec;38(12):2011–2018. PMID: 31794312. doi: 10.1377/hlthaff.2019.00924
- Supe A, Burdick WP. Challenges and issues in medical education in India. Acad Med. 2006 Dec;81(12):1076–80. PMID: 17122473. doi: 10.1097/01.ACM.0000246699.94234.ab
- Amin Z, Burdick WP, Supe A, et al. Relevance of the flexner report to contemporary medical education in south Asia. Acad Med J Assoc Am Med Coll. 2010;85(2):333–339. doi: 10.1097/ACM.0b013e3181c874cb
- Sahai A. Medical education in India: introspection, challenges and reforms–A vision. J Anat Soc India. 2016 Dec 1;65(2):167–74. doi: 10.1016/j.jasi.2017.02.011
- Sood R. Medical education in India. Med Teach. 2008;30(6):585–91. doi: 10.1080/01421590802139823
- Anand AC. Medical education in India: moments of pensive introspection. Trop Gastroenterol. 2009 Jan-Mar;30(1):54–8. PMID: 19624093.
- Careers 360. MBBS admission in India- courses, colleges, fee, seats, duration, eligibility. [cited 2023 Jan 1]. Available from: https://web.archive.org/web/20220126194112/https://medicine.careers360.com/articles/mbbs-admission-in-india
- National Medical Commission. P.G. Medical Education Regulations. 2000 [cited 2023 Jan 1]. https://web.archive.org/web/20221009164723/https://www.nmc.org.in/rules-regulations/p-g-medical-education-regulations-2000/
- Singh T, Gupta P, Dhir SK. Medical education scenario in India over the years. Indian Pediatr. 2023;60(4):308–312. doi: 10.1007/s13312-023-2864-1
- Institute of Medicine (U.S.) Division of health sciences policy. Medical education and societal needs: a planning report for the health professions. Washington (D.C.): National Academies Press (U.S.); 1983 [cited 2023 Jan 1]. Chapter 7, MEDICAL SCHOOL ADMISSIONS. Available from: https://web.archive.org/web/20210507011744/https://www.ncbi.nlm.nih.gov/books/NBK217679/
- Medical Schools Council. Entry requirements for U.K. medical schools. [cited 2023 Jan 1]. Available from: https://web.archive.org/web/20220725211544/https://www.medschools.ac.uk/media/2877/entry-requirements-document-2022-digital.pdf
- The Times of India. Over 20 lakh applicants for NEET UG 2023. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20230426191059/https://timesofindia.indiatimes.com/education/news/over-20-lakh-applicants-for-neet-ug-2023/articleshow/99621365.cms
- National Medical Commission. List of colleges teaching MBBS. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20231121001604/https://www.nmc.org.in/information-desk/for-students-to-study-in-india/list-of-college-teaching-mbbs/
- The Medic Portal. UCAS application stats for 2023 entry medicine. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20230323200550/https://www.themedicportal.com/blog/ucas-application-stats-for-2023-entry-medicine/
- NRMP. Results and Data. Main residency match. National Resident Matching Program. 2020 [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20220421054620/https://www.nrmp.org/wp-content/uploads/2021/12/MM_Results_and-Data_2020-rev.pdf
- GMC. Recent pass rates for PLAB 1 and PLAB 2. General Medical Council [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20180714082502/https://www.gmc-uk.org/registration-and-licensing/join-the-register/plab/recent-pass-rates-for-plab-1-and-plab-2
- Shiksha Internal Authors. NEET PG result 2020: statistics released by N.B.E. suggest 89,549 qualified the exam. 2020 Jan 31 [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20220515173235/https://www.shiksha.com/medicine-health-sciences/articles/neet-pg-result-2020-statistics-released-by-nbe-suggest-89-549-qualified-the-exam-blogId-29943
- Ozair A, Bhat V, Detchou DKE. The US residency selection process after the United States medical licensing examination step 1 Pass/Fail change: overview for applicants and educators. JMIR Med Educ. 2023 Jan 6;9:e37069. doi: 10.2196/37069
- The Atlantic. Where pseudoscience is spreading. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20230603182446/https://www.theatlantic.com/international/archive/2020/08/amitabh-bachchan-india-coronavirus/615310/
- Statista. Gini coefficient for India in selected years from 1983 to 2019. [cited 2023 Nov 22]. Available form: https://web.archive.org/web/20231122173600/https://www.statista.com/statistics/1273096/india-gini-index/
- Gao H, Liu W, Nie NJ. Who, what and where (WWW) problems in scientific communities. Sci Eng Ethics. 2018;24(1):327–330. doi: 10.1007/s11948-016-9843-5
- Thiriveedhi S, Myla A, Priya CV, et al. A study on the assessment of anxiety and its effects on students taking the national eligibility cum entrance test for undergraduates (NEET-UG) 2020. Cureus. 2023 Aug 28;15(8):e44240. doi: 10.7759/cureus.44240
- Collegedunia. College Predictor For NEET 2023. [cited 2023 Jan 1]. https://web.archive.org/web/20230307064307/https://collegedunia.com/neet-college-predictor
- Bal AM. Medicine, merit, money and caste: the complexity of medical education in India. Indian J Med Ethics. 2010;7(1):25–28. doi: 10.20529/IJME.2010.009
- Qadeer I. The real crisis in medical education. Indian J Med Ethics. 2006 Jul;3(3):95–96. doi: 10.20529/IJME.2006.036
- Brazeau CM, Schroeder R, Rovi S, et al. Relationship between medical student service and empathy. Acad Med. 2011 Oct;86(10 Suppl):S42–5. PMID: 21955767. doi: 10.1097/ACM.0b013e31822a6ae0
- Hojat M. Assessments of empathy in medical school admissions: what additional evidence is needed? Int J Med Educ. 2014 Jan 11;5:7–10. PMID: 25341204; PMCID: PMC4207176. DOI:10.5116/ijme.52b7.5294
- Nicholson S. The benefits of aptitude testing for selecting medical students. BMJ. 2005 Sep 10;331(7516):559–60. PMID: 16150767; PMCID: PMC1200592. doi: 10.1136/bmj.331.7516.559
- Shiksha Internal Authors. National Education Boards in India – CBSE, CISCE, NIOS. [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20230227222719/https://www.shiksha.com/education-boards-in-india-chp
- Allen. Pre-Nurture & Career Foundation [PNCF]: courses. Kota: Allen Career Institute; [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20220410065333/https://www.allen.ac.in/pncf/kota/2020-21/pre-nurture-career-foundation-coaching/courses-for-pncf-2020-21.asp
- Allen. NEET(U.G.) 2019. Allen Career Institute. [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20220410065440/allen.ac.in/results/neet-ug-2019-result-all-india-toppers.asp
- Allen. AIIMS 2019 Result. Allen Career Institute. [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20221004044826/https://www.allen.ac.in/apps/selection-results/yesteryears/default.asp?e=AIIMS&y=2019&c=
- Collegedunia. Dummy school vs regular school vs integrated school - which one to choose? [cited 2023 Jan 1]. Available from: https://web.archive.org/web/20230307064508/https://collegedunia.com/social/356-dummy-school-vs-regular-school-vs-integrated-school-which-one-to-choose
- Mohamed IS Data on medical admissions proves NEET is anti-poor, say judges. The Hindu. 2019 Nov 05 [cited 2022 Apr 6]. Available from: https://web/20230307064832/https://www.thehindu.com/news/cities/chennai/data-on-medical-admissions-proves-neet-is-anti-poor-say-judges/article29882825.ece
- NITI Aayog. Education change in rankings. [cited 2023 Jan 1]. Available from: https://web.archive.org/web/20230307064954/https://social.niti.gov.in/edu-new-ranking%20
- Allen. Pre-Medical NEET (U.G.), AIIMS: Courses. AIPMT (NEET-UG) & AIIMS Courses & Fee Structure For Session 2023-24. Allen Career Institute: Kota; [cited 2023 Mar 7]. Available from: https://web.archive.org/web/20221204023416/https://www.allen.ac.in/kota/neet-ug-aiims-coaching.asp
- Business standard. India’s per capita income remains below pre-Covid level in 2021-22. 2022 Jun 1 [cited 2022 Sep 3]. Available from: https://web.archive.org/web/20221024095531/https://www.business-standard.com/article/economy-policy/india-s-per-capita-income-remains-below-pre-covid-level-in-2021-22-122053101435_1.html
- Allen. Courses for pre-medical NEET (UG). [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20231103182659/https://www.allen.ac.in/kochi/2023-24/neet-ug-aiims-coaching/courses-for-neet-ug-aiims-2023-24.asp
- Careers 360. Best NEET coaching institutes in India with fees structure -coachings, tutorials. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20230320125435/https://medicine.careers360.com/articles/best-neet-coaching-institutes-in-india-with-fees-structure
- Physics Wallah. Physics wallah fee structure, courses fee for all offline and online classes. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20231103183924/https://www.pw.live/exams/vidyapeeth/physics-wallah-fee-structure/
- Allen. Classroom courses for PRE-MEDICAL NEET (UG). [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20231103185152/https://www.allen.ac.in/ujjain/2023-24/neet-ug-aiims-coaching/courses-for-neet-ug-aiims-2023-24.asp?course=enth-off
- Byju’s. Aakash BYJU’S live online classroom program. [cited 2023 Nov 22]. Availble from: https://web.archive.org/web/20230406183037/https://shop.byjus.com/collections/byjus-online-classroom-program
- Unacademy. NEET UG subscription. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20230529052609/https://unacademy.com/goal/neet-ug/YOTUH/subscribe?plan_type=iconic
- Resonance. Samarth. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20230609143617/https://www.resonance.ac.in/courses/Samarth.aspx.
- Resonance. Resonance FEE Structure For NEET Courses (2024-25). [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20231104031336/https://www.resonance.ac.in/courses/fee-structure-neet.aspx
- Margshree. NEET Coaching Fees Structure in Delhi NCR. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20230824121221/https://margshree.com/neet-course/neet-course-fee/
- Kini SB. A serious compromise in the quality of medical education in India by some Recently established private medical colleges. Online J Health Allied Scs. 2022;21(4):12. Available from: https://www.ojhas.org/issue84/2022-4-12.html
- Mahal A, Mohanan M. Growth of private medical education in India. Med Educ. 2006 Oct;40(10):1009–11. PMID: 16987192. doi: 10.1111/j.1365-2929.2006.02560.x
- Sabde Y, Diwan V, De Costa A, et al. Mapping the rapid expansion of India’s medical education sector: planning for the future. BMC Med Educ. 2014 Dec 17;14:266. PMID: 25515419; PMCID: PMC4302536. 10.1186/s12909-014-0266-1
- Babu TA, Joseph NM, Sharmila V. Academic dishonesty among undergraduates from private medical schools in India. Are we on the right track? Med Teach. 2011;33(9):759–61. Epub 2011 May 19. PMID: 21592022. doi: 10.3109/0142159X.2011.576717
- Medical Counselling Committee. Institute’s Information. [cited 2022 Sep 3]. Available from: https://web.archive.org/web/20221018070436/https://mcc.nic.in/UGCounselling/Home/GetInstituteProfile
- The Print. MBBS seats rose 110% in 10 yrs, number of medical aspirants up by over 14 lakh, govt tells LS. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20230807200033/https://theprint.in/india/education/mbbs-seats-rose-110-in-10-yrs-number-of-medical-aspirants-up-by-over-14-lakh-govt-tells-ls/1703978/
- The Indian Express. The prohibitive cost of private medical education in India. 2022 Mar 3 [cited 2022 Sep 03]. Available from: https://web.archive.org/web/20220308195048/https://www.newindianexpress.com/opinions/editorials/2022/mar/03/the-prohibitive-cost-of-private-medical-education-in-india-2425697.html
- Bansal RK. Private medical education takes off in India. Lancet. 2003 May 17;361(9370):1748–9.
- Singh T. Commercialisation of medical education–a review of capitation fee colleges. J Indian Med Assoc. 1994 Sep;92(9):301–303. PMID: 7814906.
- Joy SRR, Vijayan S, Ugargol A. Mushrooming of private medical schools in india, the present student profile and cost of medical education and its impact On equity, health care accessibility, cost and perceived quality of health care(2007) IHEA 2007 6th world congress: explorations in health economics paper. Available at SSRN: or 10.2139/ssrn.992143http://ssrn.com/abstract=992143
- The Times of India. Fee in govt medical colleges goes op by up to 400%. 2018 Jul 29 [cited 2022 Apr 6]. https://web.archive.org/web/20220913040955/https://timesofindia.indiatimes.com/city/ahmedabad/fee-in-govt-medical-colleges-goes-up-by-up-to-400/articleshow/65181424.cms
- Medical Dialogues. Punjab Govt criticised for 75% MBBS fee hike in GMCs. 2022 Sep 10 [cited 2022 Apr 6]. https://web.archive.org/web/20220410065820/https://medicaldialogues.in/state-news/punjab/punjab-govt-criticised-for-75-percent-mbbs-fee-hike-at-gmcs-69417
- The Times of India. Haryana government hikes MBBS fee to rs 40 lakh. 2022 Nov 09 [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20220410065906/https://timesofindia.indiatimes.com/city/chandigarh/hry-govt-hikes-mbbs-fee-to-rs-40l/articleshow/79118518.cms
- Harrison’s Principles Of Internal Medicine, Twentieth Edition (Vol.1 & Vol.2). Amazon [cited 2022 Apr 6]. https://web.archive.org/web/20220410070025/https://www.amazon.in/Harrisons-Principles-Internal-Medicine-Twentieth/dp/1259644030
- Collegedunia. NEET PG 2022 exam pattern, marking scheme, & distribution of questions. [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20220410070127/https://collegedunia.com/exams/neet-pg/exam-pattern.
- INI-CET. Institute of national ImportanceCombined entrance test (INI-CET)for PG courses. Available from: https://web.archive.org/web/20231122184928/https://docs.aiimsexams.ac.in/sites/1_PROSPECTUS%20PART-A%20INI-CET%20JANUARY%202024%20SESSION-FINAL.pdf
- Shiksha. NEET PG Seats in India: Check State-wise List Here!. [cited 2023 Jan 1]. Available from: https://web.archive.org/web/20230131084539/https://www.shiksha.com/medicine-health-sciences/articles/neet-pg-seats-in-india-blogId-62867
- Medical Dialogues. Around 1.8 lakh candidates appeared for NEET-PG 2022. [cited 2023 Jan 1]. Available from: https://web.archive.org/web/20220628091430/https://medicaldialogues.in/news/education/around-18-lakh-candidates-appeared-for-neet-pg-2022-93387
- Arvind A, Amit T, Ashish G. Review of postgraduate medical entrance examination. 9th ed. Vol. 2. In: Pathology. Gorakhpur: Pulse Publications; 2013. p. 350–355.
- Delhi Academy of Medical Sciences. Achievement MD/MS courses. [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20221202065506/https://www.damsdelhi.com/topper-zone
- Collegedunia. DR. Bhatia medical coaching institute (NEET-PG, AIMS-PG). [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20231103191720/https://collegedunia.com/institute/108-dr-bhatia-medical-coaching-institute-neet-pg-aims-pg-new-delhi
- Egurukul. Select your package & plan. [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20230307093630/https://www.egurukulapp.com/package/packagePlan
- Prepladder. Dream Pack 4.0. [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20221209094008/https://www.prepladder.com/courses/medical-pg/plan
- Marrow. The gold standard for NEET PG - NEXT. [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20230307094628/https://www.marrow.com/pro?source=google
- Unacademy. NEET PG: select a subscription that suits you. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20231122191311/https://unacademy.com/goal/neet-pg-live/SDDOC/subscribe?plan_type=iconic
- Speed Institute. NEXT PG Courses. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20231103193215/https://www.speedmedicalcentre.com/neet-pg-coaching/pg-preparation-courses/
- Belur R RGUHS plans coaching for P.G. medical entrance from next year. Deccan Herald. D.H. News Service; 2020 [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20220410071542/https://www.deccanherald.com/state/karnataka-districts/rguhs-plans-coaching-for-pg-medical-entrance-from-next-year-809898.html
- Shiksha Internal Authors. 687 MD colleges in India. [cites 2022 Apr 6]. Available from: https://web.archive.org/web/20230131081453/https://www.shiksha.com/medicine-health-sciences/colleges/md-colleges-india
- The New Indian Express. Act against private colleges not paying PG students: medicos tell NMC; [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20230829053723/https://www.newindianexpress.com/nation/2023/aug/29/act-against-private-colleges-not-paying-pg-students-medicos-tell-nmc-2609669.html
- The New Indian Express. Red tape? T.N. govt P.G. doctors’ salary gets delayed. [cited 2023 Jan 1]. https://web.archive.org/web/20221027203232/https://www.newindianexpress.com/states/tamil-nadu/2022/oct/17/red-tape-tn-govt-pg-doctors-salary-gets-delayed–2508943.html
- Wikipedia. Internship (Medicine). [cited 2023 Jan 1]. https://web.archive.org/web/20230224235640/https://en.wikipedia.org/wiki/Internship_(medicine)
- Wikipedia. Medical education in India. [cited 2023 Jan 1]. https://web.archive.org/web/20230130155248/https://en.wikipedia.org/wiki/Medical_education_in_India
- National Medical Commission. Public Notice. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20230604045541/https://www.nmc.org.in/MCIRest/open/getDocument?path=/Documents/Public/Portal/LatestNews/Public%20Notice%20-%20NExT%20Regulations.pdf
- National Medical Commission. Public Notice. [cited 2023 Jan 1]. https://web.archive.org/web/20230112054933/https://www.nmc.org.in/MCIRest/open/getDocument?path=/Documents/Public/Portal/LatestNews/Public%20Notice%20-%20NExT%20Regulations.pdf
- Ozair A, Bhat V, Detchou DKE. The U.S. Residency selection process after the United States medical licensing examination step 1 pass/fail change: overview for applicants and educators. JMIR Med Educ. 2023;9:e37069. PMID: 36607718. doi: 10.2196/37069
- Burk-Rafel J, Santen SA, Purkiss J. Study behaviors and USMLE step 1 performance: implications of a student self-directed parallel curriculum. Acad Med. 2017;92(11S):S67–S74. doi: 10.1097/ACM.0000000000001916
- USMLE. Change to pass/fail score reporting for step 1. [cited 2022 Mar 20]. https://web.archive.org/web/20230214162507/https://www.usmle.org/usmle-step-1-transition-passfail-only-score-reporting
- Kaplan. Clinical skills prep: realistic practice, real results. [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20230307100430/https://www.kaptest.com/usmle-step-2cs
- Samson Clinical Courses. Welcome to PLAB 2 section. [cited 2022 Apr 6]. Available from: https://web.archive.org/web/20221204151952/https://samsoncourses.com/plab-2/
- Youngclaus J, Roskovensky L. An updated look at the economic diversity of U.S. Medical students. AAMC Analysis In Brief. 2018;18(5):1–3 [cited 2022 April 6]. Available from: https://www.aamc.org/system/files/reports/1/october2018anupdatedlookattheeconomicdiversityofu.s.medicalstud.pdf:https://web.archive.org/web/20220805231754/
- Pisaniello MS, Asahina AT, Bacchi S, et al. Effect of medical student debt on mental health, academic performance and specialty choice: a systematic review. BMJ Open. 2019;9(7):e029980. doi: 10.1136/bmjopen-2019-029980
- U.S. Census Bureau. Income and poverty in the United States: 2020. 2021 Sep 14 [cited 2022 Sep 3]. https://web.archive.org/web/20230226154717/https://www.census.gov/library/publications/2021/demo/p60-273.html
- Nguyen M, Desai MM, Fancher TL, et al. Temporal trends in childhood household income among applicants and matriculants to Medical School and the likelihood of acceptance by income, 2014-2019. JAMA. 2023 May 11;329(21): 1882. Epub ahead of print. PMID: 37166785. 10.1001/jama.2023.5654.
- Guevara JP, Wade R, Aysola J. Racial and ethnic diversity at medical schools - why Aren’t we there yet? N Engl J Med. 2021;385(19):1732–1734. doi: 10.1056/NEJMp2105578
- Karan A, Negandhi H, Hussain S, et al. Size, composition and distribution of health workforce in India: why, and where to invest? Hum Resour Health. 2021 Mar 22;19(1):39. PMID: 33752675; PMCID: PMC7983088. doi: 10.1186/s12960-021-00575-2
- Sharma DC. India still struggles with rural doctor shortages. Lancet. 2015 Dec 12;386(10011):2381–2. PMID: 26700521. 10.1016/S0140-6736(15)01231-3
- Goel S, Angeli F, Dhirar N, et al. Factors affecting medical students’ interests in working in rural areas in north india-A qualitative inquiry.PloS One. 2019 Jan 10;14(1):e0210251. doi: 10.1371/journal.pone.0210251
- Mohammadiaghdam N, Doshmangir L, Babaie J, et al. Determining factors in the retention of physicians in rural and underdeveloped areas: a systematic review. BMC Fam Pract. 2020 Oct 23;21(1):216. PMID: 33097002; PMCID: PMC7585284. doi: 10.1186/s12875-020-01279-7
- Rao M, Rao KD, Kumar AK, et al. Human resources for health in India. Lancet. 2011 Feb 12;377(9765):587–598. Epub 2011 Jan 10. PMID: 21227499. 10.1016/S0140-6736(10)61888-0
- Sudhinaraset M, Ingram M, Lofthouse HK, et al. What is the role of informal healthcare providers in developing countries? A systematic review. PloS One. 2013;8(2):e54978. doi: 10.1371/journal.pone.0054978
- Gautham M, Shyamprasad KM, Singh R, et al. Informal rural healthcare providers in North and South India. Health Policy Plan. 2014;29(suppl 1):i20–i29. doi: 10.1093/heapol/czt050
- Kanjilal B, Mondal S, Samanta T, et al. “A parallel health care market: Rural medical practitioners in West Bengal, India” (Future Health Systems Research Brief No. 2). Institute of Health Management Research, 2007.
- Das J, Chowdhury A, Hussam R, et al. The impact of training informal health care providers in India: a randomized controlled trial. Science.2016 Oct 7;354(6308):aaf7384. doi: 10.1126/science.aaf7384
- Varghese J. The new rural doctor: qualified quack or appropriate healthcare provider? Indian J Med Ethics. 2010;7(2):70–72. doi: 10.20529/IJME.2010.028
- Launcher A. State-wise medical pg bond details for neet pg 2021-22. [cited 2022 Sept 3]. https://web.archive.org/web/20221001010528/https://www.admissionlauncher.com/medical-pg-bond-in-different-state/
- Mohan P, Kumar R. Strengthening primary care in rural India: lessons from Indian and global evidence and experience. J Family Med Prim Care. 2019 Jul;8(7):2169–2172. PMID: 31463225; PMCID: PMC6691438. doi: 10.4103/jfmpc.jfmpc_426_19
- The World Bank. Current health expenditure (% of G.D.P.). 2022 January 30 [cited 2022 Aug 6]. https://web.archive.org/web/20230302070941/https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS
- Leaune E, Rey-Cadilhac V, Oufker S, et al. Medical students attitudes toward and intention to work with the underserved: a systematic review and meta-analysis. BMC Med Educ. 2021 Feb 24;21(1):129. PMID: 33627102; PMCID: PMC7905612. doi: 10.1186/s12909-021-02517-x
- Morris CG, Johnson B, Kim S, et al. Training family physicians in community health centers: a health workforce solution. Fam Med. 2008 Apr;40(4):271–6. PMID: 18382840.
- Huntington I, Shrestha S, Reich NG, et al. Career intentions of medical students in the setting of Nepal’s rapidly expanding private medical education system. Health Policy Plan. 2012;27(5):417–428. doi: 10.1093/heapol/czr052
- Wibulpolprasert S, Pengpaibon P. Integrated strategies to tackle the inequitable distribution of doctors in Thailand: four decades of experience. Hum Resour Health. 2003 Nov 25;1(1):12. PMID: 14641940; PMCID: PMC317381. doi: 10.1186/1478-4491-1-12
- The New York Times. Surprise gift: free tuition for all N.Y.U. Medical students. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20230726162632/https://www.nytimes.com/2018/08/16/nyregion/nyu-free-tuition-medical-school.html
- NYU Langone Health. Affordability & financial aid for MD students. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20231029095043/https://med.nyu.edu/education/md-degree/affordability-financial-aid
- CBSNews. How the NYU School of Medicine is going tuition-free. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20230128040300/https://www.cbsnews.com/news/tuition-free-medical-school-how-the-nyu-school-of-medicine-is-going-tuition-free-60-minutes-2019-12-29/
- SMSIMSR. In rural for rural. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20230326153747/https://smsimsr.org/
- Business Standard. SMSIMSR focuses on rural medical education, increased enrollment for girls. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20230429074146/https://www.business-standard.com/education/news/simsr-outs-focus-on-rural-medical-education-increased-enrollment-for-girls-123033000947_1.html
- The Hindu. All free medical education seats at SMSIMSR college filled up. [cited 2023 Nov 22]. Available from: https://web.archive.org/web/20231010023508/https://www.thehindu.com/news/national/karnataka/all-free-medical-education-seats-at-smsimsr-college-filled-up/article67369610.ece
- Igumbor EU, Del Río A, Buso DL. Training medical students in the community - memoirs and reflections of the University of Transkei medical School. Med Educ Online. 2006 Dec;11(1):4605. PMID: 28253780. doi: 10.3402/meo.v11i.4605
- World Health Organization. Report on the WHO/PEPFAR planning meeting on scaling up nursing and medical education. Geneva: WHO. 2009 [cited 2023 Jan 1]. Available from: https://www.aspeninstitute.org/wp-content/uploads/files/content/images/WHO.PEPFAR_ScalingUpPlanningRept.pdf
- Takeshita J, Wang S, Loren AW, et al. Association of racial/ethnic and gender concordance between patients and physicians with patient experience ratings. JAMA Netw Open. 2020;3(11):e2024583. doi: 10.1001/jamanetworkopen.2020.24583
- Poole KG Jr. ‘I want a doctor who looks like me’: the dilemma of race-based requests. Ccjm. 2020 May;87(5):268–270. PMID: 32357980. doi: 10.3949/ccjm.87a.19110
- Gomez LE, Bernet P. Diversity improves performance and outcomes. J Natl Med Assoc. 2019 Aug;111(4):383–392. Epub 2019 Feb 11. PMID: 30765101. doi: 10.1016/j.jnma.2019.01.006
- Diwan V, Minj C, Chhari N, et al. Indian medical students in public and private sector medical schools: are motivations and career aspirations different? – studies from Madhya Pradesh, India.BMC Med Educ. 2013 Sep 15;13(1):127. doi: 10.1186/1472-6920-13-127
- Ozair A, Singh KK. Delivering high-quality, Equitable Care in India: an ethically-resilient framework for healthcare innovation after COVID-19. Front Public Health. 2021 Feb 18;9: 640598. PMID: 33681137; PMCID: PMC7935506. doi: 10.3389/fpubh.2021.640598

