?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Workers exposed to bullying often report musculoskeletal symptoms. In this study we have clinically evaluated the prevalence and nature of musculoskeletal dysfunction among a group of workers exposed to bullying and studied the relationship between clinical findings and self-reported musculoskeletal and mental symptoms.
Materials and methods
In a cross-sectional study, 144 patients admitted to an outpatient clinic for victims of workplace bullying were assessed with the Global Physiotherapy Examination 52 (GPE-52), a standardised test battery examining posture, respiration, movement, muscle and skin. The patients filled in self-report questionnaires regarding musculoskeletal symptoms (MSI), anxiety and depression (The Hospital Anxiety and Depression Scale, HADS) and post-traumatic stress symptoms (Impact of Events Scale revised version, IES-R).
Results
Patients victimised by bullying showed reduced flexibility, reduced ability to relax, restricted respiration and tense and painful muscles. The total GPE-52 sum-score and the main domains Movement and Muscle had significant correlations with most self-reported health variables, strongest between the subdomain Flexibility and HADS-D (r = 0.37) and HADS-A (r = 0.36).
Conclusions
Victims of bullying have clinically evident musculoskeletal dysfunctions that were further found to have a relationship with self-reported mental symptoms. Future health services for these patients should be multi-dimensional and include a bodily assessment by a physiotherapist and relevant treatment when needed.
Introduction
Workplace bullying is one of many stressors often included in studies on psychosocial risk factors and health [Citation1]. Also referred to as harassment, emotional abuse, mistreatment and ‘mobbing’ [Citation2], bullying denotes a situation with repeated and on-going exposure to negative behaviours from one’s colleague(s) or superiors [Citation3]. This predicament typically lasts and escalates over months to years, and is distinguished from a mere conflict situation not only by the repeated negative acts involved but also by the target’s inability to defend him- or herself in the actual situation, often due to a formal or informal perceived imbalance of power between the parties [Citation3].
Such an ongoing situation, generally evaluated as extremely harmful or threatening by the targets, is found to be a source of chronic or even traumatic stress [Citation4].
Exposure to workplace bullying has been documented as a prevalent problem in contemporary workplaces and as a serious threat to the health and well-being of those exposed, being related to a range of mental health problems, as well as self-reported psychosomatic and musculoskeletal complaints [Citation5–8]. Although physical and psychosomatic outcomes have been studied to a lesser degree than psychological outcomes in the form of anxiety and depression, a number of studies describe elevated levels of self-reported musculoskeletal complaints in targets. These studies mostly, however, focus on subjective complaints that are rather unspecific and quite prevalent in the population, such as backaches, muscular pain and headache [Citation9,Citation10]. A notable exception is Kivimäki et al., who studied the association between stress at work, including exposure to bullying, and newly diagnosed fibromyalgia in hospital employees [Citation11]. Being a target of bullying at work was associated with a fourfold risk of physician-diagnosed fibromyalgia, as reported in a questionnaire by the study participants.
Yet, published data on musculoskeletal health problems in targets of workplace bullying are mainly based on surveys with self-reports employing predefined symptom checklists. Clinical assessments and observational data are therefore highly needed to obtain objective and nuanced health data for workers suffering from workplace bullying [Citation12]. So, even if relationships between bullying and musculoskeletal complaints are well documented, these are so far based on the targets’ own perceptions and reports. Clinical validation of these perceptions and clinical descriptions of potential health impairment in the musculoskeletal domain are still lacking.
Part of the bullying experience for many targets involves the threat of social exclusion, an experience often accompanied by severe social pain [Citation13,Citation14]. The social pain/physical pain overlap theory (SPOT), suggests that social and physical pain might rely on overlapping neural processes in the form of a common neural alarm system [Citation15]. This might then explain why targets of bullying so frequently describe musculoskeletal complaints, where bodily pain is the main symptom. Are these perceptions only a mirror of neurological processes, or do they indicate actual bodily changes in the musculoskeletal system?
The main aim of the present study was to examine whether patients exposed to workplace bullying have clinically evident dysfunction in their musculoskeletal system. We have therefore evaluated the prevalence and nature of musculoskeletal dysfunction among targets of bullying seeking healthcare by way of a clinical examination. Secondly, we wanted to investigate how these clinical findings are related to patients’ self-reported musculoskeletal symptoms and mental health symptoms. These data may then validate the instruments often used in studies on victims of workplace bullying.
Materials and methods
This is a clinical cross-sectional study among patients seeking treatment at an outpatient clinic for victims of workplace bullying.
Participants
All patients (n = 161) assessed at a clinic for targets of workplace bullying, Jobbfast, in the period from August 2011 throughout February 2017, were invited to participate in the study. Jobbfast was part of the Outpatient clinic at the Department of Occupational Medicine, Haukeland University Hospital in Bergen, where patients from all over Norway were referred because of health problems due to experiences of bullying or harassment in their workplace. Over a period of three consecutive days, the patients went through a clinical program by a team of doctors, a psychologist, a physiotherapist and an occupational consultant [Citation16].
Self-administered questionnaires
Prior to the physical examination, all patients answered a battery of pen and pencil questionnaires.
Negative Acts Questionnaire 22 (NAQ-22)
We used the revised version of the Negative Acts Questionnaire 22 (NAQ-22) [Citation17] to assess the patients’ exposure to workplace bullying. This is a highly validated questionnaire and the most used questionnaire on workplace bullying globally [Citation18]. NAQ-22 is also an example of the behavioural experience method for the measurement of workplace bullying. The questionnaire consists of 22 items where the patients are asked to rate how often they have experienced different specific negative acts at work over the past 6 months. A number of patients were sick-listed at the time of assessment and had not experienced negative acts in the previous 6 months. They were asked to rate their exposure to negative acts when the exposure was at its peak. The response alternatives are ‘never’, ‘now and then’, ‘monthly’, ‘weekly’ and ‘daily’. A sum score is calculated, with a range from 22 to 110 points. The validated cut-off score is set at 33 points for low-intensity bullying and 45 for high-intensity bullying [Citation19]. In this study, ‘being a victim of bullying’ was defined as having a score of 33 or more.
Musculoskeletal Index (MSI)
The participants were also asked to rate their health with an instrument for the assessment of subjective health complaints (SHC), previously validated in a study performed at the National Institute of Occupational Health in Norway [Citation20]. We used the instrument to assess the intensity and duration of self-reported musculoskeletal complaints the preceding 14 days prior to assessment. The intensity is rated on a four-point scale (0 = not troubled, 1 = a little troubled, 2 = quite troubled, 3 = seriously troubled), the duration has three dimensions (1 = 1–5 days, 2 = 6–10 days, 3 = 11–14 days). We computed one complaint-severity index (index range 0–9): musculoskeletal (MSI). MSI constitutes the following 12 items: Headache, neck pain, pain in the left shoulder or upper arm, pain in the right shoulder or upper arm, pain in the left forearm, pain in the right forearm, pain in left wrist or hand, pain in right wrist or hand, pain in the upper back, pain in the lower back, chest pain and pain in lower extremities.
Pain drawing
In a validated pain drawing, the patients indicated their area of pain the previous 14 days prior to the physiotherapy examination. The drawing is an outline of the human body with a frontal and a posterior view, placed on a grid with a total of 120 squares [Citation21,Citation22]. According to pain localisation, we categorised the patients into three groups: group 1: head/neck and shoulders, group 2: lower back/legs, and group 3: widespread pain, that is, pain located both in the upper and lower body. Patients who reported any bodily pain were asked to state the average pain intensity during the last 14 days on a 10 cm wide visual analogue scale (VAS) going from 0 (no pain) to 10 (worst possible).
The Hospital Anxiety and Depression Scale (HADS)
The Hospital Anxiety and Depression Scale (HADS) was used to rate symptoms of anxiety and depression. This is a validated, frequently used instrument in clinical studies [Citation23]. It consists of seven items for anxiety (HADS-A) and seven for depression (HADS-D). Each item is scored on a four-point scale from 0 (not present) to 3 (considerable), giving subscale scores on HADS-A and HADS-D from 0 to 21. A sum-score of 8 points is the suggested cut-off for possible disorder on both scales.
Impact of Events Scale – revised version (IES-R)
Many targets of bullying present with symptoms of post-traumatic stress disorder [Citation4,Citation6]. Post-traumatic stress symptoms were therefore assessed with the 22-item revised and validated version of the Impact of Events Scale revised version (IES-R) [Citation24], with a five-point response scale ranging from 0 (not at all) to 4 (very high degree) with respect to how distressing each item has been during the past week, and the total score range is 0–88 [Citation25]. The patients reported symptoms during the last 7 days in relation to difficult experiences at work. A suggested cut-off for patients with posttraumatic stress disorder (PTSD) is set at 33 in a review [Citation26].
Clinical examination
One of two experienced physiotherapists examined the patients in order to assess the degree of physical aberrations. Prior to the examination, a physician had assessed the patients, and medical history including ongoing musculoskeletal disorders (MSD) was noted. Except for general information on which patients were referred to the clinic, and the sex of the patient, the physiotherapist had no information on patient history, diagnoses or self-reported mental health scores. The physiotherapist was briefly informed if there was a history of known sexual abuse since the examination requires bodily touch and palpation.
The Global Physiotherapy Examination-52 (GPE-52), a standardised and validated test battery with 52 tests (items), was used as body examination [Citation22,Citation27]. GPE-52 was developed to document where and to what extent the patient has bodily problems and resources, and is intended for patients with MSD and/or psychiatric or psychosomatic disorders. The method is based upon the notion that the whole body may react to long-lasting physical and/or psychological problems with resulting changes in muscle tension, movements, respiration and posture [Citation22]. The method has been examined for reliability and different aspects of validity in healthy persons, in patients diagnosed with long-lasting MSD (defined as musculoskeletal pain >12 weeks) [Citation22,Citation27], in patients with dizziness [Citation28], and in patients diagnosed with different psychiatric disorders [Citation29].
GPE-52 yields information in five main domains: Posture (8 items), Respiration (8 items), Movement (16 items), Muscle (12 items) and Skin (8 items). These main domains consist of altogether 13 subdomains; each with four tests (items) [Citation22,Citation27]. No equipment is needed when performing the examination, only observation and handling by the therapist, in addition to a ruler and a goniometer during testing of passive range of motion. All tests and positions are standardised, and have little measurement error [Citation27]. Postural and respirational items are observed both in standing and supine positions. The Movement domain includes passive tests of range of motion (ROM), testing of flexibility in the head and trunk, and of ability to relax in response to passive movements performed by the therapists with the patient in standing and supine, as well as active movements performed by the patient. Included in the examination of the Muscle and Skin domains are stretch and pressure palpation and reaction to stretch palpation of muscle, performed by the therapist with the patient in supine [Citation27]. Every item is scored according to an empirically defined standard or ideal, given the score 0, and deviations from the standard can go in two directions; decreased or increased findings with a score ranging from −2.3 to +2.3. The scores of each item are summed to 13 subdomain sum-scores (each subdomain consisting of the absolute sum-score from four of the 52 items) and to five main domain sum-scores, in addition to the total GPE-52 sum-score. The maximum possible score is 119.6. Based on data from healthy subjects the following categories have been defined in the 13 subdomains (sum of score in four tests): cut-off score <3.0: normal or adequate function, score ≥3.0–6.0: moderate dysfunction and score >6.0: major dysfunction. Total GPE-52 sum-score <39 usually indicates a good result [Citation22,Citation30,Citation31]. The examination takes 30–45 min.
The results of the physiotherapy examination will be compared to results from a previous study where 104 healthy individuals (62% female) with no history of pain the last 12 months and 247 patients diagnosed with long-lasting MSD (70% female), all were assessed with the GPE-52 [Citation22]. The patients with MSD all had long-lasting pain problems and had been diagnosed with different MSDs upon admittance to a rehabilitation clinic. Of these, 55% had widespread pain when categorised by the formerly mentioned pain drawing. When they were examined with the GPE-52 they had been on sick-leave due to MSD for a mean of 3.3 months (not more than 4 months), but had suffered MSD/pain for much longer. GPE-52 scores in other samples with healthy persons and patients with MSD have been replicated and validated in later studies [Citation29].
Statistics
Descriptive methods were used to characterise the sample. GPE-52 and its subdomains were compared between the three groups using ANOVA (normality assumptions hold), and with t-test when comparing gender. The associations between GPE-52 and its main- and subdomains on one side and MSI, HADS and IES-R on the other were assessed by Spearman correlations. The general significance level was set to 0.05. Accounting for multiple comparisons we used the Bonferroni adjustment (GPE-52 and all main- and subdomains) leading to a marginal level of 0.0026. The computation was done in SPSS 24 (IBM Inc., Armonk, NY) and Matlab 9.5 (Mathworks, Natick, MA), the graphics were derived using Matlab 9.5.
In this study we were correlating different constructs; bodily dysfunction as found by clinical examination and self-reported mental symptoms. When interpreting the strength of relationships between different constructs, lower coefficients can be expected than when using similar constructs [Citation32]. This interpretation was used in this study and implies that r ≥ 0.50 was defined as strong, r ≥ 0.30–0.49 as moderate, and r ≥ 0.10–0.29 as weak.
Results
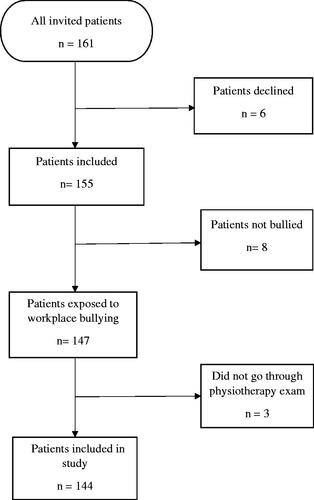
Altogether 155 patients (96%) agreed to participate, of whom 147 met the criteria for being a victim of workplace bullying. Of these, 144 went through the physiotherapy examination and were included in the study (see ). shows descriptive characteristics and outcomes in the study participants for the sample as a whole, as well as for women and men separately.
Table 1. Characteristics of bullied patients.
Eighty-one percent of the study participants were women, and the median age in the sample was 52 years. At the time of assessment, 65 patients (45%) reported symptoms consistent with ongoing MSD. As many as 110 (77.5%) of the patients reported widespread bodily pain on the pain drawing, and only five (3.5%) reported no pain. The prevalence of sexual abuse history was comparable to what is seen in the general population [Citation33].
Negative Acts Questionnaire 22 (NAQ-22)
It is noteworthy that 101 patients (70%) had a NAQ score ≥45 indicating high-intensity bullying. The remaining 43 patients scored above the lower threshold for bullying exposure (≥33).
Musculoskeletal Index (MSI)
In the questionnaire on subjective health complaints, 42 patients (29%) indicated to be quite troubled or seriously troubled with muscle pain (score ≥2 on the MSI subscale).
The Hospital Anxiety and Depression Scale (HADS)
The mean scores on HADS anxiety and depression were in the range of possible disorder [Citation23].
Impact of Events Scale – revised version (IES-R)
The IES-R showed a mean score suggestive of PTSD [Citation26]; 68% of the patients had a score ≥33.0, being the threshold indicative for PTSD.
Gender differences
Descriptive characteristics were comparable for women and men, but with some noteworthy exceptions. The men had higher scores on mental symptoms (HADS and IES-R), but comparable scores on MSI and prevalence of MSD. On the other hand, a higher percentage of women scored above the cut-off for high-intensity bullying; 75% vs 63% among men.
Physiotherapy examination
In , the results of the physiotherapy examination is displayed. The figure depicts the patients in our study, as well as results from the previous study where 104 healthy individuals were compared with 247 patients diagnosed with long-lasting MSD. This previous study also used GPE-52 [Citation22]. See supplemental file.
Figure 2. Results of the physiotherapy examination GPE-52 in bullied patients compared to 247 patients diagnosed with long-lasting MSD and 104 healthy individuals.
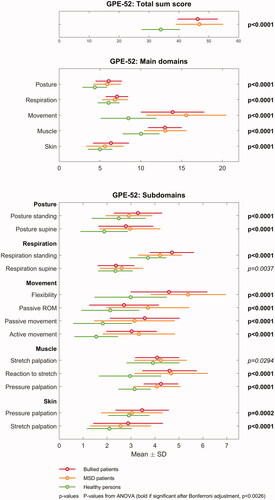
Among the patients in our study, mean GPE-52 scores were 3.0 for nine of 13 subdomains In most of these, the score was above or equal to the score for the MSD patients, and significantly higher than the scores reported for healthy persons, illustrated in [Citation22]. The results were most prominent in the two main domains Movement and Muscle. The subdomains Respiration standing, Flexibility, Stretch and Reaction to stretch palpation, as well as Pressure palpation of muscle, had the highest scores.
The mean GPE-52 total score for the bullied patients’ was 46.3 (SD 6.7), equivalent to the mean of the MSD patients that was 46.9 (SD 8.0), whereas the mean score for healthy persons was 33.9 (SD 6.4) [Citation22].
In the GPE-52 sub-domains results for the bullied patients are listed. Although the results are quite similar for the two genders, men had scores above 3.0 in ten subdomains (as opposed to nine for women), and higher mean GPE-52 total score (47.8 vs 45.9), indicating even more dysfunction.
Table 2. Mean values (and standard deviation) of GPE-52 within 13 subdomains and total sum score in bullied patients; whole sample, and women and men separately.
Associations between clinical findings and self-reported musculoskeletal and mental health symptoms
illustrates the correlations between all bullied patients’ clinical findings in the physiotherapy examination and their self-reported symptoms. See also the supplemental file. The total GPE-52 sum-score, as well as the main domains Movement and Muscle had weak to moderate correlations (r = 0.14–0.36) with the scores on all four questionnaires; MSI, HADS-anxiety, HADS-depression and IES-R. The strongest correlation was found between Movement and HADS-A (r = 0.36). For Respiration, we found significant yet weak correlations with HADS-D and IES-R (r = 0.20 and 0.17, respectively). The main domains Posture and Skin had hardly any correlations with the questionnaires. In the subdomains, Flexibility had moderate correlations to all four questionnaires (r = 0.33–0.37).
Figure 3. Correlations between all bullied patients’ self-reported symptoms and the clinical findings in the physiotherapy examination GPE-52. Correlations with 95% CI.
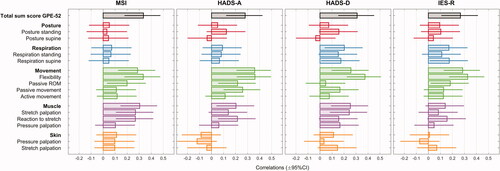
lists the correlations separately for men and women between GPE-52 and the sub-domains, versus the self-report questionnaires. For women, the subdomain Flexibility was moderately correlated to all self-report symptoms, whereas Reaction to stretch of muscle had weak to moderate correlations, and Respiration in supine had low correlations with all four questionnaires. Several other correlations were also significant for women, indicated with asterisks in . For men, none of the correlation coefficients were significant, although several estimates had r > 0.20, such as in Respiration standing, Passive ROM, Active movement, and Stretch and Pressure of muscle. The higher correlations were mostly related to HADS-A, MSI and IES-R, and some also to HADS-D. There were also other interesting differences between men and women: The two skin subdomains showed weak to moderate correlations with three of four self-report symptoms in men (r = 0.15–0.33). For women, the only notable correlation in the Skin subdomains was stretch palpation which was weakly correlated to HADS-D (r = 0.15).
Table 3. Correlations for bullied women (n = 117) and men (n = 27).
Discussion
The present study shows that patients exposed to workplace bullying have clinically evident dysfunction in their musculoskeletal system, comparable to a heterogeneous sample of patients diagnosed with long-lasting MSD and significantly more so than healthy controls. The clinical findings in the physiotherapy examination confirm the patients’ self-report, where 77.5% of the bullied patients reported widespread pain (see ). This is a very high proportion; even higher than in the study on MSD patients where 55% reported widespread pain [Citation22]. Only five of the bullied patients reported no pain. Interestingly, men in the bullied sample had significantly more dysfunction than women in three of the Movement subdomains. In general, however, there were stronger correlations for women than men between the GFM-52 outcomes and the self-reported outcomes. However, a note of caution must be added, due to the low number of men (n = 27).
The total GPE-52 sum-score for bullied patients was comparable to what is previously found in patients sick-listed due to long-lasting MSD [Citation22] and also in patients undergoing a rehabilitation program for dizziness [Citation28]. The main domain Movement, especially tests representing reduced flexibility, mobility, and ability to relax, and tests in Muscle, representing tense and painful muscles, showed the highest aberration. In addition, Respiration in the standing position was more affected (i.e. tense and restricted) in our patient group than in the said patients with MSD. When analysing men and women separately, we found some notable differences, equivalent to former findings in patients with MSD [Citation22]. Men had significantly more restricted movements and women had more resistance in their skin when doing pressure palpation.
The total GPE-52 sum-score and its domains were significantly correlated with all self-reported health variables; MSI, HADS-anxiety, HADS-depression and IES-R, as illustrated in . Particularly dysfunction in Flexibility was correlated with symptoms of anxiety, depression and post-traumatic stress (HADS and IES-R), respectively. Restricted respiration and tense and painful muscles were also associated with reported psychological distress. Associations between bodily aberrations measured with GPE and psychological symptoms has been reported in a former study [Citation21]. The associations were different for bullied women and men, as was found in the former study (). For women, the correlations to psychological symptoms were significant and moderate to weak (r < 0.4) and most prominent in the Movement and Muscle domains. For men, clinical aberrations in Respiration and Skin had several associations r > 0.20, but none were significant, probably due to the small sample size. This indicates, on one hand, that there is a relationship between physical and psychological findings, but also that the variance in data is considerable and somewhat different for women and men. The study indicates that the methods we have used to assess mental and physical health complement each other. As bullied patients have both physical as well as psychological aberrations, single-mode treatment approaches might be insufficient.
The results of the physiotherapy examination imply that bullied patients have a bodily function characterised by restrained breathing, reduced flexibility and ability to relax, and a painful muscular system. These are unequivocal findings that confirm previous results in several surveys where bullied workers reported musculoskeletal symptoms [Citation34–36]. The findings could very well be the result when the individual has been in a state of physiological stress for a long time. A model of the interplay between psychological defences and bodily conditions, describes how repression and denial of emotional experiences manifest in patterns of less flexibility/mobility and a restrained respiration as well as increased muscle tension [Citation37,Citation38]. This relationship has not, according to the authors’ knowledge of the literature, been systematically investigated in victims of bullying before.
The patients in our study had a high degree of post-traumatic stress symptoms; mean score on the IES-R was 42.9, well above the suggested cut-off at 33 points for PTSD [Citation26]. 68% of the patients had a score above this threshold. This confirms previous studies on bullied workers where post-traumatic stress symptoms are frequently reported. In a meta-analysis and literature review published in 2015 the authors concluded that an average of 57% of victims reported symptoms of PTSD above thresholds for caseness [Citation4]. Interestingly, the men in our study reported higher levels of anxiety, depression and post-traumatic stress symptoms than women. This even though they seemingly were less exposed by negative acts at work, reflected in a lower prevalence of high-intensity bullying.
In a former study of patients with MSD, patients with widespread long-lasting pain had strong correlations between the precursor of GPE-52 and several MMPI-2 subscales (MMPI-2: Revised Minnesota Multiphasic Personality Inventory), indicating a psychosomatic V-profile with affective disturbances and somatic problems [Citation21]. Patients with anxiety and depression often suffer from physical health conditions, including musculoskeletal health problems. As the patients in our study had outcomes on HADS indicating anxiety and depression, this has to be taken into consideration when trying to explain the relationship between workplace bullying and musculoskeletal dysfunction. One explanation could be that workplace bullying first impacts psychological health, which then results in physical health aberrations. Yet, the present results indicate that the musculoskeletal symptoms reported by victims of bullying in fact reflect bodily dysfunction and are not simply correlates of mental health problems or a mirror of neurological overlap between social and bodily pain [Citation15].
Strengths and limitations
As this study has a cross-sectional design, it is not possible to conclude on a possible causal relationship between workplace bullying and musculoskeletal dysfunction. It is therefore advisable that future research should include studies with a longitudinal design. Although the study population is a highly selected group of patients referred to our department by their family physician, the high response rate strengthens the study. Another strength of the study was the use of standardised instruments in the assessment of the patients. The two physiotherapists were specially trained for using the method GPE-52, minimising any interpersonal variation in methods and measurement. The physiotherapists examined the patients without any information regarding patient history, work situation or self-reported health as measured in the questionnaires.
The majority of patients in this study had been exposed to high-intensity bullying; 101 of 144 had a NAQ score above the threshold value of 45, with the rest scoring above the threshold of 33 indicative of low-intensity bullying (). A study published in 2012 indicated that only 2.1% of the Norwegian workforce had a score ≥45 [Citation19], clearly indicating that our study population consists of individuals with high exposure to workplace bullying. This might explain the extent of the bodily problems in the patient group. To clarify the extent of physical dysfunction in patients exposed to less intense bullying, further studies are needed.
Even though the physical aberrations in the patient group as a whole are quite convincing, there were individuals with a normal result on the GPE-52, as illustrated with the standard deviation in and . Furthermore, findings in our study could also support the use of only parts of GPE-52, as the examination of Posture and Skin seemed less informative, while examination of Respiration, Movement and Muscle were. Noteworthy, this is not a study of bullying from a legal perspective, hence, we are looking at patients that together with their family or occupational physician had sought treatment for health problems that they perceived to be caused by exposure to bullying and harassment. Yet, the inclusion criteria were based on the patients` information on their exposure to specific negative acts, typical for victims of bullying employing national cut-off scores. Further studies are needed to conclude whether workplace bullying is in fact causing these problems and to what extent mental health problems are mediating factors.
Last but not least, our patients are predominantly female. Although a typical feature of these kinds of studies, this poses a problem regarding our knowledge on differences between female and male targets and must be addressed in future studies.
Implications
To the best of our knowledge, this is the first clinical study on the musculoskeletal system of workers exposed to workplace bullying. The study is therefore important as a validation of earlier findings employing self-report data. In addition, the knowledge we provide on health status and symptomatology in these victims is important for practitioners, be it physicians, physiotherapists or psychologists in general practice or in hospital settings.
The results in our study indicate that future health services to bullied patients should be based on a multi-dimensional approach. A thorough clinical examination of both psychological and physical health, including physiotherapy examination, is advisable. Patients with documented physical aberrations may benefit from a follow-up that includes an exercise and body awareness program promoting improved flexibility, ability to relax, improved breathing and less muscle tension. Improvement in these areas could represent a form of coping that also could influence their general health condition, including their mental health. Treatment programs having a multidisciplinary approach needs to be further developed and evaluated.
Conclusions
The present study shows that targets of bullying seeking healthcare have a high degree of musculoskeletal dysfunctions, in support of previous questionnaire studies on physical health in workers exposed to workplace bullying. The extent of the musculoskeletal problems revealed in our study clearly indicates that these problems should be addressed in future health services to these patients. Secondly, these bodily problems are significantly related to psychological symptoms of anxiety, depression and posttraumatic stress. Hence, treatment programs addressing the health of targets of bullying should therefore be multi-dimensional and multi-disciplinary and include both bodily and mental health assessments.
Ethical approval and consent to participate
All subjects were thoroughly informed by personal instruction, and written consent was obtained at inclusion. It was emphasised that participation was voluntary, and a refusal to participate or withdraw from the study, later on, would have no consequences for treatment. The study was approved by The Regional Committee for Medical and Health Research Ethics Western Norway (REK Vest, REK no 2014/53), and by the Norwegian Social Science Data Services (NSD).
Author contributions
KB, NM, SE and AK have planned and carried out the study, and participated in the interpretation of the data analysis, and reviewed and revised the manuscript. JA planned and performed statistical analyses. All authors read and approved the final manuscript.
| Abbreviations | ||
| SPOT | = | The social pain physical pain overlap theory |
| NAQ-22 | = | The revised version of the Negative Acts Questionnaire 22 |
| MSI | = | Musculoskeletal Index |
| VAS | = | Visual Analogue Scale |
| HADS | = | The Hospital Anxiety And Depression Scale |
| HADS-A | = | Anxiety subscale of HADS |
| HADS-D | = | Depression subscale of HADS |
| IES-R | = | the Impact of Events Scale –revised version |
| PTSD | = | posttraumatic stress disorder |
| MSD | = | musculoskeletal disorders |
| GPE-52 | = | Global Physiotherapy Examination-52 |
| ROM | = | range of motion |
| MMPI-2 | = | revised Minnesota Multiphasic Personality Inventory. |
Supplemental_file_11.20.20_KB.docx
Download MS Word (17.4 KB)Acknowledgements
We would like to thank colleague and physiotherapist Astrid Aalvik for contributing to the examination of patients, Mr. Øystein Hoprekstad for entering the data used in this study and Mr. Stein Håkon Låstad Lygre for valuable advice in handling and interpreting the data.
Disclosure statement
The authors declare that they have no competing interests. This work was completed at the Department of Occupational Medicine, Haukeland University Hospital without any external funding.
Data availability statement
Readers who want access to data should contact the first author. Data will be made available in line with data protection procedures of the said hospital.
References
- Schutte S, Chastang JF, Malard L, et al. Psychosocial working conditions and psychological well-being among employees in 34 European countries. Int Arch Occup Environ Health. 2014;87(8):897–907.
- Aquino K, Thau S. Workplace victimization: aggression from the target’s perspective. Annu Rev Psychol. 2009;60:717–741.
- Einarsen S, Hoel H, Zapf D, et al. The concept of bullying and harassment at work: the European tradition. Bullying and harassment in the workplace Developments in theory, research, and practice. Boca Raton (FL): Taylor & Francis Group; 2011. p. 3–39.
- Nielsen MB, Tangen T, Idsoe T, et al. Post-traumatic stress disorder as a consequence of bullying at work and at school. A literature review and meta-analysis. Aggress Violent Beh. 2015;21(0):17–24.
- Kivimaki M, Virtanen M, Vartia M, et al. Workplace bullying and the risk of cardiovascular disease and depression. Occup Environ Med. 2003;60(10):779–783.
- Nielsen MB, Einarsen S. Outcomes of exposure to workplace bullying: a meta-analytic review. Work & Stress. 2012;26(4):309–332.
- Hogh AM, Hansen ÅM. Individual consequences of workplace bullying/mobbing. In: Press C, editor. Bullying and harassment in the workplace development in theory, research, and practice. Boca Raton (FL): Taylor & Francis Group; 2011. p. 107–128.
- Aarestad SH, Einarsen SV, Hjemdal O, et al. Clinical characteristics of patients seeking treatment for common mental disorders presenting with workplace bullying experiences. Front Psychol. 2020;11:583324.
- Takaki J, Taniguchi T, Hirokawa K. Associations of workplace bullying and harassment with pain. Int J Env Res Public Health. 2013;10(10):4560–4570.
- Nixon AE, Mazzola JJ, Bauer J, et al. Can work make you sick? A meta-analysis of the relationships between job stressors and physical symptoms. Work & Stress. 2011;25(1):1–22.
- Kivimaki M, Leino-Arjas P, Virtanen M, et al. Work stress and incidence of newly diagnosed fibromyalgia: prospective cohort study. J Psychosom Res. 2004;57(5):417–422.
- Nielsen MB, Mageroy N, Gjerstad J, et al. Workplace bullying and subsequent health problems. Tidsskr nor Laegeforen. 2014;134(12–13):1233–1238.
- Einarsen S, Hoel H, Zapf D, et al. Bullying and harassment in the workplace developments in theory, research, and practice. 2nd ed. Boca Raton (FL): CRC Press; 2011.
- Eisenberger NI. The pain of social disconnection: examining the shared neural underpinnings of physical and social pain. Nat Rev Neurosci. 2012;13(6):421–434.
- Eisenberger NI, Lieberman MD. Why it hurts to be left out: the neurocognitive overlap between physical and social pain. In: Williams KD, Forgas JP, Hippel Wv, editors. The social outcast: ostracism, social exclusion, rejection, and bullying. New York (NY): Cambridge University Press; 2005. p. 109–130.
- Buhaug K, Aasen TB, Einarsen S, et al. Health care related to workplace bullying. Tidsskr nor Laegeforen. 2013;133(20):2129–2130.
- Einarsen S, Hoel H, Notelaers G. Measuring exposure to bullying and harassment at work: validity, factor structure and psychometric properties of the Negative Acts Questionnaire-Revised. Work Stress. 2009;23(1):24–44.
- Nielsen MB, Notelaers G, Einarsen SV. Methodological issues in the measuring of workplace bullying. In: Einarsen S, Zapf D, Cooper CL, editors. Bullying and harassment at work: theory, research and practice. Boca Raton (FL): CRC Press Taylor and Francis; 2020.
- Notelaers G, Einarsen S. The world turns at 33 and 45: defining simple cutoff scores for the Negative Acts Questionnaire–Revised in a representative sample. Eur J Work Organ Psy. 2013;22(6):670–682.
- Steingrimsdottir OA, Vollestad NK, Roe C, et al. Variation in reporting of pain and other subjective health complaints in a working population and limitations of single sample measurements. Pain. 2004;110(1–2):130–139.
- Kvåle A, Ellertsen B, Skouen JS. Relationships between physical findings (GPE-78) and psychological profiles (MMPI-2) in patients with long-lasting musculoskeletal pain. Nord J Psychiatry. 2001;55(3):177–184.
- Kvåle A, Skouen JS, Ljunggren AE. Discriminative validity of GFM-52 in patients with long-lasting musculoskeletal pain versus healthy persons. J Musculoskeletal Pain. 2003;11(3):23–35.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370.
- Weiss D, Marmar C. The Impact of Event Scale - revised. In: Keane JWTM, editor. Assessing psychological trauma and PTSD. New York (NY): Guilford Press; 2006. p. 399–411.
- Beck JG, Grant DM, Read JP, et al. The Impact of Event Scale-Revised: psychometric properties in a sample of motor vehicle accident survivors. J Anxiety Disord. 2008;22(2):187–198.
- Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale - Revised. Behav Res Ther. 2003;41(12):1489–1496.
- Kvåle A, Skouen JS, Ljunggren AE. Sensitivity to change and responsiveness of the global physiotherapy examination (GPE-52) in patients with long-lasting musculoskeletal pain. Phys Ther. 2005;85(8):712–726.
- Kvåle A, Wilhelmsen K, Fiske H. Physical findings in patients with dizziness undergoing a gruop exercise program. Physiother Res Int. 2008;13(3):162–175.
- Kvåle A, Bunkan BH, Opjordsmoen S, et al. Development of the movement domain in the global body examination. Physiother Theory Pract. 2012;28(1):41–49.
- Kvåle A, Ljunggren AE, Johnsen TB. Examination of movement in patients with long-lasting musculoskeletal pain: reliability and validity. Physiother Res Int. 2003;8(1):36–52.
- Kvåle A, Ljunggren AE, Johnsen TB. Palpation of muscle and skin. Is this a reliable and valid procedure in assessment of patients with long-lasting musculoskeletal pain? Adv Physiother. 2003;5(3):122–136.
- Carter R, Lubinsky J. Rehabilitation research: principles and applications. Amsterdam (The Netherlands): Elsevier Health Sciences; 2015.
- Stoltenborgh M, Van Ijzendoorn MH, Euser EM, et al. A global perspective on child sexual abuse: meta-analysis of prevalence around the world. Child Maltreat. 2011;16(2):79–101.
- Min JY, Park SG, Kim SS, et al. Workplace injustice and self-reported disease and absenteeism in South Korea. Am J Ind Med. 2014;57(1):87–96.
- Kaaria S, Laaksonen M, Rahkonen O, et al. Risk factors of chronic neck pain: a prospective study among middle-aged employees. Eur J Pain. 2012;16(6):911–920.
- Janssens H, Clays E, De Clercq B, et al. The relation between psychosocial risk factors and cause-specific long-term sickness absence. Eur J Public Health. 2014;24(3):428–433.
- Reich W. Character analysis. New York (NY): Farar, Strauss & Giroux; 1969.
- Monsen K, Havik OE. Psychological functioning and bodily conditions in patients with pain disorder associated with psychological factors. Br J Med Psychol. 2001;74:183–195.