ABSTRACT
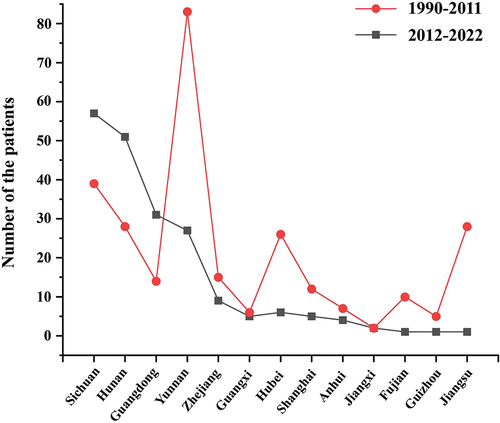
Histoplasmosis is a systemic mycosis caused by the dimorphic fungus in the genus Histoplasma. Histoplasmosis is overlooked in China. This study aims to provide an epidemiological and clinical update on histoplasmosis in China by literature review. We reviewed cases of histoplasmosis reported in recent 11 years and described a case of histoplasmosis-triggered hemophagocytic lymphohistiocytosis (HLH) in an immunocompetent patient. A total of 225 cases of histoplasmosis diagnosed in China between 2012 and 2022 were involved in this study, compared with 300 cases reviewed from 1990 to 2011, an increasing number of cases of histoplasmosis have been diagnosed in the last 11 years. The majority of cases of histoplasmosis were autochthonous cases, mainly from provinces Sichuan (56/225, 24.9%), Hunan (50/225, 22.2%), Guangdong (31/225, 13.8%), and Yunnan (24/225, 10.7%). Higher incidence (52.5%, 53/99) of histoplasmosis occurred in immunocompetent patients which is similar to those from the previous 21 years, and the prevalence of the disease did not vary highly over time. Of note, the number of histoplasmosis cases is increasing, and the geographic distribution is shifting southwards over time. Improved awareness is critically important for informing clinical practice in China.
1. Introduction
Histoplasmosis is a worldwide-distributed systemic mycosis caused by Histoplasma species, a thermally dimorphic fungi with a specific ecological niche. Its clinical manifestations can range from respiratory infections in immunocompetent individuals to invasive disseminated histoplasmosis in immunosuppressed patients (Benedict and Mody Citation2016). Histoplasmosis is highly endemic in regions of North, Central, and South America, as well as being reported in parts of Asia and Africa (Bahr et al. Citation2015; Thompson et al. Citation2021), but is probably more widespread than previously thought (Antinori Citation2014). However, the real global burden of histoplasmosis remains unknown due to its non-specific clinical symptoms and radiological findings, whose accurate diagnosis is still challenging (Adenis et al. Citation2014; Araúz and Papineni Citation2021).
Histoplasmosis is sorely neglected in China by epidemiologists, researchers, and clinicians, often with fundamental epidemiologic questions still unanswered. Sporadic cases have been reported (Antinori et al. Citation2021; Ocansey et al. Citation2022) since the first case of histoplasmosis was reported in 1958 (Lan et al. Citation2010). A Chinese group has reviewed 300 cases of histoplasmosis reported during 1990 to 2011 in China (Pan et al. Citation2013) showing a strong association with the Yangtze River flows. Most of the patients had autochthonous infections. A Chinese survey of histoplasmin skin test reactivity among 735 Chinese volunteers with no history of living abroad indicated that the positive rate of histoplasm in skin reaction in Southeast subjects is higher than that in the Northwest which supported the Pan’s study (Zhao et al. Citation2001). However, epidemiological and clinical data on this disease remain limited due to the lack of comprehensive surveillance for histoplasmosis in China.
This study retrospectively summarises recent 11 years cases of histoplasmosis reported both in English and Chinese about its epidemiological and clinical characteristics, in comparison with previous review data from 1990 to 2011 (Pan et al. Citation2013), to provide the updated data on prevalence and geographic distribution of histoplasmosis in China, as well as a new case of progressive disseminated histoplasmosis triggered hemophagocytic lymphohistiocytosis in an immunocompetent patient from China.
2. Materials and methods
2.1. Literature review
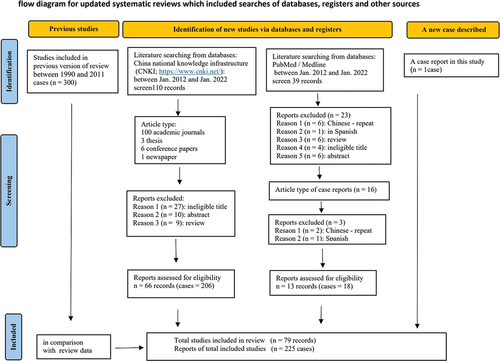
A literature search was carried out in databases including PubMed/Medline, Scopus, Web of Science, Embase, and China National Knowledge Infrastructure (CNKI; https://www.cnki.net/). The English and Chinese language (CNKI database) literature between January 2012 and December 2021 was reviewed using search terms “China”, “Chinese”, “histoplasmosis”, and “Histoplasma spp.”. The literature search identified 79 published articles about cases of human histoplasmosis including 66 articles in Chinese and 13 in English (Stable 1).
2.2. Eligibility criteria for patients’ inclusion
Patients were diagnosed with histoplasmosis based on a global guideline for the diagnosis and management of endemic mycoses (Thompson et al. Citation2021) in China. Publications were considered only with individual case reports, and case series. The cases included travel-related, and autochthonous cases.
2.3. Data collection
The following information was extracted from each article: author, year, language, country of exposure, number of cases, patients’ information (age, gender, occupation, and affected organs), systemic antifungal therapy, and outcomes.
3. Result
3.1. Case presentation
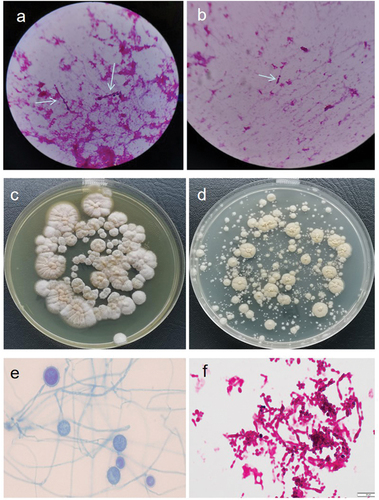
A 44-year-old Chinese male living in Yunnan province was admitted to the emergency department in our hospital on NaN Invalid Date with an intermittent high fever for two months. The patient had worked in Kenya for two years and he started fever after four months back from Kenya. He received empiric treatment with antibiotics at the local hospital for two months, however, fever persisted, while the number of blood platelets reduced to the critical value (<20 × 109/L). Therefore, the patient came to our hospital for further treatment. He denied any medical history. He had experience of eating wild animals (including paguma larvata, pheasant, etc.) during his stay in Kenya. A physical examination at the time of admission revealed a high fever (39.8 °C), hepatosplenomegaly, scleral yellow staining. The patient was suffering from fatigue, progressive weightless >6 kg within two months. His white blood cell (WBC) count was 13.21 × 109/L (83% neutrophils), red blood cell count (RBC) 2.83 × 1012/L, haemoglobin (Hb) level 83 g/L and platelet (PLT) count 1 × 109/L. Albumin 17.8 g/L, total bilirubin 55.4 μmol/L, direct bilirubin 40.8 μmol/L. Aspartate and alanine aminotransferase levels were normal. Activated partial thromboplastin time (APTT) and prothrombin time (PT) were prolonged (42.6 seconds and 14.5 seconds, respectively). The serum procalcitonin (PCT) and C-reactive protein (CRP) were elevated (3.342 ng/mL and 71.89 mg/L, respectively). Serologic tests for syphilis, human immunodeficiency virus, hepatitis B and C, and T-spot test for tuberculosis were negative. A CT scan of chest and abdomen showed mild inflammation in the lower lobes of bilateral lungs, and the liver was slightly enlarged (). The sputum culture showed no positive result. However, Wright-stained bone marrow aspirates revealed intracellular oval or spherical yeast-like cells, which was highly suggestive of H. capsulatum (), with normal number and classification of megakaryocytes. Although the culturing with bone marrow sample was negative for fungal and bacteria in 5 days incubation, disseminated histoplasmosis was diagnosed based on clinical presentation and visible intracellular yeast-like cells in bone marrow smear. Amphotericin B (30 mg, Qd, i.e.) was administered against fungal infection, meanwhile, cryoprecipitation and platelet transfusion were given to improve the coagulation function. Nevertheless, after 7 days of treatment, the fever persisted, and blood tests showed pancytopenia, WBC 2.22 × 109/L, Hb 63 g/L, PLT 4 × 109/L. APTT and PT prolonged more to 48.6 seconds and 17.2 seconds, respectively. His serum ferritin and sCD25 were elevated to 2,545 μg/L and 35,854 pg/mL, respectively. Then, a second bone marrow puncture was performed, and a bone marrow examination revealed lots of histiocytes phagocytosing red blood cells, erythroblasts, and platelets along with many intrahistiocytic, and extracellular H. capsulatum which indicated HLH secondary to histoplasmosis. HLH was diagnosed. However, the culture of the bone marrow aspirate provided negative results after 16 days of incubation. We did a routine check by smear with a negative culture specimen. Interestingly, yeast-like cells and hyphae were seen in the smears (). which were compatible with Histoplasma spp., then we inoculated the culture specimen on the Sabouraud Dextrose Agar (SDA), incubated at 28 °C and 37 °C, respectively, in 9 days later, it appeared cottony white colonies under culture condition at 28 °C and a yeast-like colony at 37 °C (). Microscopic examination showed tuberculate macroconidia and the septated hyphae, and budding cells and pseudohyphae under microscopic (). The isolate was identified using PCR by amplifying the ITS1–4 gene, and four sets of specific primers (ARF, H-antigen, OLE, M-antigen) as described previously (Rodrigues et al. Citation2020), the sequences were blasted in NCBI (https://www.ncbi.nlm.nih.gov/). The isolate was identified as H. capsulatum. The sequences were deposited in the GenBank under the accession number ON244035 (ITS), ON478356 (ARF), ON478359 (H-antigen), ON478358 (OLE), ON478357 (M-antigen), which had 99% identity with the Ajellomyces capsulatum isolate UAMH 7141. The patient completed the 4-week course of AMB (30 mg, Qd, i.v) and changed to oral itraconazole (200 mg, Bid), which led to the rapid disappearance of fever, with the normal blood test indicators. He was discharged with a prescription of itraconazole 200 mg twice daily for 12 months, and followed up for 1 year, no evidence of relapse was noted.
Figure 1. A CT scan of chest and abdomen on the day of admission. A mild inflammation was seen in the lower lobes of bilateral lungs, and the liver was slightly enlarged.
Figure 2. Histoplasma capsulatum (numerous, capsulated yeast cells) of phagocyte cells (arrow) in bone marrow smear (Wright’s staining, magnification 1,000×).
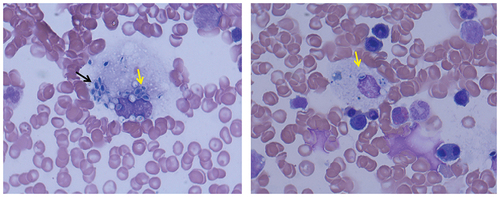
Figure 3. (a, b) Yeast-like spores and hyphae (with an arrow, gram staining, magnification 1,000×) under microscopy with bone marrow cultured at 37 °C in 16 days. (c, d) Colonies grown at 28 °C and 37 °C with bone marrow bone cultured in 16 days; (c) White, short villous and filamentous colonies; (d) Yeast-like colonies. (e, f) Fungal morphology under microscopy by taking colonies, respectively; (e) A filamentous form with tuberculate macroconidia on the septate hyphae (lactic acid phenol cotton blue staining); (f) Yeast-like fungus, budding cells with pseudohyphae (gram staining).
3.2. Summary of the literature
The literature search identified 79 articles about cases of human histoplasmosis both in English and Chinese from China ().
A total of 225 cases of histoplasmosis diagnosed in China between year 2012 and 2022 were involved in this study, compared with 300 cases reviewed from year 1990–2011.
3.3. Regional distribution
A total of 225 cases of histoplasmosis were diagnosed in China between 2012 and 2022 including our case involved in this study. As shown in , the 225 patients (162 males, 72.0%) were with a median age of 39.2 years (range 6 months to 75 years old). Only 6.2% (14/225) of the patients were possibly imported cases with travelling history, in contrast, 93.8% (211/225) of the patients had never travelled outside of China, and the most of the cases (71.6%, 161/225) were from four provinces, namely Sichuan (56/225, 24.9%), Hunan (50/225, 22.2%), Guangdong (31/225, 13.8%) and Yunnan (24/225, 10.7%).
Table 1. The regional distribution of 225 patients diagnosed as histoplasmosis from 2012 to 2022 in China.
3.4. Clinical characteristics
Among the 225 patients included in this study, 23.5% (53/225) patients were immunocompetent; 9.3% (21/225) were patients with HIV; 4.4% (10/225) with other immunocompromise disease; 6.7% (15/225) with underlying disease, however, nearly half (111/225) of the patients did not describe their immune conditions. Disseminated histoplasmosis (DH) was diagnosed with 178 in 225 (79.2%) cases; the remaining 47 patients presented with chronic pulmonary (41/225, 18.2%), gastrointestinal infection (5/225, 2.2%), and oropharynx infection (1, 0.4%). The most common symptoms were fever (116/225, 51.6%), hepatosplenomegaly (90/225, 40.0%), respiratory symptoms (74/225, 32.9%), digestive tract symptoms (53/225, 23.6%), and lymphadenopathy (41/225, 18.2%). Three cases reported complications with HLH ().
Table 2. The clinical characteristics of 225 patients diagnosed as histoplasmosis from 2012 to 2022 in China.
3.5. The diagnosis, treatment, and outcome
The diagnostic work-up varied among the 225 patients: histopathology examination was the main method for diagnosis (94 cases, 41.8%); followed by microscopic visualisation of the fungus with bone marrow smear (62 cases, 27.6%); bone marrow smear + histopathology examination (11 cases, 4.9%); urinary or serum Histoplasma antigen (11 cases, 4.9%); culture was available in 34 cases (15.1%); PCR was reported in 8 cases (3.6%) and mNGS was in 2 cases (1.3%). Based on the final diagnosis of the 225 patients, 222 patients were proven as histoplasmosis, and 2 patients were diagnosed as probable histoplasmosis ().
Table 3. The diagnosis, treatment, and outcome of 225 patients diagnosed as histoplasmosis from 2012 to 2022 in China.
A majority of patients were treated with one of the amphotericin B (AMB) formulations including AMB alone (66/225, 29.3%), AMB + itraconazole (46/225, 20.4%) or + fluconazole (11/225, 4.9%), + other azoles (22/225, 9.8%); 9/225 (4%) patients were treated with itraconazole alone; 10/225 (4.4%) cases with operation combined with antifungals; 14 cases did not receive any treatments. Forty-six patient’s treatment was not recorded. Of the 167 patients whose outcomes were recorded, 10 (6.0%) died ().
4. Discussions
We reported a case of disseminated histoplasmosis-triggered HLH in an immunocompetent patient. The initial clinical presentation, mycological examination, and exposure history in this case were suggestive of histoplasmosis. However, poor clinical response to antifungal therapy, and additional findings such as extreme hyperferritinemia and sCD25, critically helped to establish the diagnosis of HLH secondary to disseminated histoplasmosis. Repeating bone marrow biopsy is often needed, as in most cases hemophagocytosis may not be observed in the initial bone marrow aspirate but will become evidence on follow-up evaluation. Antifungal therapy alone might be sufficient because the symptoms of HLH disappeared completely with the progress of antifungal therapy. Jabr et al. (Citation2019) reviewed 65 cases with histoplasmosis-induced HLH and found that most cases had HIV which exhibited immunodeficiency backgrounds, and most patients were relatively young. However, our case occurred in a relatively young (44 years old) but immunocompetent patient. A literature search in PubMed by the end of September 2017 showed that only four cases worldwide (Jabr et al. Citation2019) and two cases in China (Lv et al. Citation2021; Song et al. Citation2021) had been reported the HLH secondary to H. Capsulatum in immunocompetent patients. Therefore, histoplasmosis-associated HLH among immunocompetent patients is a rare complication.
This review summarised 225 cases of histoplasmosis reported from 2012 to 2022 for 11 years, compare with 300 cases reviewed from 1990 to 2011 for 22 years period (). An increasing number of cases of histoplasmosis have been diagnosed in the last 11 years. This could be because of the improved laboratory tests and awareness of clinicians in recent years. A review of cases of histoplasmosis from 1990 to 2011 showed a strong association with the regions along the Yangtze River flows and most of the patients had autochthonous infections (Pan et al. Citation2013). This statement is undoubtedly true but incomplete. shows the geographical distribution of histoplasmosis diagnosed in southern China during 2012–2022 and 1990–2011. Increasing cases in the last 11 years mainly occurred in four provinces, namely, Sichuan (56/225, 24.9%), Hunan (50/225, 22.2%), Guangdong (31/225, 13.8%), and Yunnan (24/225, 10.7%). The number of cases had dropped severely in provinces Yunnan, Hubei, and Jiangsu where are along the Yangtze River flows. Of note, the Guangdong province is in the south, far from the Yangtze River flows where 13.8% of cases were diagnosed. Thus, our results suggest an expanding focus on histoplasmosis to the southern parts of China. Our data also confirmed the skin-test study (Zhao et al. Citation2001) that its geographic range is much broader than it is often appreciated. The Conditions suitable for H. capsulatum have shifted southwards in the past decade, perhaps resulting from a humid and warming climate, anthropogenic land use, and today’s mobile population which in favour for the growth and dispersal of H. capsulatum.
Figure 5. The geographical distribution of histoplasmosis diagnosed in southern China during 2012–2022 compared to those during 1990–2011.
Another important message arising from our review is that only 13 cases of histoplasmosis reported the suspected exposure history, 93.8% (211/225) cases of histoplasmosis were not associated with any disclosed history of travel or residence in areas considered to be endemic for the disease and can, therefore, possibly be classified as autochthonous. These findings are in agreement with data from the previous review that 91.3% of the histoplasmosis cases were definitely acquired within China (Pan et al. Citation2013). This might be due to greater inoculum exposure although most people with histoplasmosis may, in fact, not have clear or memorable exposures to bird or bat droppings.
A higher prevalence of histoplasmosis among immunocompetent individuals (53.5%, 53/99) was observed among 99 cases with clear underly disease descriptions in the literature reviewed (), which is in line with those (49.1%, 85/173) reported in the previous review (Pan et al. Citation2013). Similar prevalence of histoplasmosis among patients with HIV (21/99 vs. 38/173) and patients with OIC (25/99 vs. 45/173) were found when compared with previous review (Pan et al. Citation2013). The conditions suitable for H. capsulatum are changing, leading to a corresponding change in epidemiology in the United States as well. One recent retrospective study of 261 cases conducted in the United States found a higher prevalence of disseminated disease among immunocompetent subjects (33%), although it is still an AIDS-defining illness (Franklin et al. Citation2021). However, Benedict and Mody (Citation2016) reported that histoplasmosis-related hospitalisations have increased over the past decade throughout the United States and are increasingly seen in patients with immunocompromising conditions other than human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS).
The patients’ ages ranged between 6 months to 75 years old and a majority of our cases involved males (63.5%, 162/255) and the male-to-female ratio was 2.6:1 which was similar as previous data (2.4:1) (Pan et al. Citation2013) in China and Europe (2.6:1) (Antinori et al. Citation2021) but lower than that observed in study from Brazil (4:1) (Almeida et al. Citation2019). It is in line with a previous review (Pan et al. Citation2013) that the most common clinical features among the 225 patients were fever (116/225), splenomegaly/hepatomegaly (105/225), and respiratory symptoms (74/225). Gastrointestinal (GI) symptoms and lymphadenopathy have also been noted as frequent symptoms (18%–23.5%) in disseminated diseases. It is worth noting that 23.5% (53/225) of the patients had intestinal histoplasmosis, and 5/225 had localised intestinal histoplasmosis only. Interestingly, HLH was described in two immunocompetent patients in China, which is different from previous studies that HLH was described more frequently among the immunocompromised patients (Nguyen et al. Citation2020; Antinori et al. Citation2021).
Histopathology or direct microscopy is still commonly applied in the Lab diagnosis of Chinese cases in both periods. The most diagnosis among 225 cases was based on histopathology and direct microscopy examination (79%, 177/225). Cultures from clinical samples show poor sensitivity (). Although antigen detection in urine/serum and PCR emerge as valuable adjunctive diagnostic tools, those are not commonly applied in Chinese cases yet due to their expensive cost and are only available in a few laboratories unfortunately.
Amphotericin B (AmB) was as first-line therapy in 86.8% (145/167) of the cases, with good curative effect. It is difficult to evaluate clinical outcomes based on single-case reports and small case series, given that most infected persons are disseminated histoplasmosis, The high proportions of patients who were hospitalised (94%) and died (6%) suggest relatively severe illness for these patients.
However, several limitations should be noted in this review. The data from the literature review does not consider the underreporting of milder cases and underdiagnosed cases, and some incomplete information from the case reports and small case series may have biased our findings. The lack of comprehensive surveillance for these diseases also leaves a gap in our understanding of their true burden in China.
In conclusion, our evidence suggests that the known range of Histoplasma endemicity around the Yangtze River flows is shifting. The number of histoplasmosis cases is increasing but the prevalence of the disease has not vary highly over time. It could not estimate the total disease burden yet due to data from the literature review may reflect only a small fraction of the total disease burden while also underestimating the mildest cases.
Author contributions
L.C., H.Z, and S.D. conceived this study, analysed the data, and wrote the manuscript; L.C., D.H., C.Z., T.W., and X.C. conducted the experiments; F.H. analysed the data and revised the manuscript; All authors have read and agreed to the published version of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Adenis A, Nacher M, Hanf M, Basurko C, Dufour J, Huber F, Aznar C, Carme B, Couppie P. 2014. Tuberculosis and histoplasmosis among human immunodeficiency virus-infected patients: A comparative study. Am J Trop Med Hyg. 90(2):216–223. doi: 10.4269/ajtmh.13-0084.
- Almeida MA, Almeida Silva F, Guimarães AJ, Almeida Paes R, Zancopé Oliveira RM. 2019. The occurrence of histoplasmosis in Brazil: A systematic review. Int J Jnfect Dis. 86:147–156. doi:10.1016/j.ijid.2019.07.009.
- Antinori S. 2014. Histoplasma capsulatum: More widespread than previously thought. Am J Trop Med Hyg. 90(6):982–983. doi: 10.4269/ajtmh.14-0175.
- Antinori S, Giacomelli A, Corbellino M, Torre A, Schiuma M, Casalini G, Parravicini C, Milazzo L, Gervasoni C, Ridolfo AL. 2021. Histoplasmosis diagnosed in Europe and Israel: A case report and systematic review of the literature from 2005 to 2020. J Fungi (Basel). 7(6):481. doi:10.3390/jof7060481.
- Araúz AB, Papineni P. 2021. Papineni 2021. P Histoplasmosis Infect Dis Clin North Am. 35(2):471–491. doi: 10.1016/j.idc.2021.03.011.
- Bahr NC, Antinori S, Wheat LJ, Sarosi GA. 2015. Histoplasmosis infections worldwide: thinking outside of the Ohio river valley. Curr Trop Med Rep. 2(2):70–80. doi: 10.1007/s40475-015-0044-0.
- Benedict K, Mody RK. 2016. Epidemiology of histoplasmosis outbreaks, United States, 1938-2013. Emerg Infect Dis. 22(3):370–378. doi: 10.3201/eid2203.151117.
- Franklin AD, Larson L, Rauseo AM, Rutjanawech S, Hendrix MJ, Powderly WG, Spec A. 2021. A comparison of presentations and outcomes of histoplasmosis across patients with varying immune status. Med Mycol. 13(6):624–633. doi: 10.1093/mmy/myaa112.
- Jabr R, El Atrouni W, Male HJ, Hammoud KA. 2019. Histoplasmosis-associated hemophagocytic lymphohistiocytosis: A review of the literature. Can J Infect Dis Med Microbiol. 2019:7107326. doi:10.1155/2019/7107326.
- Lan G, Cunjian Z, Zhiqiang S, Yin Z, Li W, Baiyu Z, Fei H. 2010. Primary localized histoplasmosis with lesions restricted to the mouth in a Chinese HIV-negative patient. Int J Infect Dis. 14:e325–328. doi:10.1016/j.ijid.2010.04.002.
- Lv XL, Wang DZ, Guo Y, Chen GA. 2021. One case report of hemophagocytic syndrome secondary to disseminated Histoplasma capsulatum infection. Chinese J Infect Chemother. 21:473–475. in Chinese.
- Nguyen D, Nacher M, Epelboin L, Melzani A, Demar M, Blanchet D, Blaizot R, Drak Alsibai K, Abboud P, Djossou F, et al. 2020. Hemophagocytic lymphohistiocytosis during HIV infection in cayenne hospital 2012-2015: First think histoplasmosis. Front Cell Infect Microbiol. 24(10):574584. doi: 10.3389/fcimb.2020.574584.
- Ocansey BK, Kosmidis C, Agyei M, Dorkenoo AM, Ayanlowo OO, Oladele RO, Darre T, Denning DW, Govender NP. 2022 24. Histoplasmosis in Africa: Current perspectives, knowledge gaps, and research priorities. PLoS Negl Trop Dis. 16(2):e0010111. doi:10.1371/journal.pntd.0010111.
- Pan B, Chen M, Pan WH, Liao WQ. 2013. Histoplasmosis: A new endemic fungal infection in China? review and analysis of cases. Mycoses. 56(3):212–221. doi: 10.1111/myc.12029.
- Rodrigues AM, Beale MA, Hagen F, Fisher MC, Terra PPD, de Hoog S, Brilhante RSN, de Aguiar Cordeiro R, de Souza Collares Maia Castelo-Branco D, Rocha MFG et al. The global epidemiology of emerging histoplasma species in recent years. Stud Mycol. 97:100095. doi: 10.1016/j.simyco.2020.02.001.
- Song D, Wang J, Wang Z. 2021. Hemophagocytic lymphohistiocytosis secondary to disseminated histoplasmosis in an immunocompetent patient. Infect Dis Now. 51(3):308–309. doi: 10.1016/j.medmal.2020.09.019.
- Thompson GR, Thuy L, Ariya C, K CA, Ana A, Neil MA, David RA, Darius AJ, Ayanlowo O, Baddley JW, et al. 2021. Global guideline for the diagnosis and management of the endemic mycoses: An initiative of the European confederation of medical mycology in cooperation with the international society for human and animal mycology. Lancet Infect Dis. 21(12):e364–e74. doi:10.1016/S1473-3099(21)00191-2.
- Zhao B, Xia X, Yin J, Zhang X, Wu E, Shi Y, Tong M, Sun S, Gui X, Zhao Z, et al. 2001. Epidemiological investigation of Histoplasma capsulatum infection in China. Chin Med J(engl). 114(7):743–746.