ABSTRACT
Public Health Emergency Operations Centers (PHEOCs) are the critical units to lead communications, information sharing, and resource mobilisation during national and international health emergencies, and are key components for maintaining global health security. This assessment sought to examine the coordination mechanisms between national and sub-national PHEOCs in Thailand, Cambodia, Lao People’s Democratic Republic, and Malaysia (TCLM countries) during the COVID-19 pandemic. Information was collected on PHEOC structures, functions, and cross-border communications in three stages: a literature review of national PHEOC and emergency preparedness capacities; questionnaire responses from stakeholders to describe PHEOC activity at the national level; and meetings with emergency response staff in five border provinces of Thailand to assess communications between sub-national PHEOCs across country borders. The findings showed that each of the countries has demonstrated a commitment to strengthening their national PHEOCs and improving cross-border communication in the face of the COVID-19 pandemic. Strong existing relationships between TCLM countries assisted in activating a coordinated pandemic response, but gaps remain in efficient data sharing, workforce capacity, and the utilisation of consistent communication platforms among countries. Lessons learned from the pandemic can be used to further strengthen countries’ preparedness for future health emergencies, in line with International Health Regulations (2005) and regional plans to build health security in the Southeast Asia region. This assessment provides TCLM countries with the opportunity to address weaknesses in national and international PHEOC capacities. It may be used alongside existing guidelines to prepare the region for a stronger response to future global and regional health emergencies.
Introduction
Public Health Emergency Operations Centers (PHEOCs) are critical for global health security (World Health Organization, Citation2014). During national and international public health emergencies, PHEOCs function to lead, direct, communicate, and coordinate efforts to control and lessen the impacts of health threats. With timely communication during the early stages of a public health crisis, effective responses can be mobilised to prevent widespread disease by providing early warning signals, describing the dynamic nature of the situation, and analysing risk factors to inform decision-making and guide the response (World Health Organization, Citation2017d). Communication within PHEOCs and stakeholder agencies is necessary for domestic disease control, and it is also crucial to foster communication between PHEOCs of other countries to mitigate the adverse effects of public health threats, including COVID-19 (Hinjoy et al., Citation2020). To succeed in their operations, fully functioning PHEOCs require strong organisational structure, adherence to the standardised Incident Command System (ICS), policy and resource support, and information and communication infrastructure, as well as adequate numbers of dedicated, experienced, and highly competent staff (Balajee et al., Citation2017; World Health Organization, Citation2015). Both the International Health Regulations (IHR) (2005) and the Global Health Security Agenda (GHSA) have recognised the importance of maintaining functional PHEOCs to enhance global health security and mitigate international public health threats (CDC, Citation2014; World Health Organization, Citation2005).
Thailand, Cambodia, Lao People’s Democratic Republic (PDR), and Malaysia (collectively referred to in this paper as TCLM countries) face frequent emerging and re-emerging disease threats that have the potential to spill over into neighbouring countries due to the cross-border movement of people and animals. In 2017, officials in the Association of Southeast Asian Nations (ASEAN) the Member States, including TCLM countries, agreed to maintain high levels of collaboration and capacity to detect, investigate, and contain outbreaks of emerging and re-emerging infectious diseases in the region, and established the ASEAN Emergency Operations Center (EOC) Network to assist with communication and information-sharing in the event of public health emergencies (ASEAN Health Cluster 2, Citation2017). These existing relationships between TCLM countries and ASEAN were leveraged at the start of the COVID-19 pandemic to coordinate responses and prevent SARS-CoV-2 spread from nearby Wuhan, China.
Continued disease threats including COVID-19 reinforce the need for effective collaboration between countries. Standardized lines of communication and data sharing protocols strengthen the interoperability of national PHEOCs and increase preparedness to respond to national, regional, and global emergencies. Countries in the Southeast Asia region, including TCLM countries, have based their strategic plans for emergency preparedness and response on IHR (2005) mechanisms and World Health Organization (WHO) strategies for emerging disease threats (Corwin et al., Citation2021; East Asia, Citation2019). While regional plans are in place for public health preparedness and response, including for the response to COVID-19 (East Asia, Citation2020), the practical applications of international coordination between the PHEOCs of TCLM countries have not been examined in the face of the pandemic. Under the facilitation of Thailand’s Office of International Cooperation (OIC), a project was conducted from April 2020 to May 2021 in collaboration with the governments of Cambodia, Lao PDR, and Malaysia to better understand the international coordination mechanisms across TCLM countries’ PHEOCs, and to assess their capacities to detect, prevent, and respond to public health threats including COVID-19. This paper aims to identify the strengths, gaps, and challenges TCLM countries face in achieving a coordinated PHEOC response to public health threats. With lessons learned from the COVID-19 pandemic, we provide suggestions to improve preparedness and response to emerging infectious disease threats across the TCLM borders.
Methods
Our assessment and analysis of PHEOC coordination mechanisms in TCLM countries contained three stages: a desk review of PHEOC capacities and legal frameworks in each of the TCLM countries, a written questionnaire to assess cross-border PHEOC communication and coordination at the national level during COVID-19, and a series of meetings to assess international coordination mechanisms at the sub-national level during COVID-19.
The desk review assessed PHEOC legislative frameworks, practices, policies, and resources for international coordination among each of the TCLM countries (). A review was conducted of English-language literature published during 2017–2020 that included the keywords ‘preparedness’, ‘emergency preparedness’, ‘PHEOC’, ‘EOC’, ‘health emergency preparedness’, and international framework terms relevant to the TCLM countries, using public search engines including PubMed, Science Direct, Scopus, and Google Scholar. WHO/IHR Joint External Evaluation (JEE) reports for each country were reviewed, and other online reports were obtained through WHO mechanisms including the Public Health Emergency Operations Centre Network (PHEOC-NET), ASEAN mechanisms including ASEAN EOC Network newsletter and the ASEAN +3 Field Epidemiology Training Network (FETN), and the Mekong Basin Disease Surveillance (MBDS) network (East Asia, Citation2019; Mekong Basin Disease Surveillance, Citation2007). Additional information was obtained from presentations and meeting notes from the 2019 PHEOC-NET conference in Chiang Mai, Thailand, and MBDS cross-border network meetings (2017–2019) (East Asia, Citation2019).
Data from the desk review were collected using a standardised review form developed for this project. A working group systematically extracted content about policies, organisational structures, human resources, and key operational areas of PHEOCs, as well as information management, data-sharing, and cooperation between TCLM countries in response to public health threats.
For the second stage of the assessment, the study team developed a brief written questionnaire based on the WHO’s Checklist for Pandemic Influenza Risk and Impact Management and adapted the content to apply to COVID-19 (World Health Organization, Citation2018a). The questionnaire (see Supplemental Material) was sent to contacts in TCLM countries to assess national-level PHEOC operations, processes for international communication and coordination, and insights learned throughout the COVID-19 pandemic. A list of stakeholders to invite for participation was compiled from existing contacts within national PHEOCs, ministries of health, disease control units, international organisations, risk communication agencies, and other professional contacts identified during previous bilateral and multilateral meetings. Open-ended questions sought to solicit information on formal processes and procedures in communication between national PHEOCs, best practices and lessons learned in cross-border collaboration during the COVID-19 pandemic, and suggestions to improve international PHEOC coordination in the future. Participants were asked to provide responses that reflected the country’s PHEOC; questions were not designed to gauge individuals’ opinions or perspectives. Project coordinators invited participants to clarify responses or elaborate further in video calls as needed. Responses were compiled in aggregate at the country-level. Data were categorised to reflect internal PHEOC mechanisms, operations, and data sharing during the COVID-19 pandemic, strengths, and challenges in communication with other TCLM countries, and recommendations for regional coordination moving forward.
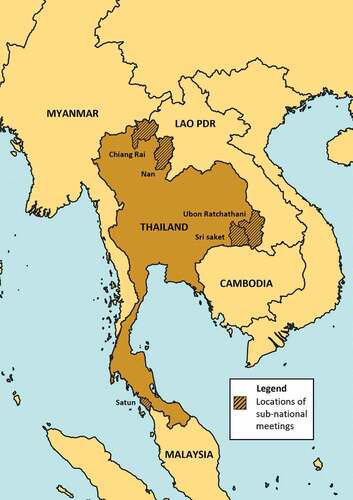
The third stage of the assessment evaluated cross-border coordination mechanisms at the sub-national level, between provincial PHEOCs in border provinces of Thailand and their counterparts in Cambodia, Lao PDR, and Malaysia. Five provinces were selected to host two-day meetings based on their location along border-areas where Thailand’s Ministry of Public Health supports GHSA activities (). Invitations to attend the meetings were sent to members of Provincial Communicable Disease Committees, and participants included public health officials, immigration and other governmental officers, and representatives from hospitals and universities in Thai border provinces. Project staff conducted meetings in each of the provinces during February-April 2021, during which sub-national officials in Thailand described their working relationships with counterparts across international borders in the context of public health emergencies including COVID-19. Participants discussed methods to improve coordination mechanisms, frameworks, and information sharing under existing Memorandums of Understanding (MOUs) during future disease outbreaks and public health events occurring in border regions. Guiding questions were used to standardise the information collected, and findings from each meeting were recorded in a common format (see Supplemental Material). Written summaries of each of the meetings were analysed to extract information regarding methods for sub-national PHEOC communication during emergencies, best practices and challenges encountered, and suggestions for the improvement of cross-border coordination. Extracted information from each of the border meetings was examined for commonalities.
Figure 1. The five provinces within Thailand that participated as sites to sub-national coordinating mechanisms along borders were Chiang Rai, Nan, Ubon Ratchathani, Sri Saket, and Satun.
A qualitative content analysis approach was applied to the three stages of the assessment to examine the frameworks, operations, communication structures, and interconnectivity of PHEOCs in TCLM countries, with a focus on international collaboration during the COVID-19 pandemic. Each country’s PHEOC capacity and operations were analysed at the national level using an adaptation of the WHO’s Strategic Framework for Emergency Preparedness (World Health Organization, Citation2017d). Findings from stages 1 and 2 of the assessment were used to describe strengths and gaps in each country’s emergency preparedness capacities. International communication and collaboration mechanisms between national- and sub-national-level PHEOCs were analysed based on findings from stages 2 and 3; strengths, best practices, gaps, and opportunities were identified. All stakeholders’ responses were considered, emphasising observations and suggestions that were common across multiple countries. Findings relating to international PHEOC coordination were disaggregated by country to provide insights into emergency communication across the TCLM region as a whole.
In Thailand, the project was considered as a monitoring and evaluation activity of PHEOC communication and coordination mechanisms amongst TCLM countries in light of the COVID-19 response. The project was reviewed and approved by the US Centers for Disease Control and Prevention, USA (CDC), and determined to be non-research.
Results
In the desk review (Stage 1), 76 articles and documents were screened. 28 documents met the study criteria, and 4 meeting reports and/or presentations were included in the detailed analysis.
The questionnaire (Stage 2) was circulated to 37 individuals in TCLM countries in February 2021, and 10 individuals returned questionnaires in the form of individual or pooled responses between March and September 2021 (27% response rate). Responses represented 3 individuals from Thailand, 1 from Cambodia, 3 from Lao PDR, and 3 from Malaysia, all from divisions or collaborations with each respective country’s Ministry of Health. All responses were included in the analysis.
Between February and April 2021, meetings among PHEOC staff and emergency response stakeholders took place in 5 border provinces of Thailand (Stage 3): Nan (73 participants), Chiang Rai (31 participants), Satun (83 participants), Ubon Ratchathani (47 participants), and Sri Saket (33 participants). Standardized notes from each meeting reflected best practices, challenges, and opportunities to improve sub-national PHEOC coordination in border areas.
National PHEOC structures, functions, and capacity: Results from desk review
The desk review provided information on PHEOC frameworks and operations in each of the countries. Thailand, Cambodia, Lao PDR, and Malaysia each has frameworks, plans, and mechanisms to support public health emergency preparedness, although the degree of preparedness and comprehensiveness of strategic plans varied between countries (). All TCLM countries have implemented PHEOCs at the country level under IHR (2005) and the Bi-Regional Technical Advisory Group on the Asia Pacific Strategy for Emerging Diseases and Public Health Emergencies-III (APSED-III) strategic framework (World Health Organization, Citation2017a). According to their JEEs, Malaysia and Thailand have fully staffed and permanent central PHEOC offices located within each respective Ministry of Health, with comprehensive information technology (IT) infrastructures to effectively manage data and communications (World Health Organization, Citation2017b, Citation2019). Malaysia has further invested in PHEOC staff and IT support since 2016, serving as the focal leader of the ASEAN EOC Network (EOC-Net Annual Meeting, Citation2019). Cambodia and Lao PDR both have established operational PHEOCs, but have inconsistent IT infrastructures to support emergency operations, as their reporting and surveillance systems rely on a combination of smartphone applications, paper-based systems, and web-based reports (World Health Organization, Citation2016, Citation2017c). To address this limitation, Cambodia developed a comprehensive master plan for a ‘Health Information System’, and Lao PDR has received project-based support from the Bill & Melinda Gates Foundation to enhance surveillance systems and PHEOC capacities (Asia Pacific Observatory on Health Systems and Policies, Citation2014; Bill & Melinda Gates Foundation, Citation2018). However, Cambodia’s national health workforce plan does not include public health professionals, and Lao PDR’s PHEOC does not have dedicated staff (Department of Planning and Health Information, Kingdom of Cambodia, Citation2016; World Health Organization, Citation2017c). (Bill & Melinda Gates Foundation, Citation2018), Training programs for response operations remain an ongoing need in both countries.
Table 2. Core elements of emergency preparedness at the national level, adapted from WHO strategic framework for emergency preparedness.
In the response to COVID-19, national plans were enacted in each country to strengthen pandemic response and coordination across sectors. In Thailand, the National Strategic Plan for Emerging Infectious Diseases (2017–2021), the Pandemic Influenza Preparedness Plan, and the activation of the Center for COVID-19 Situation Administration were utilised to guide the pandemic response and provide cross-sector collaboration (Bureau of Emerging Infectious Diseases, Citation2016; EOC-Net Annual Meeting, Citation2019). Malaysia employed an all-hazards approach in its national Crisis Preparedness and Response Center and used existing strategic plans to inform their COVID-19 response (Of Health Malaysia, Citation2017; EOC-Net Annual Meeting, Citation2019.). Cambodia and Lao PDR both have communicable disease decrees and have established a ‘One Health’ approach in their avian influenza prevention and response plans (EOC-Net Annual Meeting, Citation2019.), and both countries adapted these frameworks to apply to the COVID-19 pandemic.
Coordination mechanisms and information sharing between TCLM countries during COVID-19: Results from questionnaire responses
Questionnaire respondents reported that strong relationships among TCLM countries allowed cross-border coordination mechanisms to be mobilised quickly in the pandemic response. The ASEAN EOC Network provided a platform for discussions among TCLM countries to share control measures and lessons learned as the COVID-19 pandemic unfolded. A daily situation report was shared through the network to increase awareness of disease hotspots and best practices for containment. Malaysia’s PHEOC, as the lead country of the ASEAN EOC Network, organised online meetings monthly and on an ad-hoc basis. Video conferences with country PHEOCs and other regional partners were conducted to share information and discuss contact tracing, testing, isolation, and quarantine approaches. Additionally, several bilateral meetings were organised between Thailand and Lao PDR, as well as Thailand and Malaysia, to strengthen PHEOC coordination and cross-border response.
Questionnaire respondents in each of the TCLM countries reported that PHEOC coordination mechanisms were based on IHR (2005) protocol, with a National Focal Point (NFC) in each country serving as the primary point of contact to share information with other countries. However, respondents identified challenges in communication and information-sharing during the COVID-19 pandemic. Multiple country representatives reported that even with a known NFC in each country, it was at times difficult to determine the correct person to contact for specific requests, especially those requiring approval from higher levels within the government. With high staff turnover in several countries, contact lists for PHEOCs and other national disease control agencies were often outdated. Additionally, IT systems were not always interoperable between countries, so data sharing between NFCs commonly occurred through email or other informal channels. The lack of standardised communication methods between countries meant the timeline for information sharing was inconsistent, with requests for data critical to combatting the spread of COVID-19 sometimes taking a week or more to reach their destination. Informal communications, such as a WhatsApp group, helped to maintain communications between the countries, but respondents reported that the timely sharing of sensitive information remained a gap in cross-border coordination.
Sub-national-level PHEOC communication strategies: Results from border province meetings
Key strengths and challenges of cross-border communications at the sub-national level are shown in . While communications were less structured at lower administrative levels than the national level, channels of informal contact between border provinces were frequently utilised in disease control strategies. Stakeholders reported using social media (e.g. Line, Facebook, WhatsApp) to quickly communicate across borders. Several border regions conducted annual or semi-annual meetings to discuss diseases of concern and strategies to improve communication in situations such as when individuals cross borders to seek medical care, as is sometimes seen along the Lao PDR – Thailand border. While not all border provinces have local PHEOCs, participants from each border region in Thailand reported efforts to share information with neighbouring countries, in line with the existing MOUs. However, several regions noted inconsistencies in the sharing of sensitive information. For example, there is no mandate in the Thailand – Lao PDR MOU to share highly sensitive information at the sub-national level, and the need to obtain approvals from the national level complicated rapid communication across borders. Limited staff and financial resources at the local level hindered coordination in several border provinces, and differing IT mechanisms were a barrier to timely data sharing.
Table 3. Common strengths and challenges in cross-border communications identified from questionnaires and sub-national meetings.
In some border regions, staff were able to speak their cross-border counterpart’s language, thus, the use of a translator was not required. Language barriers had an impact on communications among some provinces in northern Thailand, where bordering countries relied on communicating in English or through the use of a translator. An example of strong sub-national coordination was identified at the Thailand – Malaysia border, where shared databases, SOPs, and communication in both Malay and English allowed for the rapid exchange of information and efficient coordination of control efforts. Consistent annual meetings between multiple provinces of Thailand and Malaysia provided up-to-date reviews of the effectiveness of disease control along border areas, as well as a space to discuss strategies for improvement. These observations are drawn from the information obtained from each of the study provinces, and do not necessarily reflect the entire landscape of each respective border region.
Technical capacity and emergency workforce support between countries
From border meetings at the sub-national level in Stage 3, gaps were reported in the knowledge of disease control and prevention, particularly in areas without strong local leadership. Limited epidemiologic knowledge led to delays in communications and coordination between border provinces in the pandemic response. High staff turnover complicated the consistent operations of TCLM emergency workforces. In some border regions, provincial leaders in Thailand reported that there were no sub-national PHEOC counterparts in cross-border provinces, so emergency response relied on directives from the national level and coordination with other key actors in disease containment, including local hospitals. Limited IT capacities and surveillance mechanisms in rural border areas further complicated efforts to control COVID-19, lessening the possibility for real-time information sharing between countries.
All three stages of the assessment identified that joint tabletop exercises have been conducted among TCLM countries to strengthen PHEOC capacity and improve epidemiologic knowledge. One such exercise, a virtual COVID-19 Table-Top Exercise conducted by the ASEAN Center for Military Medicine in May 2020, was designed to aid pandemic response, communication, and cooperation between civil and security sectors at the regional level (ASEAN Center of Military Medicine, Citation2020). Civilian and military actors from 10 ASEAN Member States (including TCLM countries) participated in the exercise, which was observed by the ASEAN Secretary, ASEAN Coordinating Centre for Humanitarian Assistance on disaster management, and representatives from Australia, China, India, Japan, New Zealand, Russia, and the USA. Other multi-national activities are being planned to improve PHEOC capacity in TCLM countries. For example, stakeholders in border meetings reported that Thailand will be supporting Lao PDR in conducting surveillance rapid response training and is developing bi-lingual e-learning exercises in epidemiology for Lao PDR PHEOC staff.
Recommendations from national and provincial stakeholders
Despite challenges identified in cross-border communications, all questionnaire respondents described strong relationships among TCLM countries and a willingness to collaborate on emergency responses. Stakeholders suggested several actions to improve PHEOC coordination at the national level. To address issues in timely communication across borders, questionnaire respondents recommended maintaining an updated list of contact persons for each country’s PHEOC, coordinating agencies, and establishing more than one NFC for each country’s PHEOC to handle varying requests for information. Respondents also suggested developing an official SOP or communication plan for emergencies, and standardising IT capacity and communication channels for information sharing across borders. To improve workforce capacity, several respondents recommended conducting cross-border training exercises for PHEOC staff. At the sub-national level in Stage 3, participants recommended creating a roster of interpreters to minimise language barriers at the local level, conducting additional trainings in epidemiology and knowledge of international frameworks for the emergency response workforce, and revising outdated MOUs.
Discussion
Strengthening PHEOC capacities and international coordination mechanisms is a priority of WHO and development partners (Association of Southeast Asian Nations Secretariat, Citation2020; Fernando, Citation2020; World Health Organization, Citation2005). The revision of the IHR in 2005 provided a mechanism to review, assess, and improve countries’ emergency preparedness and response through core capacity requirements, with the ability to identify strengths and weaknesses through annual reporting, after-action reviews, JEEs, and other external analyses (World Health Organization, Citation2005, Citation2018c). Significant improvements to global health security will likely come from reflections on the COVID-19 pandemic, which has reignited the need for a sharp focus on international coordination (Aavitsland et al., Citation2021; Blinken & Becerra, Citation2021; World Health Organization, Citation2021e). The pandemic brings to light challenges to both national and international response capacities and, in turn, provides an opportunity to examine areas for global improvement in emergency preparedness and response. Results from this assessment can help TCLM countries prioritise areas for improvement in emergency preparedness and inform the lead of the ASEAN EOC Network of considerations for strengthening health security in the region and preparing for future public health events of international concern.
This assessment found that each of the TCLM countries demonstrated a commitment to strengthening their national PHEOCs and improving cross-border communication in the face of the COVID-19 pandemic. In recent years, each country has taken steps towards improving emergency preparedness and PHEOC functions through national strategic plans, strengthening of surveillance and IT systems, and legislation, but the degree of preparedness varies between countries. Collectively, TCLM countries have frameworks in place to support international collaboration during public health emergencies, such as bilateral MOUs and the ASEAN EOC Network. Throughout the COVID-19 pandemic, these existing relationships were leveraged to activate a coordinated pandemic response, including the exchange of information across borders.
Despite commitments to improving emergency response capacities across TCLM countries, common challenges persisted throughout the pandemic response. Country representatives identified difficulties in timely information sharing at the national and sub-national levels, most often stemming from a time lag in receiving approval to share sensitive data, and a lack of standardised platforms for data-sharing between countries. Consistent communication channels and standardised data sharing procedures could improve coordination between TCLM countries during future public health emergencies; the need to address communication barriers at the national and sub-national levels is a key finding of this assessment. Based on reported gaps in achieving a coordinated international response, as well as recommendations from stakeholders, other efforts to address challenges should prioritise comprehensive training of PHEOC staff, limiting staff turnover, and the modernisation of surveillance and information-sharing mechanisms. Maintaining PHEOC preparedness with a properly trained workforce, integrity in data and information-sharing systems, and clear cross-border communication procedures can help TCLM countries strengthen their collective response to future international health threats.
In an interconnected world, effective communication among countries is essential for the early detection of health threats, as well as for understanding the scope of emergencies and mitigating the impacts of infectious diseases across borders. Strengthening international partnerships and communications is a priority for improving global health security, and developing quality information systems is critical to achieving more effective international coordination (Balajee et al., Citation2017; World Health Organization, Citation2005, Citation2018b). Digital communication and data-sharing challenges such as those identified in this analysis are not unique to TCLM countries; as the world transitions to digital health solutions, countries adopt systems that work best in the context of their own needs, but it can be challenging to integrate differing systems at the regional or global level. In its global strategy on digital health, the WHO has advocated for countries to integrate their surveillance and reporting technologies to be operable between countries, and to establish international agreements for data-sharing (World Health Organization, Citation2021a). As this analysis identified, data-sharing platforms were not consistent among TCLM countries. The development of IT system integrations and data-sharing agreements, perhaps through existing platforms such as the ASEAN EOC Network, could improve the timeliness of information exchange and support a coordinated response to future health threats. Revising MOUs between countries to better address international data-sharing needs during health emergencies, as well as collectively investing in an interoperable IT system for the secure exchange of information, would greatly improve PHEOC coordination among TCLM countries. The improvement of health data systems is crucial to the ability to share sensitive information quickly and securely across borders and will likely be one of the priorities for TCLM countries and the ASEAN region moving forward.
Health security cannot be effectively improved following COVID-19 without the sharing of successes and challenges encountered throughout the pandemic, as was done in TCLM countries through the ASEAN EOC Network and sub-national meetings in border regions. Conversations about lessons learned are equally important at the global level and are a key component of success in initiatives such as the GHSA (World Health Organization, Citation2018b). In response to gaps identified throughout the pandemic, the WHO has called for continued strengthening emergency response capacities, encouraging countries to improve surveillance and early warning systems to better prepare for future health threats (World Health Organization, Citation2021, Citation2022). Global actors have also been using the COVID-19 pandemic as an opportunity to re-examine the strengths and weaknesses of the IHR (2005) to craft suggestions to improve the framework. Several examinations of IHR (2005) functioning during the COVID-19 pandemic identified needs for intensified international coordination, improved data-sharing in response to health threats, effective engagement of NFCs across borders during the crisis response, and continued capacity-building and training of emergency response staff (Aavitsland et al., Citation2021; Blinken & Becerra, Citation2021; World Health Organization, Citation2021d). Our findings support the need for such improvements, as the same points were identified as weaknesses in COVID-19 response and coordination between TCLM countries. Global initiatives such as the WHO’s proposal to establish a Universal Health and Preparedness Review could assist in identifying resources and capacities needed to strengthen national and international preparedness for future health emergencies (World Health Organization, Citation2021c). Ongoing discussions and critical evaluations of COVID-19 response activities can help TCLM countries to improve emergency response capacities and prepare for health threats on the national, regional, and global scales.
Our analysis showed that TCLM countries have formed strong partnerships between PHEOCs and maintain a desire to address gaps in international coordination during public health emergencies. Initiatives at the regional level encourage countries to remain invested in global health security and can be leveraged to strengthen PHEOC coordination among TCLM countries. ASEAN Health Cluster 2 provides goals and frameworks that countries can use to build resilient health systems with the capacity to respond to health hazards and emerging health threats; these frameworks can serve as a tool for TCLM countries to address gaps in emergency preparedness capacities (ASEAN Health Cluster 2, Citation2017; Association of Southeast Asian Nations Secretariat, Citation2014). Through platforms such as the ASEAN EOC Network, ASEAN +3 Field Epidemiology Training Network, and the upcoming establishment of the ASEAN Centre for Public Health Emergencies and Emerging Diseases, TCLM countries and others in the region continue to remain actively involved in building capacity to prevent, detect, and respond to public health threats in a collaborative nature (, Association of Southeast Asian Nations Secretariat, Citation2022; Association of Southeast Asian Nations, Citation2022; Fernando, Citation2020). APSED-III, which our analysis found has been used to guide COVID-19 response operations in TCLM countries, provides a strategic framework for the Asia Pacific region to strengthen the core capacities required under IHR (2005), and emphasises the importance of partnerships and inter-connectivity of information systems at the regional level (World Health Organization Regional Office for the Western Pacific, Citation2017). Other regional guidelines, including the 2021–2025 work program for the ASEAN Agreement on Disaster Management and Emergency Response (AADMER) and the Information and Communications Technology Roadmap on Disaster Management for 2025 and Beyond, call for countries to enhance emergency response capacities by conducting regular emergency preparedness drills and exercises, further developing international telecommunications networks and data-sharing agreements, and advancing the interoperability of EOC information systems (Association of Southeast Asian Nations Secretariat, Citation2020; Centre, Citation2019). These recommendations directly correspond to our findings, as all were mentioned by stakeholders in stages 2 and 3 of the assessment as potential ways forward to improve international coordination between PHEOCs in TCLM countries.
Through WHO platforms, the Southeast Asia region has committed to strengthening health systems and improving global health security using lessons learned from the pandemic (East Asia, Citation2019; WHO Regional Office for South, Citation2021). To further improve public health emergency response, TCLM countries can utilise initiatives developed by the WHO for the Southeast Asian region. WHO working groups have been established in Southeast Asia to facilitate the improvement of the region’s implementation of the Global Outbreak Alert and Response Network (GOARN). Discussions are underway outlining tactics to improve regional response to health emergencies through GOARN, which could include regional policies and training to address key gaps in outbreak response (World Health Organization, Citation2021, Citation2021, Citation2021). A coordinated approach to improving public health notifications and response across borders could address gaps identified in this assessment regarding timely communication and emergency workforce capacities; TCLM countries should consider remaining actively involved in the implementation of regional initiatives. In addition to staying up to date on JEEs, countries could take advantage of opportunities to form collaborative initiatives with the WHO to identify additional areas for improvement in national and regional emergency response capacities. For example, Thailand became one of the first countries to implement the Joint Intra-Action Review with the WHO in July 2020. This tool helped identify the strengths and vulnerabilities of the national COVID-19 response, which included the need to enhance coordination, improve surveillance, and strengthen the workforce (World Health Organization, Citation2020). A COVID-19 Intra-Action Review has subsequently been conducted in Lao PDR, and another is planned for Cambodia (World Health Organization, Citation2022b). Ongoing assessments of PHEOC response, particularly relating to COVID-19, can provide TCLM countries with valuable insights into the strengths and weaknesses of their emergency response capacities and leave the Southeast Asia region better equipped to prevent, detect, and respond to future public health threats.
This project had several limitations. First, the assessment was initiated and led by Thailand and therefore contains more complete information for Thailand than for other countries. The meetings in border provinces during the third stage, for instance, were conducted among key sub-national actors in Thailand and did not reflect the perspectives of cross-border counterparts. Results from this work may inform the development of future independent assessments conducted by external partners. Second, the amount of in-depth information provided in response to the questionnaire varied between countries. There was a relatively low overall response rate, lacking responses from several key government and development partners in each country. Several factors may have influenced the low response rate, including competing priorities to respond to the immediate COVID-19 situation and submitting pooled responses (i.e. completing the form as a group rather than as individuals). As a result, the findings may not fully reflect communication procedures used by national PHEOCs to coordinate with other countries during the COVID-19 pandemic. Third, the literature review was limited to English-language documentation, which may not be fully representative of the current policy and organisational landscape in each respective country. Fourth, findings regarding COVID-19 from the questionnaire responses and meetings in border provinces represent a snapshot in time during the pandemic and were not able to capture changes to international coordination as the COVID-19 response continued to unfold. Finally, this analysis did not use a validated tool for assessing PHEOCs, and instead relied on input from literature, meetings, and public health officials in each of the countries. Future external evaluations may be able to build upon the findings of this assessment and further evaluate PHEOC coordination during the COVID-19 pandemic. Future studies may also choose to expand the assessment to other countries in the Southeast Asia region.
Conclusion
Priorities for the TCLM region to improve the inter-connectedness of PHEOCs following this assessment could include commitments towards developing interoperable IT systems and cross-border communication channels; the development of SOPs for timely information sharing across borders; and expansion of regional trainings for PHEOC staff in emergency response, epidemiology, and data-sharing procedures. A continued focus on strengthening these capacities in the post-pandemic era will benefit the region’s health security in the long run and help to activate a coordinated response to future health threats. The COVID-19 pandemic has proven that strengthening global health security is not a passive endeavour; countries can continually work together to address gaps in emergency preparedness and response. This assessment, in line with WHO recommendations, provides TCLM countries with the opportunity to address weaknesses in national and international PHEOC capacities, in order to prepare the region for a stronger response to future global and regional health emergencies.
Supplemental Material
Download Zip (17.1 KB)Acknowledgments
We would like to thank representatives from Cambodia, Lao PDR, Malaysia, and Thailand for their participation in the questionnaires. We would also like to thank Wanicha Phoophoritham (Thailand MOPH — US CDC Collaboration) for her contributions to sub-national assessments and Samart Karuchit (Thailand MOPH – US CDC Collaboration) for his assistance in developing graphics.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/23779497.2023.2216267
Additional information
Funding
Notes on contributors
Royce Tsukayama
Royce Tsukayama Royce Tsukayama completed a Master’s in Public Health with a focus in Infectious Diseases at the University of California, Berkeley and has been working as a Technical Coordinator at the Department of Disease Control, Ministry of Public Health, Thailand since 2018, primarily focusing on improving regional and global health security capacities through mechanisms such as the GHSA.
Natalie Wodniak
Natalie Wodniak Natalie Wodniak, MPH is a Global Epidemiology Fellow with the Division of Global Health Protection within the CDC-Thailand office. She supports several laboratory-enhanced epidemiologic studies throughout Thailand, focusing on emerging and re-emerging infectious diseases, and works to strengthen global health security within the Southeast Asia region.
Soawapak Hinjoy
Soawapak Hinjoy Soawapak Hinjoy (DVM, MSc, MPH, DrPH) has a background in veterinary medicine. After graduating with a doctorate in Public Health, she currently holds the position of Director of Office of International Cooperation, Department of Disease Control, Ministry of Public Health. She is enthusiastic about developing collaborations in public health research on zoonotic diseases, emerging and re-emerging infectious under a conceptual One Health concept in Thailand and at the international level. She also serves as national coordinator of ASEAN Health Cluster 2 and MBDS network, developing effective public health control and prevention strategies with a perspective of global health security.
Charatdao Bunthi
Charatdao Bunthi Charatdao Bunthi, MD, MPH is a medical epidemiologist with the Division of Global Health Protection within the CDC-Thailand office. Dr. Bunthi works with Thailand ministerial, US government, and international development partners to address public health threats in Thailand and Southeast Asia. Dr. Bunthi has supported national, sub-national and regional efforts to promote global health security through strengthening public health emergency management systems in Thailand and neighboring countries within the region.
Pasakorn Akarasewi
Pasakorn Akarasewi Pasakorn Akarasewi (MD. Cert. FETP, Thai Board of Preventive Medicine, Retired) has vast experiences in public health services in Thailand. He served as a rural doctor, director of a public hospital, Director of TB Division/National TB program manager, and Director of the Bureau of Epidemiology, Department of Disease Control. He gained vast experiences in international public health while working on national TB, Global Fund management, and as National Focal Point for the International Health Regulations. He has been interested in developing collaborations in One Health, multi-sector collaboration, global health security, public health surveillance on emerging diseases, and emergency response for infectious diseases. Currently, he is member of ASEAN Field Epidemiology Training Network - FETN, and is a senior consultant of the Department of Disease Control, Ministry of Public Health. In addition, he has experience in and is enthusiastic about teaching and applying Python and Ruby to public health information and data management.
Walaiporn Jiaranairungroj
Walaiporn Jiaranairungroj Ms. Walaiporn Jiaranairungroj graduated with a Bachelor’s Degree in Medical Sciences followed by a Master of Business Administration. She formerly worked as a medical scientist and project coordinator at the Department of Medical Sciences, Ministry of Public Health, Thailand. Her current position is a project manager at the Office of International Cooperation, Department of Disease Control. Her professional interests include working and collaborating with international organizations and other stakeholder organizations who conduct field work and training workshops related to field epidemiology, disease prevention and control, and laboratory diagnosis.
Wannaporn Pueyo
Wannaporn Pueyo Wannaporn Pueyo (BSc. Public Health) has a background in public health that includes serving as a public health technical officer in a private hospital, and currently is a staff member of the Office of International Cooperation, Department of Disease Control, Ministry of Public Health, Thailand. Her roles include developing policies and strategies on disease prevention and control, developing capacity under the Public Sector Management Quality Award (PMQA), and developing the communicable disease curriculum for the global One Health approach.
Wattana Masunglong
Wattana Masunglong is the Foreign Relations Officer, Professional Level of the Office of International Cooperation, Department of Disease Control, Thailand. He is the focal point responsible for the Global and ASEAN Health Cooperation. He has worked and coordinated closely with the WHO and a wide range of international organizations to exchange and share disease control information and global health protocols. Apart from the aforementioned key roles, he is also the script maker, translator, and rapporteur for the High-Level Executives of the Department of Disease Control.
Pitchapa Kleblumjeak
Pitchapa Kleblumjeak Pitchapa Kleblumjeak earned a Bachelor’s degree from Kasetsart University. She previously served as a Policy and Plan Analyst at Office of the Narcotics Control Board and also held an international relations position at the Gemologist Institute. She currently works as a Foreign Relations Officer, focusing on supporting international cooperation and collaborating with international institutions on disease prevention and control.
John R. MacArthur
John R. MacArthur John R. MacArthur, MD, MPH is the Regional Director of the CDC Southeast Asia Regional Office and formally the Country Director for CDC Thailand. Dr. MacArthur works with governments and other partners throughout the Southeast Asia region to strengthen their core health security capacities including workforce development, surveillance, laboratory systems, One Health, and public health emergency management.
Emily Bloss
Emily Bloss Emily Bloss, PhD is an Epidemiologist with the Division of Global Health Protection within the CDC-Thailand office, where she works with foreign ministerial, US government, and international development partners to address the threat of emerging infectious diseases in Thailand and Southeast Asia. Focusing on public health emergencies, strengthening surveillance, and implementing multidisciplinary approaches to disease detection and response, Dr Bloss has supported national and regional efforts to promote global health security by strengthening capacity to prevent, detect and respond to health threats.
References
- EOC-Net Annual Meeting. (2019). Chiang Mai, Thailand. World Health Organization.
- Aavitsland, P., Aguilera, X., Al-Abri, S. S., Amani, V., Aramburu, C. C., Attia, T. A., Blumberg, L. H., Chittaganpitch, M., Le Duc, J. W., Li, D., Mokhtariazad, T., Moussif, M., Ojo, O. E., Okwo-Bele, J. -M., Saito, T., Sall, A. A., Salter, M. W., Sohn, M., & Wieler, L. H. Functioning of the international health regulations during the COVID-19 pandemic. The Lancet, 398(10308), 1283–1286. 9 October. 2021. https://doi.org/10.1016/S0140-6736(21)01911-5
- ASEAN Center of Military Medicine. (2020). ADMM COVID-19 table-top exercise for ASEAN countries plus China, Korea, Australia, Russia, and the USA. ASEAN Center of Military Medicine.
- ASEAN Health Cluster 2. (2017). ASEAN health cluster 2: Responding to all hazards and emerging threats. ASEAN Secretariat.
- ASEAN Secretariat. (2022). Association of Southeast Asian Nations. In Joint Statement: 15th ASEAN health ministers meeting (pp. 5). Jakarta.
- Asia Pacific Observatory on Health Systems and Policies. (2014). The lao people’s democratic republic health system review. Health Systems in Transition, 4(1), 75–90.
- Association of Southeast Asian Nations Secretariat, “ASEAN Emergency Operations Center (EOC) Network for Public Health,” [Online]. Available: https://aseanphe.org/phe-mechanism/asean-emergency-operation-centre-asean-eoc-network/. [Retrieved March 3, 2022].
- Association of Southeast Asian Nations Secretariat. (2014). ASEAN health cluster 2 work programme for 2016 to 2020. ASEAN.
- Association of Southeast Asian Nations Secretariat. (2020). AADMER work programme: 2021-2025. ASEAN.
- Association of Southeast Asian Nations Secretariat, “ASEAN+3 field epidemiology training network (ASEAN+3 FETN),” 2020. [Online]. Available: https://aseanphe.org/phe-mechanism/asean3-field-epidemiology-training-network-asean3-fetn/. [Retrieved March 3, 2022].
- Balajee, S. A., Pasi, O. G., Etoundi, A. G. M., Rzeszotarski, P., Do, T. T., Hennessee, I., Merali, S., Alroy, K. A., Phu, T. D., & Mounts, A. W. (2017). Sustainable model for public health emergency operations centers for global settings. Emerging Infectious Diseases, 23(Suppl 1), S190–195. https://doi.org/10.3201/eid2313.170435
- Bill & Melinda Gates Foundation. (2018). Lao PDR emergency operations center planning and design mission. https://www.gatesfoundation.org/~/media/GFO/Documents/How-We-Work/RFP-Lao-PDR-EOC/Lao-PDR-EOC-Planning-and-Design-Mission-Report.pdf?la=en
- Blinken, A. J., & Becerra, X. Strengthening global health security and reforming the international health regulations: Making the world safer from future pandemics. JAMA, 326(13), 1255–1256. 5 October. 2021. https://doi.org/10.1001/jama.2021.15611
- Bureau of Emerging Infectious Diseases. (2016). Thailand national strategic plan for emerging infectious diseases: 2017-2021 (pp. 8). (Department of Disease Control, Ministry of Public Health.
- Centre, A. H. A. (2019). ICT roadmap on disaster management for 2025 and beyond. AHA Centre.
- Corwin, A., Plipat, T., Phetsouvanh, R., Mayxay, M., Xangsayarath, P., Mai, L. T. Q., Oum, S., & Kuddus, M. A. The impact of preparedness in defying COVID-19 pandemic expectations in the lower Mekong region: A Case Study. American Journal of Tropical Medicine & Hygiene, 104(4), 1519–1525. 18 January. 2021. https://doi.org/10.4269/ajtmh.20-1499
- Department of Planning and Health Information, Kingdom of Cambodia, “Health Strategic Plan 2016-2020,” 2016.
- Fernando, F. M. (2020). ASEAN Center for Public Health Emergencies and Emerging Diseases (ACPHEED) The ASEAN Stronger Health Systems, Our Lifeline in a Pandemic, Special Edition, 14–15.
- Hinjoy, S., Tsukayama, R., Chuxnum, T., Masunglong, W., Sidet, C., Kleeblumjeak, P., Onsai, N., & Iamsirithaworn, S. (2020, July). Self-assessment of the Thai Department of Disease Control’s communication for international response to COVID-19 in the early phase. International Journal of Infectious Diseases, 96, 205–210. https://doi.org/10.1016/j.ijid.2020.04.042
- Mekong Basin Disease Surveillance, 2007. [Online]. Available: https://mbdsnet.org/.
- Of Health Malaysia, M. (2017). Malaysia Strategy for Emerging Infectious Diseases and Public Health Emergencies (MYSED) Work Plan, 2017-2021. Ministry of Health Malaysia, Kuala Lumpur, 1–33.
- US Centers for Disease Control and Prevention. (2014). Global Health Security Agenda: GHSA Emergency Operations Centers Action Package (GHSA Action Package Respond-1). US CDC.
- WHO Regional Office for South-East Asia, “WHO South-East Asia countries resolve to reorient and strengthen health systems,” 7 September. 2021. [Online]. Available: https://www.who.int/southeastasia/news/detail/07-09-2021-who-south-east-asia-countries-resolve-to-reorient-and-strengthen-health-systems. [Accessed 10 February 2022].
- WHO Regional Office for South-East Asia. (2019). Five-Year regional strategic plan to strengthen public health preparedness and Response: 2019-2023. World Health Organization.
- WHO Regional Office for South-East Asia. (2020). 2019 novel coronavirus (2019-nCov) strategic preparedness and response plan for the South-East Asia Region. World Health Organization.
- World Health Organization. (2005). International Health Regulations: Third Edition, .
- World Health Organization. (2014). A systematic review of public health Emergency Operations Centres (EOC).
- World Health Organization. (2015). Framework for a public health emergency operations centre.
- World Health Organization. (2016). Joint external evaluation of IHR core capacities of the Kingdom of Cambodia. World Health Organization, Geneva, 22–33.
- World Health Organization. (2017a). Asia Pacific strategy for emerging diseases and public health emergencies: Advancing implementation of the international health regulations (2005).
- World Health Organization. (2017b). Joint external evaluation of IHR core capacities of the Kingdom of Thailand.
- World Health Organization. (2017c). Joint external evaluation of IHR core capacities of the Lao People’s Democratic Republic.
- World Health Organization. (2017d). A strategic framework for emergency preparedness.
- World Health Organization. (2018a). A checklist for pandemic influenza risk and impact management: Building capacity for pandemic response.
- World Health Organization. (2018b). Global Health Security Agenda (GHSA) 2024 Framework.
- World Health Organization. (2018c). International health regulations (2005) monitoring and evaluation framework.
- World Health Organization. (2019). Joint external evaluation of IHR core capacities of Malaysia. World Health Organization, Geneva, 42–55.
- World Health Organization. (2020). Joint intra-action review of the public health response to COVID-19 in Thailand.
- World Health Organization. (2021). Statement on the sixth meeting of the international health regulations (2005) Emergency Committee regarding the coronavirus disease (COVID-19) pandemic. WHO.
- World Health Organization. (2021). Terms of reference (as of 14 July 2021): Governance working group (WG1). In Global Oubreak and Alert Response Network. WHO.
- World Health Organization. (2021). Terms of reference (as of 14 July 2021): HR surge working group (WG2). In Global Oubreak and Alert Response Network. WHO.
- World Health Organization. (2021). Terms of reference (as of 14 July 2021): Operational research working group (WG3). In Global Oubreak and Alert Response Network. WHO.
- World Health Organization. (2021a). Global strategy on digital health: 2020-2025.
- World Health Organization. (2021c). Universal Health and Preparedness Review (UHPR): Member states information session.
- World Health Organization, “Building health systems resilience for universal health coverage and health security during the COVID-19 pandemic and beyond: WHO position paper,”, 2021d.
- World Health Organization, “Report of the review committee on the functioning of the International Health Regulations (2005) during the COVID-19 response,”, 2021e.
- World Health Organization. (2022). Statement on the tenth meeting of the international health regulations (2005) emergency committee regarding the coronavirus disease (COVID-19) pandemic. WHO.
- World Health Organization, “Intra-Action Review (IAR),” World Health Organization, 2022b. [Online]. Available: https://extranet.who.int/sph/intra-action-review. [Retrieved July 4, 2022].
- World Health Organization Regional Office for South-East Asia, “Annual meeting 2019: Public Health Emergency Operations Centres Network (EOC-NET),” 23–25 September. 2019. [Online]. Available: https://www.who.int/southeastasia/news/events/detail/2019/09/23/default-calendar/annual-meeting-2019-public-health-emergency-operations-centres-network-eoc-net. [Retrieved November 2, 2021].
- World Health Organization Regional Office for the Western Pacific. (2017). Asia Pacific Strategy for Emerging Diseases and Public Health Emergencies: Advancing implementation of the international health regulations (2005). World Health Organization.

